Tasuku Honjo Kyoto University, Kyoto, Japan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Issue
Cell Circuitry || Science Teaches English || The Chicken Genome Is Hot || Magnets in Medicine SEPTEMBER 2002 www.hhmi.org/bulletin Leading Doublea Life It’s a stretch, but doctors who work bench to bedside say they wouldn’t do it any other way. FEATURES 14 On Human Terms 24 The Evolutionary War A small—some say too small—group of Efforts to undermine evolution education have physician-scientists believes the best science evolved into a 21st-century marketing cam- requires patient contact. paign that relies on legal acumen, manipulation By Marlene Cimons of scientific literature and grassroots tactics. 20 Engineering the Cell By Trisha Gura Adam Arkin sees the cell as a mechanical system. He hopes to transform molecular 28 Call of the Wild biology into a kind of cellular engineering Could quirky, new animal models help scien- and in the process, learn how to move cells tists learn how to regenerate human limbs or from sickness to health. avert the debilitating effects of a stroke? By M. Mitchell Waldrop By Kathryn Brown 24 In front of a crowd of 1,500, Ohio’s Board of Education heard testimony on whether students should learn about intelligent design in science class. DEPARTMENTS 2 NOTA BENE 33 PERSPECTIVE ulletin Intelligent Design Is a Cop-Out 4 LETTERS September 2002 || Volume 15 Number 3 NEWS AND NOTES HHMI TRUSTEES PRESIDENT’S LETTER 5 JAMES A. BAKER, III, ESQ. 34 Senior Partner, Baker & Botts A Creative Influence In from the Fields ALEXANDER G. BEARN, M.D. Executive Officer, American Philosophical Society 35 Lost on the Tip of the Tongue Adjunct Professor, The Rockefeller University UP FRONT Professor Emeritus of Medicine, Cornell University Medical College 36 Biology by Numbers FRANK WILLIAM GAY 6 Follow the Songbird Former President and Chief Executive Officer, SUMMA Corporation JAMES H. -

Enhanced Monocyte Migration to CXCR3 and CCR5 Chemokines in COPD
ERJ Express. Published on March 10, 2016 as doi: 10.1183/13993003.01642-2015 ORIGINAL ARTICLE IN PRESS | CORRECTED PROOF Enhanced monocyte migration to CXCR3 and CCR5 chemokines in COPD Claudia Costa1, Suzanne L. Traves1, Susan J. Tudhope1, Peter S. Fenwick1, Kylie B.R. Belchamber1, Richard E.K. Russell2, Peter J. Barnes1 and Louise E. Donnelly1 Affiliations: 1Airway Disease, National Heart and Lung Institute, Imperial College London, London, UK. 2Chest Clinic, King Edward King VII Hospital, Windsor, UK. Correspondence: Louise E. Donnelly, Airway Disease, National Heart and Lung Institute, Dovehouse Street, London, SW3 6LY, UK. E-mail: [email protected] ABSTRACT Chronic obstructive pulmonary disease (COPD) patients exhibit chronic inflammation, both in the lung parenchyma and the airways, which is characterised by an increased infiltration of macrophages and T-lymphocytes, particularly CD8+ cells. Both cell types can express chemokine (C-X-C motif) receptor (CXCR)3 and C-C chemokine receptor 5 and the relevant chemokines for these receptors are elevated in COPD. The aim of this study was to compare chemotactic responses of lymphocytes and monocytes of nonsmokers, smokers and COPD patients towards CXCR3 ligands and chemokine (C-C motif) ligand (CCL)5. Migration of peripheral blood mononuclear cells, monocytes and lymphocytes from nonsmokers, smokers and COPD patients toward CXCR3 chemokines and CCL5 was analysed using chemotaxis assays. There was increased migration of peripheral blood mononuclear cells from COPD patients towards all chemokines studied when compared with nonsmokers and smokers. Both lymphocytes and monocytes contributed to this enhanced response, which was not explained by increased receptor expression. -

Nobel Laureates Endorse Joe Biden
