Identification of a Frameshift Mutation in SON Gene Via Whole Exome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transcriptional Integration of Mitogenic and Mechanical Signals by Myc and YAP
Downloaded from genesdev.cshlp.org on September 30, 2021 - Published by Cold Spring Harbor Laboratory Press RESEARCH COMMUNICATION rum-mediated and growth factor-mediated cell cycle Transcriptional integration entry (Kelly et al. 1983; Armelin et al. 1984; Roussel of mitogenic and mechanical et al. 1991; Barone and Courtneidge 1995; de Alboran et al. 2001; Trumpp et al. 2001; Perna et al. 2012). This signals by Myc and YAP function of Myc stems from its ability to control the ex- pression of a large fraction of genes involved in cell activa- Ottavio Croci,1,5 Serena De Fazio,1,5 1,5 1,4,5 tion and proliferation. Francesca Biagioni, Elisa Donato, When ectopically expressed in quiescent cells, Myc is Marieta Caganova,1 Laura Curti,1 Mirko Doni,2 able to drive cell cycle progression in the absence of serum Silvia Sberna,1 Deborah Aldeghi,1 (Eilers et al. 1991; Pelengaris et al. 1999). This effect of Chiara Biancotto,1 Alessandro Verrecchia,2 Myc is context-dependent, however, since not all cells or tissues respond to Myc by entering the cell cycle (Jack- Daniela Olivero,3 Bruno Amati,1,2 1 son et al. 1990; Xiao et al. 2001; Murphy et al. 2008). This and Stefano Campaner suggests that a full proliferative response may require the engagement of other TFs, which may respond to different 1Center for Genomic Science of IIT@SEMM (Istituto Italiano di regulatory signals, such as metabolic or mechanical cues. Tecnologia at European School of Molecular Medicine), Recently, YAP has emerged as a key TF in the control of Fondazione Istituto Italiano di Tecnologia (IIT), 20139 Milan, cell growth and organ size in response to a variety of Italy; 2Department of Experimental Oncology, European signals such as cell adhesion, apico–basolateral polarity, Institute of Oncology (IEO), 20139 Milan, Italy; 3Laboratorio di cytoskeletal tension, and mitogens. -

Whole Exome Sequencing Gene Package Intellectual Disability, Version 9.1, 31-1-2020
Whole Exome Sequencing Gene package Intellectual disability, version 9.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A2ML1 {Otitis media, susceptibility to}, 166760 610627 66 100 100 96 AARS1 Charcot-Marie-Tooth disease, axonal, type 2N, 613287 601065 63 100 97 90 Epileptic encephalopathy, early infantile, 29, 616339 AASS Hyperlysinemia, -

Psykisk Utviklingshemming Og Forsinket Utvikling
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD -

Your Genes, Your Choices
Your Genes, Your Choices: Exploring the Issues Raised by Genetic Research by Catherine Baker Table of Contents Acknowledgments . 6 Introduction . 7 Chapter 1 Martin Needs Medical Treatment (or does he?) . 9 Chapter 2 Priya Should Find Out if She Has Inherited a Fatal Disease (or should she?) . 14 Chapter 3 Howard’s Health Is Up to Him (or is it?) . 26 Chapter 4 Carlos and Mollie Can Have a Perfectly Healthy Baby (or can they?) . 35 Chapter 5 Donita Should Cooperate with the Police (or should she?) . 45 Chapter 6 John and Elsa Will Profit from Biotech Farming (or will they?) . 52 Chapter 7 Dr. Lu’s Patients Have the Right to Be Tall (or do they?) . 62 Chapter 8 Mrs. Fister Can Replace Her Dying Son (or can she?) . 70 Glossary . 81 References . 89 Credits . 81 Science + Literacy for Health Human Genome Project Advisory Board . 93 5 Acknowledgments I am not a science writer by trade. In order to write this book, I first had to study up on genetics and the issues involved. Then I had to try to explain them in a way that other newcomers to the subject could understand, without making terrible errors. It was a difficult task! I am therefore indebted to the members of the AAAS Advisory Panel (listed on page 82). At an all-day meeting in the spring of 1995, they steered my away from my original outline toward the book you find here. Many months later, several panel members provided very useful reviews of the manuscript. For this, I would like to thank Ruth Allen, Jeffrey Botkin, Ron Cole-Turner, Robert Cook-Deegan, and Joan Weiss. -

Structure and Mechanism of the RNA Polymerase II Transcription Machinery
Downloaded from genesdev.cshlp.org on October 9, 2021 - Published by Cold Spring Harbor Laboratory Press REVIEW Structure and mechanism of the RNA polymerase II transcription machinery Allison C. Schier and Dylan J. Taatjes Department of Biochemistry, University of Colorado, Boulder, Colorado 80303, USA RNA polymerase II (Pol II) transcribes all protein-coding ingly high resolution, which has rapidly advanced under- genes and many noncoding RNAs in eukaryotic genomes. standing of the molecular basis of Pol II transcription. Although Pol II is a complex, 12-subunit enzyme, it lacks Structural biology continues to transform our under- the ability to initiate transcription and cannot consistent- standing of complex biological processes because it allows ly transcribe through long DNA sequences. To execute visualization of proteins and protein complexes at or near these essential functions, an array of proteins and protein atomic-level resolution. Combined with mutagenesis and complexes interact with Pol II to regulate its activity. In functional assays, structural data can at once establish this review, we detail the structure and mechanism of how enzymes function, justify genetic links to human dis- over a dozen factors that govern Pol II initiation (e.g., ease, and drive drug discovery. In the past few decades, TFIID, TFIIH, and Mediator), pausing, and elongation workhorse techniques such as NMR and X-ray crystallog- (e.g., DSIF, NELF, PAF, and P-TEFb). The structural basis raphy have been complemented by cryoEM, cross-linking for Pol II transcription regulation has advanced rapidly mass spectrometry (CXMS), and other methods. Recent in the past decade, largely due to technological innova- improvements in data collection and imaging technolo- tions in cryoelectron microscopy. -

"The Genecards Suite: from Gene Data Mining to Disease Genome Sequence Analyses". In: Current Protocols in Bioinformat
The GeneCards Suite: From Gene Data UNIT 1.30 Mining to Disease Genome Sequence Analyses Gil Stelzer,1,5 Naomi Rosen,1,5 Inbar Plaschkes,1,2 Shahar Zimmerman,1 Michal Twik,1 Simon Fishilevich,1 Tsippi Iny Stein,1 Ron Nudel,1 Iris Lieder,2 Yaron Mazor,2 Sergey Kaplan,2 Dvir Dahary,2,4 David Warshawsky,3 Yaron Guan-Golan,3 Asher Kohn,3 Noa Rappaport,1 Marilyn Safran,1 and Doron Lancet1,6 1Department of Molecular Genetics, Weizmann Institute of Science, Rehovot, Israel 2LifeMap Sciences Ltd., Tel Aviv, Israel 3LifeMap Sciences Inc., Marshfield, Massachusetts 4Toldot Genetics Ltd., Hod Hasharon, Israel 5These authors contributed equally to the paper 6Corresponding author GeneCards, the human gene compendium, enables researchers to effectively navigate and inter-relate the wide universe of human genes, diseases, variants, proteins, cells, and biological pathways. Our recently launched Version 4 has a revamped infrastructure facilitating faster data updates, better-targeted data queries, and friendlier user experience. It also provides a stronger foundation for the GeneCards suite of companion databases and analysis tools. Improved data unification includes gene-disease links via MalaCards and merged biological pathways via PathCards, as well as drug information and proteome expression. VarElect, another suite member, is a phenotype prioritizer for next-generation sequencing, leveraging the GeneCards and MalaCards knowledgebase. It au- tomatically infers direct and indirect scored associations between hundreds or even thousands of variant-containing genes and disease phenotype terms. Var- Elect’s capabilities, either independently or within TGex, our comprehensive variant analysis pipeline, help prepare for the challenge of clinical projects that involve thousands of exome/genome NGS analyses. -

