Zoonotic Pathogens of Peri-Domestic Rodents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evolutionary Biology of the Genus Rattus: Profile of an Archetypal Rodent Pest
Bromadiolone resistance does not respond to absence of anticoagulants in experimental populations of Norway rats. Heiberg, A.C.; Leirs, H.; Siegismund, Hans Redlef Published in: <em>Rats, Mice and People: Rodent Biology and Management</em> Publication date: 2003 Document version Publisher's PDF, also known as Version of record Citation for published version (APA): Heiberg, A. C., Leirs, H., & Siegismund, H. R. (2003). Bromadiolone resistance does not respond to absence of anticoagulants in experimental populations of Norway rats. In G. R. Singleton, L. A. Hinds, C. J. Krebs, & D. M. Spratt (Eds.), Rats, Mice and People: Rodent Biology and Management (Vol. 96, pp. 461-464). Download date: 27. Sep. 2021 SYMPOSIUM 7: MANAGEMENT—URBAN RODENTS AND RODENTICIDE RESISTANCE This file forms part of ACIAR Monograph 96, Rats, mice and people: rodent biology and management. The other parts of Monograph 96 can be downloaded from <www.aciar.gov.au>. © Australian Centre for International Agricultural Research 2003 Grant R. Singleton, Lyn A. Hinds, Charles J. Krebs and Dave M. Spratt, 2003. Rats, mice and people: rodent biology and management. ACIAR Monograph No. 96, 564p. ISBN 1 86320 357 5 [electronic version] ISSN 1447-090X [electronic version] Technical editing and production by Clarus Design, Canberra 431 Ecological perspectives on the management of commensal rodents David P. Cowan, Roger J. Quy* and Mark S. Lambert Central Science Laboratory, Sand Hutton, York YO41 1LZ, UNITED KINGDOM *Corresponding author, email: [email protected] Abstract. The need to control Norway rats in the United Kingdom has led to heavy reliance on rodenticides, particu- larly because alternative methods do not reduce rat numbers as quickly or as efficiently. -

Review of the Hylomyscus Denniae Group (Rodentia: Muridae) in Eastern Africa, with Comments on the Generic Allocation of Epimys Endorobae Heller
PROCEEDINGS OF THE BIOLOGICAL SOCIETY OF WASHINGTON 119(2):293–325. 2006. Review of the Hylomyscus denniae group (Rodentia: Muridae) in eastern Africa, with comments on the generic allocation of Epimys endorobae Heller Michael D. Carleton, Julian C. Kerbis Peterhans, and William T. Stanley (MDC) Department of Vertebrate Zoology, National Museum of Natural History, Smithsonian Institution, Washington, D.C. 20560-0108, U.S.A., e-mail: [email protected]; (JKP) University College, Roosevelt University, Chicago, Illinois 60605, U.S.A.; Department of Zoology, Division of Mammals, The Field Museum of Natural History, Chicago, Illinois 60605, U.S.A., e-mail: [email protected]; (WTS) Department of Zoology, Division of Mammals, The Field Museum of Natural History, Chicago, Illinois 60605, U.S.A., e-mail: [email protected] Abstract.—The status and distribution of eastern African populations currently assigned to Hylomyscus denniae are reviewed based on morpho- logical and morphometric comparisons. Three species are considered valid, each confined largely to wet montane forest above 2000 meters: H. denniae (Thomas, 1906) proper from the Ruwenzori Mountains in the northern Albertine Rift (west-central Uganda and contiguous D. R. Congo); H. vulcanorum Lo¨nnberg & Gyldenstolpe, 1925 from mountains in the central Albertine Rift (southwestern Uganda, easternmost D. R. Congo, Rwanda, and Burundi); and H. endorobae (Heller, 1910) from mountains bounding the Gregory Rift Valley (west-central Kenya). Although endorobae has been interpreted as a small form of Praomys, additional data are presented that reinforce its membership within Hylomyscus and that clarify the status of Hylomyscus and Praomys as distinct genus-group taxa. The 12 species of Hylomyscus now currently recognized are provisionally arranged in six species groups (H. -

Genetic Identification of Freely Traded Synanthropic Invasive Murid Rodents in Pet Shops in Gauteng Province, South Africa
African Zoology ISSN: 1562-7020 (Print) 2224-073X (Online) Journal homepage: https://www.tandfonline.com/loi/tafz20 Genetic identification of freely traded synanthropic invasive murid rodents in pet shops in Gauteng Province, South Africa Ndivhuwo Maligana, Rolanda S Julius, Tinyiko C Shivambu & Christian T Chimimba To cite this article: Ndivhuwo Maligana, Rolanda S Julius, Tinyiko C Shivambu & Christian T Chimimba (2020) Genetic identification of freely traded synanthropic invasive murid rodents in pet shops in Gauteng Province, South Africa, African Zoology, 55:2, 149-154, DOI: 10.1080/15627020.2019.1704632 To link to this article: https://doi.org/10.1080/15627020.2019.1704632 Published online: 02 Jun 2020. Submit your article to this journal Article views: 18 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=tafz20 African Zoology 2020, 55(2): 149–154 Copyright © Zoological Society Printed in South Africa — All rights reserved of Southern Africa AFRICAN ZOOLOGY ISSN 1562-7020 EISSN 2224-073X https://doi.org/10.1080/15627020.2019.1704632 Short Communication Genetic identification of freely traded synanthropic invasive murid rodents in pet shops in Gauteng Province, South Africa Ndivhuwo Maligana* , Rolanda S Julius , Tinyiko C Shivambu and Christian T Chimimba DSI-NRF Centre of Excellence for Invasion Biology and Mammal Research Institute, University of Pretoria, South Africa *Correspondence: [email protected] Although synanthropic invasive murid rodents are freely traded in pet shops in South Africa, their taxonomic identities, however, remain largely unknown. Twenty-four murid rodents were sampled from pet shops in four of the five municipalities in Gauteng Province, South Africa for genetic identification using mitochondrial cytochrome b (mtDNA) sequence data. -

Quaternary Murid Rodents of Timor Part I: New Material of Coryphomys Buehleri Schaub, 1937, and Description of a Second Species of the Genus
QUATERNARY MURID RODENTS OF TIMOR PART I: NEW MATERIAL OF CORYPHOMYS BUEHLERI SCHAUB, 1937, AND DESCRIPTION OF A SECOND SPECIES OF THE GENUS K. P. APLIN Australian National Wildlife Collection, CSIRO Division of Sustainable Ecosystems, Canberra and Division of Vertebrate Zoology (Mammalogy) American Museum of Natural History ([email protected]) K. M. HELGEN Department of Vertebrate Zoology National Museum of Natural History Smithsonian Institution, Washington and Division of Vertebrate Zoology (Mammalogy) American Museum of Natural History ([email protected]) BULLETIN OF THE AMERICAN MUSEUM OF NATURAL HISTORY Number 341, 80 pp., 21 figures, 4 tables Issued July 21, 2010 Copyright E American Museum of Natural History 2010 ISSN 0003-0090 CONTENTS Abstract.......................................................... 3 Introduction . ...................................................... 3 The environmental context ........................................... 5 Materialsandmethods.............................................. 7 Systematics....................................................... 11 Coryphomys Schaub, 1937 ........................................... 11 Coryphomys buehleri Schaub, 1937 . ................................... 12 Extended description of Coryphomys buehleri............................ 12 Coryphomys musseri, sp.nov.......................................... 25 Description.................................................... 26 Coryphomys, sp.indet.............................................. 34 Discussion . .................................................... -

Taxonomic Tapestries the Threads of Evolutionary, Behavioural and Conservation Research
Taxonomic Tapestries The Threads of Evolutionary, Behavioural and Conservation Research Taxonomic Tapestries The Threads of Evolutionary, Behavioural and Conservation Research Edited by Alison M Behie and Marc F Oxenham Chapters written in honour of Professor Colin P Groves Published by ANU Press The Australian National University Acton ACT 2601, Australia Email: [email protected] This title is also available online at http://press.anu.edu.au National Library of Australia Cataloguing-in-Publication entry Title: Taxonomic tapestries : the threads of evolutionary, behavioural and conservation research / Alison M Behie and Marc F Oxenham, editors. ISBN: 9781925022360 (paperback) 9781925022377 (ebook) Subjects: Biology--Classification. Biology--Philosophy. Human ecology--Research. Coexistence of species--Research. Evolution (Biology)--Research. Taxonomists. Other Creators/Contributors: Behie, Alison M., editor. Oxenham, Marc F., editor. Dewey Number: 578.012 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying or otherwise, without the prior permission of the publisher. Cover design and layout by ANU Press Cover photograph courtesy of Hajarimanitra Rambeloarivony Printed by Griffin Press This edition © 2015 ANU Press Contents List of Contributors . .vii List of Figures and Tables . ix PART I 1. The Groves effect: 50 years of influence on behaviour, evolution and conservation research . 3 Alison M Behie and Marc F Oxenham PART II 2 . Characterisation of the endemic Sulawesi Lenomys meyeri (Muridae, Murinae) and the description of a new species of Lenomys . 13 Guy G Musser 3 . Gibbons and hominoid ancestry . 51 Peter Andrews and Richard J Johnson 4 . -

Javan Rhino Expedition
Javan Rhino Expedition th th Destination: Java, Indonesia Duration: 10 Days Dates: 7 – 16 June 2018 Having amazing close encounters with 2 different Javan Rhinos in just one day! Enjoying the expertise of some of Ujung Kulon’s finest guides & rangers Great sightings of various kingfishers and heron species along the rivers Trekking & camping deep inside the core zone of Ujung Kulon National Park Finding very fresh evidence of at least 2 different rhinos from when we were there Seeing over 50 species of birds throughout including Green Peafowl & Elegant Pitta Spotlighing banteng, Sunda leopard cat & Javan mousedeer along the river banks Canoeing down the river where more Javan rhinos have been seen than anywhere Coming across a beautiful neonate Malayan pit viper along one of the trails Enjoying speed boat transfers around the stunning coastline of Ujung Kulon NP Tour Leader / Guides Overview Martin Royle (Royle Safaris Tour Leader) Chinglus (Lead Ujung Kulon Guide) Meeta & Udung (Ujung Kulon Rangers) Day 1: Jakarta / Adun, Geni, Wilum, Bambu, Wilf, Nurlin, Asif (Porters) Carita / Edy (Transfer driver) Ujung Kulon Ciggaman (Boat transfer skipper) Participants Days 2-8: Ujung Kulon Dr. Jacoba Brinkman Mr. Phillip DuCros Mr. Andrew Holman Mrs. Paula Holman Day 9: Ujung Kulon / Handeleum Island Day 10: Carita / Jakarta Day 11: Home Royle Safaris – 6 Greenhythe Rd, Heald Green, Cheshire, SK8 3NS – 0845 226 8259 – [email protected] Day by Day Breakdown Overview With only five species of rhinos in the world you would think that everyone would know about all five, there are not that many. But there are two that largely go unnoticed. -
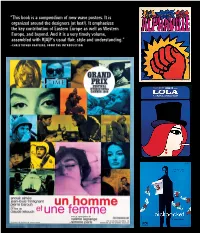
This Book Is a Compendium of New Wave Posters. It Is Organized Around the Designers (At Last!)
“This book is a compendium of new wave posters. It is organized around the designers (at last!). It emphasizes the key contribution of Eastern Europe as well as Western Europe, and beyond. And it is a very timely volume, assembled with R|A|P’s usual flair, style and understanding.” –CHRISTOPHER FRAYLING, FROM THE INTRODUCTION 2 artbook.com French New Wave A Revolution in Design Edited by Tony Nourmand. Introduction by Christopher Frayling. The French New Wave of the 1950s and 1960s is one of the most important movements in the history of film. Its fresh energy and vision changed the cinematic landscape, and its style has had a seminal impact on pop culture. The poster artists tasked with selling these Nouvelle Vague films to the masses—in France and internationally—helped to create this style, and in so doing found themselves at the forefront of a revolution in art, graphic design and photography. French New Wave: A Revolution in Design celebrates explosive and groundbreaking poster art that accompanied French New Wave films like The 400 Blows (1959), Jules and Jim (1962) and The Umbrellas of Cherbourg (1964). Featuring posters from over 20 countries, the imagery is accompanied by biographies on more than 100 artists, photographers and designers involved—the first time many of those responsible for promoting and portraying this movement have been properly recognized. This publication spotlights the poster designers who worked alongside directors, cinematographers and actors to define the look of the French New Wave. Artists presented in this volume include Jean-Michel Folon, Boris Grinsson, Waldemar Świerzy, Christian Broutin, Tomasz Rumiński, Hans Hillman, Georges Allard, René Ferracci, Bruno Rehak, Zdeněk Ziegler, Miroslav Vystrcil, Peter Strausfeld, Maciej Hibner, Andrzej Krajewski, Maciej Zbikowski, Josef Vylet’al, Sandro Simeoni, Averardo Ciriello, Marcello Colizzi and many more. -

Distribution of Native and Non-Native Rats (Rattus Spp.) Along an Elevational Gradient in a Tropical Rainforest of Southern Luzon, Philippines
ECOTROPICA 14: 129–136, 2008 © Society for Tropical Ecology DISTRIBUTION OF NATIVE AND NON-NATIVE RATS (RATTUS SPP.) ALONG AN ELEVATIONAL GRADIENT IN A TROPICAL RAINFOREST OF SOUTHERN LUZON, PHILIPPINES Cristina C. Salibay & Hazel Anne V. Luyon De La Salle University-Dasmariñas, Dasmariñas, Cavite, Philippines Abstract. Rats (Muridae) of the genus Rattus occur in the Philippines, both as native and as invasive species. While the invasive species are well known to use a large range of anthropogenic habitats, little is known about their potential to occur in forest areas. We studied the occurrence and relative abundance of different species of Rattus in forests along elevational gradients on three mountains within the Palay-palay / Mataas na Gulod National Park in Southern Luzon, Philippines. Four Rattus species were collected and their occurrence and relative abundance were found to differ significantly between species and along elevational gradients. Rattus norvegicus (40.3% of captures), R. tanezumi (21.5%), and R. argentiventer (5.6%) are invasive species and R. everetti (32.7%) a native forest-inhabiting species. While the three invasive species were most abundant at low elevations, R. everetti was most abundant at higher elevations. The number of invasive rats has been attributed to their survival and adaptation at lower elevations, where habitat conversion and degradation are most intense, while native species are more common at higher elevations where habitat is relatively un- disturbed. Key words: elevation, forest species, invasive species, Philippines, rainforest, Rattus species. INTRODUCTION and occur at high abundances in local mammal as- semblages (Heaney et al. 1998, Steppan et al. 2003). -

Comparative Phylogeography, Phylogenetics, and Population Genomics of East African Montane Small Mammals
City University of New York (CUNY) CUNY Academic Works All Dissertations, Theses, and Capstone Projects Dissertations, Theses, and Capstone Projects 6-2014 Comparative Phylogeography, Phylogenetics, and Population Genomics of East African Montane Small Mammals Terrence Constant Demos Graduate Center, City University of New York How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/gc_etds/199 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] COMPARATIVE PHYLOGEOGRAPHY, PHYLOGENETICS, AND POPULATION GENOMICS OF EAST AFRICAN MONTANE SMALL MAMMALS by TERRENCE CONSTANT DEMOS A dissertation submitted to the Graduate Faculty in Biology in partial fulfillment of the requirements for the degree of Doctor of Philosophy, The City University of New York 2014 ii This manuscript has been read and accepted for the Graduate Faculty in Biology in satisfaction of the dissertation requirement for the degree of Doctor of Philosophy. Michael J. Hickerson___________________ 4/25/2014___________ ____________________________________ Date Chair of Examining Committee Laurel A. Eckhardt____________________ 4/29/2014___________ __________________________________ Date Executive Officer Frank. T. Burbrink_____________________________ Julian C. Kerbis Peterhans______________________ Jason Munshi-South___________________________ Ana Carolina Carnaval_________________________ Supervision Committee The City University of New York iii Abstract COMPARATIVE PHYLOGEOGRAPHY, PHYLOGENETICS, AND POPULATION GENOMICS OF EAST AFRICAN MONTANE SMALL MAMMALS by TERRENCE CONSTANT DEMOS Advisor: Dr. Michael J. Hickerson The Eastern Afromontane region of Africa is characterized by striking levels of endemism and species richness which rank it as a global biodiversity hotspot for diverse plants and animals including mammals, but has been poorly sampled and little studied to date. -

Terrestrial Small Mammals (Soricidae and Muridae) from the Gamba Complex of Protected Areas, Gabon: Species Composition and Comparison of Sampling Techniques
Terrestrial Small Mammals (Soricidae and Muridae) from the Gamba Complex of Protected Areas, Gabon: Species Composition and Comparison of Sampling Techniques Carrie 0'BRIEN\ William McSHEA^ Sylvain GUIMONDOU^ Patrick BARRIERE^ and Michael CARLETON^ 1 Introduction In this paper, we document species of terrestrial insectivores (Soricidae) and rodents (Muridae) The Guineo-Congolian region encompasses 2.8 mil- weighing less than 100 g that occur in the Gamba lion km"^ of lowland rainforest stretching from the Complex, compare faunal composition between coastal regions of West Africa to eastern Democratic coastal and inland sites, and test the success of dif- Republic of Congo (White 2001). The altitude is less ferent sampling protocols. In addition, we discuss than 1000 m except for a few higher peaks, and the our findings in the context of other mammal surveys rainfall averages 1600-2000 mm per year The region conducted in lowland rainforests of Central Africa. is renowned for both its plant and animal diversity, with an estimated 8000 species of plants (80% 2 Study Area endemic. White 1983) and 270 species of lowland mammals belonging to 120 genera (Grubb 2001, The Gamba Complex in southern Gabon comprises White 2001). Gabon, in the heart of the Guineo- the Ndogo and Ngové lagoons and their drainages and Congolian region, has some 80% of its original trop- encompasses over 11,000 km^ of coastal and inland ical moist forest remaining, which is the highest of rainforest. The major habitat types within the Complex all West, Central, and East African rainforest coun- include coastal scrub forest, mangrove forest, savan- tries (Naughton-Treves and Weber 2001). -

Enter the Bank Vole
Bryan Schønecker The Bank Vole as Experimental Animal Second Edition Frydenskrig Forlag The Bank Vole as Experimental Animal, Second Edition Copyright © Bryan Schønecker 2014 All rights reserved Published by Frydenskrig Forlag, Denmark Cover and photos by Bryan Schønecker Font: Georgia ISBN-13: 978-87-997324-0-1 (EPUB) ISBN-13: 978-87-997324-1-8 (PDF) First Edition by Saxo Publish, Denmark, 2013 Other books by the author: Student’s guide to Diabetes. 2013 Student’s guide to Epilepsy. 2013 Student’s guide to Animal Stereotypies. 2013 Student’s guide to Animal Models. 2013 Contents. Preface 1 Abbreviations 2 Chapter 1 Enter the bank vole 3 1.1 Name. 3 1.2 Appearance and measurements. 4 1.3 Placement in the phylogeny. 4 1.4 Distribution and population dynamics. 5 1.5 Habitat and food. 7 1.6 Parasites, bacteria and viruses in wild bank voles. 7 1.7 Breeding season in the wild. 9 1.8 Reproduction and longevity in captivity. 9 1.9 Diurnal activity in captivity. 11 Chapter 2 How to get your bank voles 12 2.1 Legal matters. 12 2.2 Possible ways to get some bank voles. 12 2.3 How to catch your bank voles. 13 2.3.1 The Sherman trap. 13 2.3.2 The Ugglan Special #1 trap. 15 2.3.3 My personal favourite - the Ugglan trap. 16 2.4 Baiting the trap. 17 2.5 Placing the traps. 17 2.6 Checking the traps. 19 2.7 Confusion with field voles. 19 Chapter 3 How to keep your bank voles 20 3.1 Precautions against potential zoonoses. -

Muellner Artist Cv 2013
NICHOLAS MUELLNER [email protected] www.nicholasmuellner.com EDUCATION 1994 Master of Fine Arts, Tyler School of Art of Temple University, Philadelphia, PA 1993 Graduate Study in Philosophy and Aesthetics, Temple University, Rome 1991 Bachelor of Arts, Comparative Literature (Magna cum laude with Distinction in the Major), Yale University, New Haven, CT FELLOWSHIPS, GRANTS AND AWARDS 2010 MacDowell Colony Fellowship 2007 Trust for Mutual Understanding. International project grant. CEC Artslink. International project grant. New York Council for the Humanities, Small project grant. 2003-2012 Pendleton Research and Production Grants, Park School of Communications, Ithaca, NY 1993–1994 Presidential Fellowship, Temple University, Philadelphia, PA 1993 Mellon Foundation Production Grant, administered by Temple University, Philadelphia, PA 1990 Class of 1956 Traveling Fellowship BOOKS Mountain Shadow Place. A-Jump Books, Ithaca, NY October, 2012. Photographs and text by Nicholas Muellner. Limited edition book, with hand-silkscreened cover and 2 posters; edition of 100. The Amnesia Pavilions. A-Jump Books, Ithaca, NY, October, 2011. Photographs and text by Nicholas Muellner; 220 pages; 114 illustrations. Named one of the best photo books of 2011 by Time Magazine; shortlisted for Artistʼs Book of the Moment for 2012 by the Gallery of York University, Toronto. The Photograph Commands Indifference. A-Jump Books, Ithaca, NY, 2009. Photographs and text by Nicholas Muellner; design by Gerry Beegan; 84 pages, 66 illustrations. Moscow Plastic Arts. Arcadia University Art Gallery, Glenside, PA. Photographs and text by Nicholas Muellner; 48 pages, 22 color illustrations. WEB PUBLICATIONS 2011 “Amnesia Pavilions,” in Triple Canopy, Issue 15, December 2011. Original texts and photographs in embedded audio slideshows.