Nobel Laureates endorse Joe Biden 81 American Nobel Laureates in Physics, Chemistry, and Medicine have signed this letter to express their support for former Vice President Joe Biden in the 2020 election for President of the United States. At no time in our nation’s history has there been a greater need for our leaders to appreciate the value of science in formulating public policy. During his long record of public service, Joe Biden has consistently demonstrated his willingness to listen to experts, his understanding of the value of international collaboration in research, and his respect for the contribution that immigrants make to the intellectual life of our country. As American citizens and as scientists, we wholeheartedly endorse Joe Biden for President. Name Category Prize Year Peter Agre Chemistry 2003 Sidney Altman Chemistry 1989 Frances H. Arnold Chemistry 2018 Paul Berg Chemistry 1980 Thomas R. Cech Chemistry 1989 Martin Chalfie Chemistry 2008 Elias James Corey Chemistry 1990 Joachim Frank Chemistry 2017 Walter Gilbert Chemistry 1980 John B. Goodenough Chemistry 2019 Alan Heeger Chemistry 2000 Dudley R. Herschbach Chemistry 1986 Roald Hoffmann Chemistry 1981 Brian K. Kobilka Chemistry 2012 Roger D. Kornberg Chemistry 2006 Robert J. Lefkowitz Chemistry 2012 Roderick MacKinnon Chemistry 2003 Paul L. Modrich Chemistry 2015 William E. Moerner Chemistry 2014 Mario J. Molina Chemistry 1995 Richard R. Schrock Chemistry 2005 K. Barry Sharpless Chemistry 2001 Sir James Fraser Stoddart Chemistry 2016 M. Stanley Whittingham Chemistry 2019 James P. Allison Medicine 2018 Richard Axel Medicine 2004 David Baltimore Medicine 1975 J. Michael Bishop Medicine 1989 Elizabeth H. Blackburn Medicine 2009 Michael S. -

2004 Albert Lasker Nomination Form
albert and mary lasker foundation 110 East 42nd Street Suite 1300 New York, ny 10017 November 3, 2003 tel 212 286-0222 fax 212 286-0924 Greetings: www.laskerfoundation.org james w. fordyce On behalf of the Albert and Mary Lasker Foundation, I invite you to submit a nomination Chairman neen hunt, ed.d. for the 2004 Albert Lasker Medical Research Awards. President mrs. anne b. fordyce The Awards will be offered in three categories: Basic Medical Research, Clinical Medical Vice President Research, and Special Achievement in Medical Science. This is the 59th year of these christopher w. brody Treasurer awards. Since the program was first established in 1944, 68 Lasker Laureates have later w. michael brown Secretary won Nobel Prizes. Additional information on previous Lasker Laureates can be found jordan u. gutterman, m.d. online at our web site http://www.laskerfoundation.org. Representative Albert Lasker Medical Research Awards Program Nominations that have been made in previous years may be updated and resubmitted in purnell w. choppin, m.d. accordance with the instructions on page 2 of this nomination booklet. daniel e. koshland, jr., ph.d. mrs. william mccormick blair, jr. the honorable mark o. hatfied Nominations should be received by the Foundation no later than February 2, 2004. Directors Emeritus A distinguished panel of jurors will select the scientists to be honored. The 2004 Albert Lasker Medical Research Awards will be presented at a luncheon ceremony given by the Foundation in New York City on Friday, October 1, 2004. Sincerely, Joseph L. Goldstein, M.D. Chairman, Awards Jury Albert Lasker Medical Research Awards ALBERT LASKER MEDICAL2004 RESEARCH AWARDS PURPOSE AND DESCRIPTION OF THE AWARDS The major purpose of these Awards is to recognize and honor individuals who have made signifi- cant contributions in basic or clinical research in diseases that are the main cause of death and disability. -
Annual Report Fy 2018 Human Frontier Science Program Organization