The General Transcription Factors of RNA Polymerase II
Downloaded from genesdev.cshlp.org on October 7, 2021 - Published by Cold Spring Harbor Laboratory Press REVIEW The general transcription factors of RNA polymerase II George Orphanides, Thierry Lagrange, and Danny Reinberg 1 Howard Hughes Medical Institute, Department of Biochemistry, Division of Nucleic Acid Enzymology, Robert Wood Johnson Medical School, University of Medicine and Dentistry of New Jersey, Piscataway, New Jersey 08854-5635 USA Messenger RNA (mRNA) synthesis occurs in distinct unique functions and the observation that they can as- mechanistic phases, beginning with the binding of a semble at a promoter in a specific order in vitro sug- DNA-dependent RNA polymerase to the promoter re- gested that a preinitiation complex must be built in a gion of a gene and culminating in the formation of an stepwise fashion, with the binding of each factor promot- RNA transcript. The initiation of mRNA transcription is ing association of the next. The concept of ordered as- a key stage in the regulation of gene expression. In eu- sembly recently has been challenged, however, with the karyotes, genes encoding mRNAs and certain small nu- discovery that a subset of the GTFs exists in a large com- clear RNAs are transcribed by RNA polymerase II (pol II). plex with pol II and other novel transcription factors. However, early attempts to reproduce mRNA transcrip- The existence of this pol II holoenzyme suggests an al- tion in vitro established that purified pol II alone was not ternative to the paradigm of sequential GTF assembly capable of specific initiation (Roeder 1976; Weil et al. (for review, see Koleske and Young 1995). -

The Mammalian Phenotype Ontology As a Tool for Annotating, Analyzing and Comparing Phenotypic Information
Open Access Method2004SmithetVolume al. 6, Issue 1, Article R7 The Mammalian Phenotype Ontology as a tool for annotating, comment analyzing and comparing phenotypic information Cynthia L Smith*, Carroll-Ann W Goldsmith*† and Janan T Eppig* Addresses: *The Jackson Laboratory, 600 Main Street, Bar Harbor, ME 04609, USA. †Massachusetts College of Pharmacy and Health Sciences, School of Pharmacy Manchester, 1260 Elm Street, Manchester, NH 03101, USA. Correspondence: Janan T Eppig. E-mail: [email protected] reviews Published: 15 December 2004 Received: 8 September 2004 Revised: 15 November 2004 Genome Biology 2004, 6:R7 Accepted: 17 November 2004 The electronic version of this article is the complete one and can be found online at http://genomebiology.com/2004/6/1/R7 © 2004 Smith et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), reports which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The<p>Thetativeofresearchand phenotypic RatMammalian trait Genome Mammaliangroups, loci knowledge and mutagenesisPhenotypeDatabase strains Phenotype and thatto Ontology flexiblereconsortia, arepresent (MP) used annota asOntology phenotypicand asa tool models tionsbiological for enables to annotating,of data.</p> individual human domain robust biology analyzingexperts. genotypes.annotation and The and disease. It of MP continues comparingmammalian Ontology The MPto phenotypic isdevelop Ontolphenotypes currentlyogy dynamically supportsinformation used in the by thecontext different via Mouse collaborative of levels mutations,Genome and input Da richness quanti-tabase from Abstract deposited research The Mammalian Phenotype (MP) Ontology enables robust annotation of mammalian phenotypes in the context of mutations, quantitative trait loci and strains that are used as models of human biology and disease. -

Regulation of RNA Polymerase II Transcription
Regulation of RNA polymerase II transcription Ronny Drapkin, Alejandro Merino and Danny Reinberg Robert Wood Johnson Medical School, University of Medicine and Dentistry of New Jersey, Piscataway, USA Transcription initiation plays a central role in the regulation of gene expression. Exciting developments in the last year have furthered our understanding of the interactions between general transcription factors and how these factors respond to modulators of transcription. Current Opinion in Cell Biology 1993, 5:469-476 Introduction TFIIJ. Formation of the DAB--polFEHJ complex, in the presence of each of four ribonucleoside triphosphates, Cellular growth and differentiation employ precise mech- enables RNAPII to clear the promoter region and initiate anisms to regulate the expression of various genes. One RNA synthesis from a specific start site [ 51. of the most rudimentary mechanisms for a cell to control The past year has seen intense activity aimed at elucidat- the functional levels of a protein is to modulate the lev- ing the molecular mechanisms underlying transcription els of mRNA encoding that polypeptide. It is therefore not initiation. In particular, the interactions that GTFs can surprising that most of the genetic programs that main- mediate, the GTF requirements for initiation, the role tain the cell in a constant state of flux mediate their effects of RNAPII phosphorylation, and the phenomenon of by impinging on mechanisms that control transcription antirepression in the process of activation have been initiation. the subject of many studies. These most recent develop- In contrast to prokaryotic RNA polymerase, eukaryotic ments are the focus of this review. enzymes require multiple accessory proteins to acquire promoter specificity. -

Gene Mapping and Medical Genetics Human Chromosome 8
J Med Genet: first published as 10.1136/jmg.25.11.721 on 1 November 1988. Downloaded from Gene mapping and medical genetics Journal of Medical Genetics 1988, 25, 721-731 Human chromosome 8 STEPHEN WOOD From the Department of Medical Genetics, University of British Columbia, 6174 University Boulevard, Vancouver, British Columbia, Canada V6T IWS. SUMMARY The role of human chromosome 8 in genetic disease together with the current status of the genetic linkage map for this chromosome is reviewed. Both hereditary genetic disease attributed to mutant alleles at gene loci on chromosome 8 and neoplastic disease owing to somatic mutation, particularly chromosomal translocations, are discussed. Human chromosome 8 is perhaps best known for its In an era when complete sequencing of the human involvement in Burkitt's lymphoma and as the genome is being proposed, it is appropriate for location of the tissue plasminogen activator gene, medical geneticists to accept the challenge of defining by copyright. PLAT, which has been genetically engineered to the set of loci that have mutant alleles causing provide a natural fibrinolytic product for emergency hereditary disease. The fundamental genetic tool of use in cardiac disease. Since chromosome 8 repre- linkage mapping can now be applied, owing largely sents about 5% of the human genome, we may to progress in defining RFLP markers.3 4 This expect it to carry about 5% of human gene loci. This review will focus on genetic disease associated with would correspond to about 90 of the fully validated chromosome 8 loci and the status ofthe chromosome 8 phenotypes in the MIM7 catalogue.' The 27 genes linkage map. -

Selective Gene Expression in Magnocellular Neurons in Rat Supraoptic Nucleus
7174 • The Journal of Neuroscience, August 11, 2004 • 24(32):7174–7185 Cellular/Molecular Selective Gene Expression in Magnocellular Neurons in Rat Supraoptic Nucleus Noriko Mutsuga,1 Tal Shahar,1 Joseph G. Verbalis,3 Michael J. Brownstein,2 Charlie C. Xiang,2 Robert F. Bonner,4 and Harold Gainer1 1Laboratory of Neurochemistry, National Institute of Neurological Disorders and Stroke, National Institutes of Health, 2Laboratory of Genetics, National Institute of Mental Health, National Institutes of Health, Bethesda, Maryland 20892, 3Department of Medicine, Division of Endocrinology and Metabolism, Georgetown University, Washington, DC 20007, and 4Laboratory of Integrative and Medical Biophysics, National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland 20892-5772 Oxytocin- and vasopressin-producing magnocellular neurons (MCNs) of the hypothalamo-neurohypophysial system are the only neu- ronal phenotypes present in the rat supraoptic nucleus (SON). Laser microdissection of the SON, extraction and T7-based amplification of its RNAs, and analysis of the resulting cDNAs by hybridization on a 35, 319 element DNA microarray have provided a detailed composite view of the gene expression profile of the MCNs. The genes expressed in the SON were compared with those expressed in a reference tissue consisting of total hypothalamus, and this “expression ratio” indicated which genes were preferentially expressed in the SON. Of the 26,000 unique genes on the array, 1385 were found to be expressed in the SON at levels more than two times greater than in the hypothalamus as a whole. Of these, 123 were expressed Ն3.4-fold higher in the SON versus hypothalamus. Most of these preferentially expressed genes were not previously known to be expressed in the MCNs. -
Utviklingsavvik V02
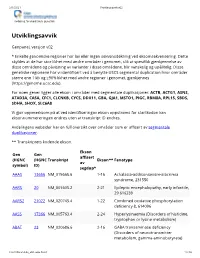
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate)