Plantar Fasciitis Standard of Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plantar Fascia-Specific Stretching Program for Plantar Fasciitis
Plantar Fascia-Specific Stretching Program For Plantar Fasciitis Plantar Fascia Stretching Exercise 1. Cross your affected leg over your other leg. 2. Using the hand on your affected side, take hold of your affected foot and pull your toes back towards shin. This creates tension/stretch in the arch of the foot/plantar fascia. 3. Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string. 4. Hold the stretch for a count of 10. A set is 10 repetitions. 5. Perform at least 3 sets of stretches per day. You cannot perform the stretch too often. The most important times to stretch are before taking the first step in the morning and before standing after a period of prolonged sitting. Plantar Fascia Stretching Exercise 1 2 3 4 URMC Orthopaedics º 4901 Lac de Ville Boulevard º Building D º Rochester, NY 14618 º 585-275-5321 www.ortho.urmc.edu Over, Please Anti-inflammatory Medicine Anti-inflammatory medicine will help decrease the inflammation in the arch and heel of your foot. These include: Advil®, Motrin®, Ibuprofen, and Aleve®. 1. Use the medication as directed on the package. If you tolerate it well, take it daily for 2 weeks then discontinue for 1 week. If symptoms worsen or return, then resume medicine for 2 weeks, then stop. 2. You should eat when taking these medications, as they can be hard on your stomach. Arch Support 1. -

Acral Manifestations of Soft Tissue Tumors Kristen M
Clinics in Dermatology (2017) 35,85–98 Acral manifestations of soft tissue tumors Kristen M. Paral, MD, Vesna Petronic-Rosic, MD, MSc⁎ Section of Dermatology, University of Chicago Pritzker School of Medicine, Chicago, IL Abstract This group of biologically diverse entities is united by topographic localization to the hands and feet. Categorizing tumors by body site narrows the differential into a short list of possibilities that can facil- itate accurate and rapid diagnosis. The goal of this review is to provide a practical approach to soft tissue tumors of acral locations for clinicians, pathologists, and researchers alike. What ensues in the following text is that tight coupling of the clinical picture and histopathologic findings should produce the correct diagno- sis, or at least an abbreviated differential. The salient clinicopathologic, immunohistochemical, and molec- ular features are presented alongside current treatment recommendations for each entity. © 2017 Elsevier Inc. All rights reserved. Introduction actin (SMA) and are deemed “myofibroblasts.”1 The tumors under this heading express combinations of CD34, FXIIIa, fi The entities presented herein are categorized on the basis of and SMA. The synthesis of collagen by broblasts translates fi fi morphogenesis (where possible) and by biologic potential as to a brous consistency that clinically imparts a rm texture benign, intermediate, and malignant neoplasms. on palpation, and, macroscopically, a gray-white or white-tan cut surface. The entities discussed next have no metastatic po- tential; that is, simple excision is adequate. Fibrous and related tissues: Benign lesions Fibroma of tendon sheath fi fl The ontogenetic classi cation of benign lesions re ects appar- Also known as tenosynovial fibroma, compared with other fi fi fi ent broblastic or broblast-like morphogenesis. -
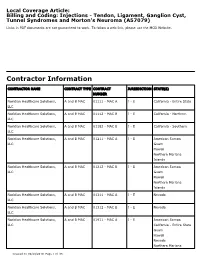
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

The Best Diagnosis Is
Dermatopathology Diagnosis Superficial Plantar Fibromatosis The best diagnosis is: H&E, original magnification 40. a. dermatofibroma b. keloid CUTISc. neurofibroma d. nodular fasciitis Do Note. superficialCopy plantar fibromatosis H&E, original magnification 400. PLEASE TURN TO PAGE 225 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION Luke Lennox, BA; Anna Li, BS; Thomas N. Helm, MD Mr. Lennox and Dr. Helm are from the Department of Dermatology, University at Buffalo, The State University of New York. Ms. Li is from the Department of Dermatology, Ross University, Dominica, West Indies. The authors report no conflict of interest. Correspondence: Thomas N. Helm, MD, Dermatopathology Laboratory, 6255 Sheridan Dr, Building B, Ste 208, Williamsville, NY 14221 ([email protected]). 220 CUTIS® WWW.CUTIS.COM Copyright Cutis 2013. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Dermatopathology Diagnosis Discussion Superficial Plantar Fibromatosis lantar fibromatosis typically presents as firm represents a reactive proliferation of spindle cells most plaques or nodules on the plantar surface of the often encountered on the extremities of young adults. Pfoot.1 The process is caused by a proliferation of Spindle cells are loosely arranged in a mucinous fibroblasts and collagen and has been associated with stroma and are not circumscribed (tissue culture ap- trauma, liver disease, diabetes mellitus, epilepsy, and pearance). Vesicular nuclei are encountered, but there alcoholism.2 Unlike the fibromatoses associated with is no remarkable nuclear pleomorphism. Extravasated Gardner syndrome, superficial plantar fibromatosis has not been associated with abnormalities in the ade- nomatous polyposis coli gene or with the -catenin gene.3,4 Lesions typically present in middle-aged or elderly individuals and involve the medial plantar fas- cia. -

Advice and Exercises for Patients with Plantar Fasciitis
Advice and exercises for patients with plantar fasciitis This leaflet provides management advice and exercises for people diagnosed with plantar fasciitis, a condition causing pain in the heel, sole and /or arch of the foot. Structures of the foot The plantar fascia is a sheet or broad band of fibrous tissue that runs along the bottom of the foot. This tissue connects the heel to the base of the toes. Under normal circumstances, the plantar fascia supports the arch of the foot and acts as a shock absorbing “bow string” within the arch of the foot. With weight bearing, the foot flattens and the plantar fascia stretches, then springing you forward ready for the next step. While walking, the stresses placed on the foot can be one and a quarter times your body weight (this increases to two and three quarter times your body weight when running). Unsurprisingly then, that heel pain is common. If tension on this “bowstring” becomes too great, irritation or inflammation can occur causing pain. What is plantar fasciitis? Plantar fasciitis is a relatively common foot problem affecting up to 10-15% of the population. It can occur at any age. It is sometimes known as “policeman’s heel”. When placed under too much stress due to abnormal loading, the plantar fascia stretches causing micro tearing and degeneration of the tissue. It can lead to pain in the heel, across the sole of the foot and sometimes into the arch area of the foot too. These micro tears repair with scar tissue, which is less flexible than the fascia and can cause the problem to persist for many months. -

A Follow-Up of Patient Reported Outcomes in Chronic Plantar Heel Pain Participants Treated with Graston Technique: a Mixed Methods Approach
University of Northern Iowa UNI ScholarWorks Dissertations and Theses @ UNI Student Work 2016 A follow-up of patient reported outcomes in chronic plantar heel pain participants treated with Graston Technique: A mixed methods approach Troy Richard Garrett University of Northern Iowa Let us know how access to this document benefits ouy Copyright ©2016 Troy Richard Garrett Follow this and additional works at: https://scholarworks.uni.edu/etd Part of the Physical Therapy Commons, and the Physiotherapy Commons Recommended Citation Garrett, Troy Richard, "A follow-up of patient reported outcomes in chronic plantar heel pain participants treated with Graston Technique: A mixed methods approach" (2016). Dissertations and Theses @ UNI. 344. https://scholarworks.uni.edu/etd/344 This Open Access Dissertation is brought to you for free and open access by the Student Work at UNI ScholarWorks. It has been accepted for inclusion in Dissertations and Theses @ UNI by an authorized administrator of UNI ScholarWorks. For more information, please contact [email protected]. Copyright by TROY RICHARD GARRETT 2016 All Rights Reserved A FOLLOW-UP OF PATIENT REPORTED OUTCOMES IN CHRONIC PLANTAR HEEL PAIN PARTICIPANTS TREATED WITH GRASTON TECHNIQUE: A MIXED METHODS APPROACH An Abstract of a Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree Doctor of Education Approved: ____________________________________ Dr. Peter J. Neibert, Committee Chair ____________________________________ Dr. Kavita R. Dhanwada Dean of the Graduate College Troy Richard Garrett University of Northern Iowa December 2016 ABSTRACT Chronic Plantar Heel Pain (CPHP), commonly known as “plantar fasciitis,” is a condition that is estimated to affect 10% of the American population. -

Plantar Fasciitis Exercises
Accurate Clinic 2401 Veterans Memorial Blvd. Suite16 Kenner, LA 70062 - 4799 Phone: 504.472.6130 Fax: 504.472.6128 www.AccurateClinic.com Plantar Fasciitis Exercise Getting the right plantar fasciitis exercise is imperative to ensure the injury doesn’t continue to affect performance. If not given the attention it needs, plantar fasciitis can flair up long after an athlete thinks they’ve recovered and badly damage training plans and competition aspirations. What is plantar fascia? Plantar fascia is a thick, fibrous band of connective tissue which originates at the heel bone and runs along the bottom of the foot in a fan-like manner, attaching to the base of each of the toes. A rather tough, resilient structure, the plantar fascia takes on a number of critical functions during running and walking. Although the fascia is invested with countless sturdy 'cables' of connective tissue called collagen fibres, it is certainly not immune to injury. In fact, about 5 to 10 per cent of all running injuries are inflammations of the fascia, an incidence rate which in the United States would produce about a million cases of plantar fasciitis per year, just among runners and joggers. Basketball players, tennis players, volleyballers, step-aerobics participants, and dancers are also prone to plantar problems, as are non-athletic people who spend a lot of time on their feet or suddenly become active after a long period of lethargy. Why does the fascia flare up? Although it is a fairly rugged structure, the plantar fascia is not very receptive to stretching, and yet stretching occurs in the fascia nearly every time the foot hits the ground. -

A Pilot Study of a Novel Treatment Method for Refractory Painful Plantar Fibromas
Open Access Austin Journal of Orthopedics & Rheumatology Research Article A Pilot Study of a Novel Treatment Method for Refractory Painful Plantar Fibromas Mihir M. Patel*, Sahvan M. Patel, Sia S. Patel and Jacob Daynes Abstract Department of Orthopedic Surgery, OrthoIndy, USA Introduction: Painful plantar fibromas may make ambulation difficult *Corresponding author: Mihir M Patel, Department for patients. They may recur and can make shoe wear difficult to purchase. of Orthopedic Surgery, OrthoIndy 8450 Northwest Blvd, Treatment modalities may include conservative care, modified shoe wear, Indianapolis, Indiana 46278, USA injections and orthotics. Surgical treatment may include open excision. The TX1A probe by Tenex Inc may be a useful alternative treatment modality for Received: March 18, 2015; Accepted: April 22, 2015; these painful lesions. Published: April 22, 2015 Materials and Methods: From 2011 through 2014, eight patients who had painful plantar fibromas elected to undergo definitive treatment for the fibromas. They all had had conservative care including modifications of shoes and either over the counter orthotics or custom orthotics. They all had advanced imaging tests (MRI or CT) preoperatively to help delineate the lesions. The definitive treatment utilized arthroscopy and the TX1A probe and was performed on an outpatient basis. Results: Preoperative AOFAS score was 30.8 (20-36). Postoperative AOFAS score was 90.1 (85-92). Average time of resolution of symptoms was 63.5 days (30-112) and average follow-up was 2.5 years. One patient had another lesion become painful but it was in a different location than the index operation. No others have had a recurrence to date. -
Top 10 Positional-Release Therapy Techniques to Break the Chain of Pain, Part 1 Timothy E
Sacred Heart University DigitalCommons@SHU All PTHMS Faculty Publications Physical Therapy & Human Movement Science 2006 Top 10 Positional-Release Therapy Techniques to Break the Chain of Pain, Part 1 Timothy E. Speicher Sacred Heart University David O. Draper Brigham Young University - Utah Follow this and additional works at: http://digitalcommons.sacredheart.edu/pthms_fac Part of the Physical Therapy Commons, and the Somatic Bodywork and Related Therapeutic Practices Commons Recommended Citation Speicher, Tim and David O. Draper. "Top-10 Positional-Release Therapy Techniques to Break the Chjin of Pain: Part 1. Athletic Therapy Today 11.5 (2006): 69-71. This Peer-Reviewed Article is brought to you for free and open access by the Physical Therapy & Human Movement Science at DigitalCommons@SHU. It has been accepted for inclusion in All PTHMS Faculty Publications by an authorized administrator of DigitalCommons@SHU. For more information, please contact [email protected], [email protected]. THERAPEUTIC MODALITIES David O. Draper, EdD, ATC, Column Editor Top 10 Positional-Release Therapy Techniques to Break the Chain of Pain, Part 1 Tim Speicher, MS, ATC, CSCS • Sacred Heart University David O. Draper, EdD, ATC • Brigham Young University OSITIONAL-RELEASE therapy (PRT) is a counterstrained tissue, decreasing abberent gamma and treatment technique that is gaining popu- alpha neuronal activity, thereby breaking the sustained P larity. The purpose of this two-part column contraction.1 Jones’s original work and PRT theory have -

Plantar Fasciitis Stage 1
PLANTAR FASCIITIS STAGE 1 ADVICE Avoid those activities which aggravate your pain (e.g walking or running). SETS & REPS: N/A FREQUENCY: N/A AVOID FLIP-FLOPS Avoid wearing flip-flops SETS & REPS: N/A FREQUENCY: N/A AVOID HIGH HEELS Avoid high heels. SETS & REPS: N/A FREQUENCY: N/A PLANTAR FASCIA ICE MASSAGE Place a frozen water bottle on the floor and roll the bottle back and forth under your foot for 10 minutes. Do this at the end of each day and after activity. SETS & REPS: 10 mins FREQUENCY: Daily PLANTAR FASCIA MASSAGE Sitting, place a golf ball on the floor and roll the ball around under your foot concentrating on the tight, tender areas. SETS & REPS: 2-5 mins FREQUENCY: As needed © 2013 The Rehab Lab Limited. Used under license. No reproduction permitted without permission. www.therehablab.com PLANTAR FASCIITIS STAGE 1 PRONE GLUTEAL CONTRACTION Lie face-down and place your hands on your buttock muscles. Contract your gluteals, feeling the muscles tightening beneath your hands and hold for 5 seconds. Relax and repeat. SETS & REPS: 10 reps FREQUENCY: 1-2 x daily GLUTEAL STRETCH Sit on a chair and place your ankle on your opposite knee. With both hands, gently push down the knee of the crossed leg. Maintaining a straight back, bend forwards from the hips until you feel a stretch. Hold. SETS & REPS: 2 minute hold FREQUENCY: 1-2 x daily HAMSTRING STRETCH Place your heel on a knee-height table/chair with your knee slightly bent and tilt your pelvis forwards. While keeping your back straight, lean forwards until you feel a stretch in your hamstring. -

Plantar Fasciitis: a Degenerative Process (Fasciosis) Without Inflammation
CLINICAL PATHOLOGY Plantar Fasciitis A Degenerative Process (Fasciosis) Without Inflammation Harvey Lemont, DPM* Krista M. Ammirati, BS* Nsima Usen, MPH* The authors review histologic findings from 50 cases of heel spur surgery for chronic plantar fasciitis. Findings include myxoid degeneration with fragmentation and degeneration of the plantar fascia and bone marrow vascular ectasia. Histologic findings are presented to support the thesis that “plantar fasciitis” is a degenerative fasciosis without inflammation, not a fasciitis. These findings suggest that treatment regimens such as serial corticosteroid injections into the plantar fascia should be reevalu- ated in the absence of inflammation and in light of their potential to induce plantar fascial rupture. (J Am Podiatr Med Assoc 93(3): 234-237, 2003) Plantar fasciitis is presumed to be synonymous with occur with long-distance running may induce an in- inflammation of the plantar fascia. In fact, the suffix flammatory process, leading to fibrosis or degenera- “-itis” inherently implies an inflammatory disease. tion, and Sewell5 stated that the pain of plantar inflam- However, is plantar fasciitis really an inflammatory mation may sometimes be secondary to periosteal disorder? inflammation of the os calcis. Although authors writ- Plantar fasciitis is widely described in the litera- ing on the subject describe inflammation as being ture as having a multifactorial and widely disputed present in plantar fasciitis, they provide no objective etiology. Interestingly, in 1965, Lapidus and Guidotti,1 clinical or histologic evidence to support their claims. in their article entitled “Painful Heel,” stated that “the In addition, when photomicrographs are provided, name of painful heel is used deliberately in prefer- they are often mislabeled as showing inflammation. -

Understanding the First
CME / ORTHOTICS & BIOMECHANICS Goals and Objectives After reading this CME the practitioner will be able to: 1) Understand normal and abnormal function of the first ray with special emphasis on its integral role in medial longitudinal arch function and hypermobility. Understanding 2) Acquire knowledge of the various etiologic factors that result in first ray hypermobility. the First Ray 109 3) Appreciate its normal and abnormal motion along Here’s a review of its normal with its attendant bio and and abnormal function, identification, pathomechanics. and clinical significance. 4) Become familiar with vari- ous methods to subjectively and BY JOSEPH C D’AMICO, DPM objectively identify its presence. Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Con- tinuing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $26.00 per topic) or 2) per year, for the special rate of $210 (you save $50). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. You can also take this and other exams on the Internet at www.podiatrym.com/cme. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. 144. Other than those entities currently accepting CPME-approved credit, Podiatry Management cannot guarantee that these CME credits will be acceptable by any state licensing agency, hospital, managed care organization or other entity.