APRIL 2017 APRIL 2018 — MARCH 2019 ANNUAL REPORT FY 2018 HUMAN FRONTIER SCIENCE PROGRAM ORGANIZATION The Human Frontier Science Program Organization (HFSPO) is unique, supporting international collaboration to undertake innovative, risky, basic research at the frontier of the life sciences. Special emphasis is given to the support and training of independent young investigators, beginning at the postdoctoral level. The Program is implemented by an international organisation, supported financially by Australia, Canada, France, Germany, India, Italy, Japan, the Republic of Korea, New Zealand, Norway, Singapore, Switzerland, the United Kingdom of Great Britain and Nothern Ireland, the United States of America, and the European Commission. Since 1990, over 7000 researchers from more than 70 countries have been supported. Of these, 28 HFSP awardees have gone on to receive the Nobel Prize. 2 The following documents are available on the HFSP website www.hfsp.org: Joint Communiqués (Tokyo 1992, Washington 1997, Berlin 2002, Bern 2004, Ottawa 2007, Canberra 2010, Brussels 2013, London 2016): https://www.hfsp.org/about/governance/membership Statutes of the International Human Frontier Science Program Organization: https://www.hfsp.org/about/governance/hfspo-statutes Guidelines for the participation of new members in HFSPO: https://www.hfsp.org/about/governance/membership General reviews of the HFSP (1996, 2001, 2006-2007, 2010, 2018): https://www.hfsp.org/about/strategy/reviews Updated and previous lists of awards, including titles and abstracts: -

IL-34–Dependent Intrarenal and Systemic Mechanisms Promote Lupus Nephritis in MRL-Faslpr Mice
BASIC RESEARCH www.jasn.org IL-34–Dependent Intrarenal and Systemic Mechanisms Promote Lupus Nephritis in MRL-Faslpr Mice Yukihiro Wada,1 Hilda M. Gonzalez-Sanchez,1 Julia Weinmann-Menke,2 Yasunori Iwata,1 Amrendra K. Ajay,1 Myriam Meineck,2 and Vicki R. Kelley1 1Renal Division, Department of Medicine, Brigham and Women’s Hospital, Boston, Massachusetts; and 2Department of Nephrology and Rheumatology, University Medical Center of the Johannes Gutenberg University Mainz, Mainz, Germany ABSTRACT lpr Background In people with SLE and in the MRL-Fas lupus mouse model, macrophages and autoanti- bodies are central to lupus nephritis. IL-34 mediates macrophage survival and proliferation, is expressed by tubular epithelial cells (TECs), and binds to the cFMS receptor on macrophages and to a newly identified second receptor, PTPRZ. Methods To investigate whether IL-34–dependent intrarenal and systemic mechanisms promote lupus lpr nephritis, we compared lupus nephritis and systemic illness in MRL-Fas mice expressing IL-34 and IL-34 lpr knockout (KO) MRL-Fas mice. We also assessed expression of IL-34 and the cFMS and PTPRZ receptors in patients with lupus nephritis. lpr Results Intrarenal IL-34 and its two receptors increase during lupus nephritis in MRL-Fas mice. In knock- out mice lacking IL-34, nephritis and systemic illness are suppressed. IL-34 fosters intrarenal macrophage accumulation via monocyte proliferation in bone marrow (which increases circulating monocytes that are recruited by chemokines into the kidney) and via intrarenal macrophage proliferation. This accumulation leads to macrophage-mediated TEC apoptosis. We also found suppression of circulating autoantibodies and glomerular antibody deposits in the knockout mice. -

October 11, 1994, NIH Record, Vol. XLVI, No. 21
October l 1, 1994 Vol. XLVI No. 21 "Still U.S. Department of Health The Second and Human Services Best Thing About Payday" National Institutes of Health Dunbar To Give First Pittman Lecture, Oct. 26 By Sara Byars scientist recognized internarionally for A her pioneering work in contraceptive vaccines has been selected to deliver the first Margaret Pittman Lecture, a new NIH series chat honors outstanding women scientists. Dr. Bonnie S. Dunbar, professor of cell . :/ biology and obstetrics and gynecology at Baylor College of Medicine, will speak on "New ':'' .:' f ,; ... .. Fromiers in Reproductive Biology and I !- J ~ , • I , , ' f ., ' / , , Contraceptive Vaccines" at 3 p.m. on 0cc. 26 ' • /} : 4 t ., : in Masur Auditorium, Bldg. I 0 . ' ' . ! • ' I I I • Guiding che development of che Pittman • ' ' ,• ,: k'I I ' I lectureship series is the NIH women scientists J: • ! • •'I I It♦ l'- : ,4 • • •· ... / ;~ ~ advisory committee, a group char advises At the NIH Research Festival 1994 poster session, Dr. Lynn Hudson (r), chief. molecular genetics section scientific directors on matters pertaining co rhe ofNJNDS' Laboratory ofViral and Molecular Pathogenesis, stops by to view the work ofDr. Rosemary role of women scientists at NIH. Wong, one ofthe authors who works in NIDDK's Molemlar, Cellular and Endocrinology Branch. See This lectureship honors Or. Margaret additional coverage ofthe event on Pages 6-7. Pittman, rhe first woman co hold the position (See PITTMAN LECTURE, Page 2) NIGMS Reorganizes, Moves to Natcher Bldg. is month, che N acional Institute of General Medical Sciences is undergoing a reorganiza Vitetta Is NIAID's 1994 tion and a move to che new William H. -
The YY1/Mir-548T-5P/CXCL11 Signaling Axis Regulates Cell
Ge et al. Cell Death and Disease (2020) 11:294 https://doi.org/10.1038/s41419-020-2475-3 Cell Death & Disease ARTICLE Open Access The YY1/miR-548t-5p/CXCL11 signaling axis regulates cell proliferation and metastasis in human pancreatic cancer Wan-Li Ge1,2,QunChen1,2, Ling-Dong Meng1,2,Xu-MinHuang1,2,Guo-dongShi1,2, Qing-Qing Zong1,3,PengShen1,2, Yi-Chao Lu1,2, Yi-Han Zhang1,2,YiMiao1,2,Jing-JingZhang1,2 andKui-RongJiang 1,2 Abstract Pancreatic cancer (PC) is a malignant tumor with a poor prognosis and high mortality. However, the biological role of miR-548t-5p in PC has not been reported. In this study, we found that miR-548t-5p expression was significantly decreased in PC tissues compared with adjacent tissues, and that low miR-548t-5p expression was associated with malignant PC behavior. In addition, high miR-548t-5p expression inhibited the proliferation, migration, and invasion of PC cell lines. Regarding the molecular mechanism, the luciferase reporter gene, chromatin immunoprecipitation (ChIP), and functional recovery assays revealed that YY1 binds to the miR-548t-5p promoter and positively regulates the expression and function of miR-548t-5p. miR-548t-5p also directly regulates CXCL11 to inhibit its expression. A high level of CXCL11 was associated with worse Tumor Node Metastasis (TNM) staging in patients with PC, enhancing proliferation and metastasis in PC cells. Our study shows that the YY1/miR-548t-5p/CXCL11 axis plays an important role in PC and provides a new potential candidate for the treatment of PC. -
Exploration of Prognostic Biomarkers and Therapeutic Targets in the Microenvironment of Bladder Cancer Based on CXC Chemokines
Exploration of Prognostic Biomarkers and Therapeutic Targets in The Microenvironment of Bladder Cancer Based on CXC Chemokines Xiaoqi Sun Department of Urology, Kaiping Central Hospital, Kaiping, 529300, China Qunxi Chen Department of Pathology, Sun Yat-sen University Cancer Center, Guangzhou, 510060, China Lihong Zhang Department of Pathology, Sun Yat-sen University Cancer Center, Guangzhou, 510060, China Jiewei Chen Department of Pathology, Sun Yat-sen University Cancer Center, Guangzhou, 510060, China Xinke Zhang ( [email protected] ) Sun Yat-sen University Cancer Center Research Keywords: Bladder cancer, Biomarkers, CXC Chemokines, Microenvironment Posted Date: February 24th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-223127/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/29 Abstract Background: Bladder cancer (BLCA) has a high rate of morbidity and mortality, and is considered as one of the most malignant tumors of the urinary system. Tumor cells interact with surrounding interstitial cells, playing a key role in carcinogenesis and progression, which is partly mediated by chemokines. CXC chemokines exert anti‐tumor biological roles in the tumor microenvironment and affect patient prognosis. Nevertheless, their expression and prognostic values patients with BLCA remain unclear. Methods: We used online tools, including Oncomine, UALCAN, GEPIA, GEO databases, cBioPortal, GeneMANIA, DAVID 6.8, Metascape, TRUST (version 2.0), LinkedOmics, TCGA, and TIMER2.0 to perform the relevant analysis. Results: The mRNA levels of C-X-C motif chemokine ligand (CXCL)1, CXCL5, CXCL6, CXCL7, CXCL9, CXCL10, CXCL11, CXCL13, CXCL16, and CXCL17 were increased signicantly increased, and those of CXCL2, CXCL3, and CXCL12 were decreased signicantly in BLCA tissues as assessed using the Oncomine, TCGA, and GEO databases. -

Balcomk41251.Pdf (558.9Kb)
Copyright by Karen Suzanne Balcom 2005 The Dissertation Committee for Karen Suzanne Balcom Certifies that this is the approved version of the following dissertation: Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine Committee: E. Glynn Harmon, Supervisor Julie Hallmark Billie Grace Herring James D. Legler Brooke E. Sheldon Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine by Karen Suzanne Balcom, B.A., M.L.S. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin August, 2005 Dedication I dedicate this dissertation to my first teachers: my father, George Sheldon Balcom, who passed away before this task was begun, and to my mother, Marian Dyer Balcom, who passed away before it was completed. I also dedicate it to my dissertation committee members: Drs. Billie Grace Herring, Brooke Sheldon, Julie Hallmark and to my supervisor, Dr. Glynn Harmon. They were all teachers, mentors, and friends who lifted me up when I was down. Acknowledgements I would first like to thank my committee: Julie Hallmark, Billie Grace Herring, Jim Legler, M.D., Brooke E. Sheldon, and Glynn Harmon for their encouragement, patience and support during the nine years that this investigation was a work in progress. I could not have had a better committee. They are my enduring friends and I hope I prove worthy of the faith they have always showed in me. I am grateful to Dr. -

Mage, Rose G. 2018 Dr
Mage, Rose G. 2018 Dr. Rose G. Mage Oral History Download the PDF: Mage_Rose_oral_history (130 kB) Office of NIH History and Stetten Museum Oral History with Dr. Rose Mage, NIAID August 22, 2018 GM: I am Dr. Gordon Margolin, volunteer in the Office of NIH History and Stetten Museum about to do an oral history with Dr. Rose G. Mage. She served as a Career Investigator in the NIAID Lab of Immunology, starting in 1965, and then as the Section Chief of the Molecular Immunogenetics section from 1988 until her retirement in 2008. We are here in the NIH Library’s audio-visual recording center on August 22, 2018. Thank you, Dr. Mage, for agreeing to record this history about you, your scientific accomplishments, and the time you spent here at NIH. Let’s begin by asking you to tell me a bit of your background, where you were raised, something about your family, and your educational pathway. RGM: I was born and raised in New York City. My father was an immigrant from Romania. He arrived in New York when he was 5 years old in 1905. I was named after his mother who died from typhoid in the 1920s. My mother was born in the USA but her family, three of her four older brothers were immigrants. I decided I wanted to be a scientist when I was about 9 years old, did well in public schools and skipped grades twice. I applied to the Bronx High School of Science and was accepted after taking a written test for admission. -
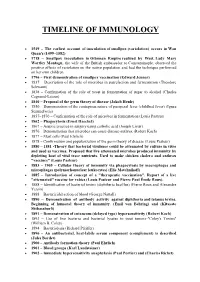
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins.