Volume 16 #4 October/December 2009
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Strážovské Vrchy Mts., Resort Podskalie; See P. 12)
a journal on biodiversity, taxonomy and conservation of fungi No. 7 March 2006 Tricholoma dulciolens (Strážovské vrchy Mts., resort Podskalie; see p. 12) ISSN 1335-7670 Catathelasma 7: 1-36 (2006) Lycoperdon rimulatum (Záhorská nížina Lowland, Mikulášov; see p. 5) Cotylidia pannosa (Javorníky Mts., Dolná Mariková – Kátlina; see p. 22) March 2006 Catathelasma 7 3 TABLE OF CONTENTS BIODIVERSITY OF FUNGI Lycoperdon rimulatum, a new Slovak gasteromycete Mikael Jeppson 5 Three rare tricholomoid agarics Vladimír Antonín and Jan Holec 11 Macrofungi collected during the 9th Mycological Foray in Slovakia Pavel Lizoň 17 Note on Tricholoma dulciolens Anton Hauskknecht 34 Instructions to authors 4 Editor's acknowledgements 4 Book notices Pavel Lizoň 10, 34 PHOTOGRAPHS Tricholoma dulciolens Vladimír Antonín [1] Lycoperdon rimulatum Mikael Jeppson [2] Cotylidia pannosa Ladislav Hagara [2] Microglossum viride Pavel Lizoň [35] Mycena diosma Vladimír Antonín [35] Boletopsis grisea Petr Vampola [36] Albatrellus subrubescens Petr Vampola [36] visit our web site at fungi.sav.sk Catathelasma is published annually/biannually by the Slovak Mycological Society with the financial support of the Slovak Academy of Sciences. Permit of the Ministry of Culture of the Slovak rep. no. 2470/2001, ISSN 1335-7670. 4 Catathelasma 7 March 2006 Instructions to Authors Catathelasma is a peer-reviewed journal devoted to the biodiversity, taxonomy and conservation of fungi. Papers are in English with Slovak/Czech summaries. Elements of an Article Submitted to Catathelasma: • title: informative and concise • author(s) name(s): full first and last name (addresses as footnote) • key words: max. 5 words, not repeating words in the title • main text: brief introduction, methods (if needed), presented data • illustrations: line drawings and color photographs • list of references • abstract in Slovak or Czech: max. -

Curriculum Vitae
Curriculum Vitae INFORMAZIONI PERSONALI Nome GIUSEPPE Cognome VENTURELLA Recapiti Dipartimento Scienze Agrarie e Forestali Telefono 329-6156064 E-mail [email protected] [email protected] FORMAZIONE TITOLI • Date 3 gennaio 2008 • Nome e tipo di istituto di istruzione o Facoltà di Agraria di Palermo - Decreto formazione Rettorale n°30 • Principali materie / abilità professionali Botanica Sistematica, Botanica forestale e oggetto dello studio micologia • Qualifica conseguita Conferma in ruolo a Professore Ordinario per il settore BIO/02 • Livello nella classificazione nazionale Professore Ordinario per il settore BIO/02 • Date 3 gennaio 2005 • Nome e tipo di istituto di istruzione o Facoltà di Agraria di Palermo- Decreto formazione Rettorale n°30 • Principali materie / abilità professionali Botanica Sistematica, Botanica forestale e oggetto dello studio micologia • Qualifica conseguita Nomina a Professore Straordinario per il settore BIO/02 • Livello nella classificazione nazionale Professore Straordinario per il settore BIO/ 02 • Date novembre 1992 – gennaio 2005 • Nome e tipo di istituto di istruzione o Facoltà di Agraria di Palermo formazione • Principali materie / abilità professionali Botanica Ambientale e Applicata, Botanica oggetto dello studio forestale e micologia • Qualifica conseguita Professore Associato gruppo E011 (BIO/03) • Livello nella classificazione nazionale Professore Associato gruppo E011 (BIO/ 03) • Date 1990 • Nome e tipo di istituto di istruzione o Corso di Laurea in Scienze Biologiche formazione -

Key Features for the Identification of the Fungi in This Guide
Further information Key features for the identifi cation Saprotrophic recycler fungi Books and References of the fungi in this guide Mushrooms. Roger Phillips (2006). Growth form. Fungi come in many different shapes and Fruit body colours. The different parts of the fruit body Collybia acervata Conifer Toughshank. Cap max. 5cm. Macmillan. Excellent photographs and descriptions including sizes. In this fi eld guide most species are the classic can be differently coloured and it is also important This species grows in large clusters often on the ground many species from pinewoods and other habitats. toadstool shape with a cap and stem but also included to remember that the caps sometimes change colour but possibly growing on buried wood. Sometimes there are are some that grow out of wood like small shelves or completely or as they dry out. Making notes or taking Fungi. Roy Watling and Stephen Ward (2003). several clusters growing ± in a ring. The caps are reddish brackets and others that have a coral- like shape. Take photographs can help you remember what they looked Naturally Scottish Series. Scottish Natural Heritage, Battleby, Perth. brown but dry out to a buff colour. The stems are smooth, note of whether the fungus is growing alone, trooping like when fresh. In some fungi the fl esh changes colour Good introduction to fungi in Scotland. and red brown and the gills are white and variably attached, or in a cluster. when it is damaged. Try cutting the fungus in half or Fungi. Brian Spooner and Peter Roberts (2005). adnate to free. Spore print white. -

Fungal Genomes Tell a Story of Ecological Adaptations
Folia Biologica et Oecologica 10: 9–17 (2014) Acta Universitatis Lodziensis Fungal genomes tell a story of ecological adaptations ANNA MUSZEWSKA Institute of Biochemistry and Biophysics, Polish Academy of Sciences, Pawinskiego 5A, 02-106 Warsaw, Poland E-mail: [email protected] ABSTRACT One genome enables a fungus to have various lifestyles and strategies depending on environmental conditions and in the presence of specific counterparts. The nature of their interactions with other living and abiotic elements is a consequence of their osmotrophism. The ability to degrade complex compounds and especially plant biomass makes them a key component of the global carbon circulation cycle. Since the first fungal genomic sequence was published in 1996 mycology has benefited from the technolgical progress. The available data create an unprecedented opportunity to perform massive comparative studies with complex study design variants targeted at all cellular processes. KEY WORDS: fungal genomics, osmotroph, pathogenic fungi, mycorrhiza, symbiotic fungi, HGT Fungal ecology is a consequence of osmotrophy Fungi play a pivotal role both in encountered as leaf endosymbionts industry and human health (Fisher et al. (Spatafora et al. 2007). Since fungi are 2012). They are involved in biomass involved in complex relationships with degradation, plant and animal infections, other organisms, their ecological fermentation and chemical industry etc. repertoire is reflected in their genomes. They can be present in the form of The nature of their interactions with other resting spores, motile spores, amebae (in organisms and environment is defined by Cryptomycota, Blastocladiomycota, their osmotrophic lifestyle. Nutrient Chytrydiomycota), hyphae or fruiting acquisition and communication with bodies. The same fungal species symbionts and hosts are mediated by depending on environmental conditions secreted molecules. -

Non-Wood Forest Products in Europe
Non-Wood Forest Products in Europe Ecologyand management of mushrooms, tree products,understory plants andanimal products Outcomes of theCOST Action FP1203 on EuropeanNWFPs Edited by HARALD VACIK, MIKE HALE,HEINRICHSPIECKER, DAVIDE PETTENELLA &MARGARIDA TOMÉ Bibliographicalinformation of Deutsche Nationalbibliothek [the German National Library] Deutsche Nationalbibliothek [the German National Library] hasregisteredthispublication in theGermanNationalBibliography. Detailed bibliographicaldatamay be foundonlineathttp: //dnb.dnb.de ©2020Harald Vacik Please cite this referenceas: Vacik, H.;Hale, M.;Spiecker,H.; Pettenella, D.;Tomé, M. (Eds)2020: Non-Wood Forest Products in Europe.Ecology andmanagementofmushrooms, tree products,understoryplantsand animal products.Outcomesofthe COST Action FP1203 on EuropeanNWFPs, BoD, Norderstedt,416p. Coverdesign, layout,produced andpublished by:BoD –Books on Demand GmbH, In de Tarpen 42,22848 Norderstedt ISBN:978-3-7526-7529-0 Content 5 1. Introduction.......................................................11 1.1Non-wood forest products.....................................11 1.2Providingevidencefor NWFP collection andusage within Europe ......................................14 1.3Outline of thebook...........................................15 1.4References ...................................................17 2. Identificationand ecologyofNWFPspecies........................19 2.1Introduction.................................................19 2.2 Theidentification of NWFP in Europe. ........................ -

80130Dimou7-107Weblist Changed
Posted June, 2008. Summary published in Mycotaxon 104: 39–42. 2008. Mycodiversity studies in selected ecosystems of Greece: IV. Macrofungi from Abies cephalonica forests and other intermixed tree species (Oxya Mt., central Greece) 1 2 1 D.M. DIMOU *, G.I. ZERVAKIS & E. POLEMIS * [email protected] 1Agricultural University of Athens, Lab. of General & Agricultural Microbiology, Iera Odos 75, GR-11855 Athens, Greece 2 [email protected] National Agricultural Research Foundation, Institute of Environmental Biotechnology, Lakonikis 87, GR-24100 Kalamata, Greece Abstract — In the course of a nine-year inventory in Mt. Oxya (central Greece) fir forests, a total of 358 taxa of macromycetes, belonging in 149 genera, have been recorded. Ninety eight taxa constitute new records, and five of them are first reports for the respective genera (Athelopsis, Crustoderma, Lentaria, Protodontia, Urnula). One hundred and one records for habitat/host/substrate are new for Greece, while some of these associations are reported for the first time in literature. Key words — biodiversity, macromycetes, fir, Mediterranean region, mushrooms Introduction The mycobiota of Greece was until recently poorly investigated since very few mycologists were active in the fields of fungal biodiversity, taxonomy and systematic. Until the end of ’90s, less than 1.000 species of macromycetes occurring in Greece had been reported by Greek and foreign researchers. Practically no collaboration existed between the scientific community and the rather few amateurs, who were active in this domain, and thus useful information that could be accumulated remained unexploited. Until then, published data were fragmentary in spatial, temporal and ecological terms. The authors introduced a different concept in their methodology, which was based on a long-term investigation of selected ecosystems and monitoring-inventorying of macrofungi throughout the year and for a period of usually 5-8 years. -
Newsletter of Jun
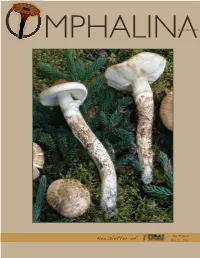
V OMPHALINISSN 1925-1858 Vol. V, No 6 Newsletter of Jun. 21, 2014 OMPHALINA OMPHALINA, newsletter of Foray Newfoundland & Labrador, has no fi xed schedule of publication, and no promise to appear again. Its primary purpose is to serve as a conduit of information to registrants of the upcoming foray and secondarily as a communications tool with members. Issues of OMPHALINA are archived in: is an amateur, volunteer-run, community, Library and Archives Canada’s Electronic Collection <http://epe. not-for-profi t organization with a mission to lac-bac.gc.ca/100/201/300/omphalina/index.html>, and organize enjoyable and informative amateur Centre for Newfoundland Studies, Queen Elizabeth II Library mushroom forays in Newfoundland and (printed copy also archived) <http://collections.mun.ca/cdm4/ description.php?phpReturn=typeListing.php&id=162>. Labrador and disseminate the knowledge gained. The content is neither discussed nor approved by the Board of Directors. Therefore, opinions expressed do not represent the views of the Board, Webpage: www.nlmushrooms.ca the Corporation, the partners, the sponsors, or the members. Opinions are solely those of the authors and uncredited opinions solely those of the Editor. ADDRESS Foray Newfoundland & Labrador Please address comments, complaints, contributions to the self-appointed Editor, Andrus Voitk: 21 Pond Rd. Rocky Harbour NL seened AT gmail DOT com, A0K 4N0 CANADA … who eagerly invites contributions to OMPHALINA, dealing with any aspect even remotely related to mushrooms. E-mail: info AT nlmushrooms DOT ca Authors are guaranteed instant fame—fortune to follow. Authors retain copyright to all published material, and BOARD OF DIRECTORS CONSULTANTS submission indicates permission to publish, subject to the usual editorial decisions. -

Naturstoffe Im Chemieunterricht: Chemie Mit Pilzen
Neue experimentelle Designs zum Thema Naturstoffe im Chemieunterricht: Chemie mit Pilzen DISS,RTATI.N 0ur ,rlangung des akademischen Grades doctor rerum naturalium 1Dr. rer. nat.2 vorgelegt dem Rat der Chemisch -Geowissenschaftlichen Fakultt der Friedrich-Schiller-Universitt Jena von Jan-Markus Teuscher ge oren am 11.08.1972 in (arl-Mar)-Stadt Gutachter: 1: Prof. Dr. Volker Woest, Arbeitsgruppe Chemiedidaktik 2: Dr. Dieter Weiß, Institut für Organische und Makromolekulare Chemie Tag der öffentlichen Verteidigung: 25.05.2011 Inhaltsverzeichnis S e i t e 3 Inhaltsverzeichnis Abbildungsverzeichnis ............................................................................................................. 5 Tabellenverzeichnis .................................................................................................................. 5 1 Einleitung und Zielsetzung ................................................................................................. 7 2 Biologische Grundlage ....................................................................................................... 9 2.1 Betrachtung der Pilze im Wandel der Zeit .................................................................. 9 2.1.1 Vorgeschichtliche Zeit ......................................................................................... 9 2.1.2 Europäisches Altertum – Anfänge der Naturwissenschaft ................................... 9 2.1.3 Mittelalterliche Scholastik ................................................................................. -

Research Article the Role of Polyphenols, Β-Carotene, and Lycopene in the Antioxidative Action of the Extracts of Dried, Edible Mushrooms
Hindawi Publishing Corporation Journal of Nutrition and Metabolism Volume 2010, Article ID 173274, 9 pages doi:10.1155/2010/173274 Research Article The Role of Polyphenols, β-Carotene, and Lycopene in the Antioxidative Action of the Extracts of Dried, Edible Mushrooms A. Robaszkiewicz,1 G. Bartosz,1, 2 M. Ławrynowicz,3 and M. Soszynski´ 1 1 Department of Molecular Biophysics, University of Ł´od´z, Banacha 12/16, 90-237 Ł´od´z, Poland 2 Department of Biochemistry and Cell Biology, University of Rzesz´ow, St. Pigonia 6, 35-959 Rzesz´ow, Poland 3 Department of Mycology, University of Ł´od´z, Banacha 12/16, 90-237 Ł´od´z, Poland Correspondence should be addressed to A. Robaszkiewicz, [email protected] Received 17 August 2010; Accepted 16 November 2010 Academic Editor: Parul Christian Copyright © 2010 A. Robaszkiewicz et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. One of the nutritional benefits of mushrooms is the presence of bioactive secondary metabolites which have been reported to exert various beneficial effects in vivo. Therefore, we selected thirteen frequently consumed species of Polish mushrooms and determined the concentration of polyphenols, flavonoids, β-carotene, and lycopene in aqueous and methanolic extracts of dried fruiting bodies as well as their reducing power and ability to scavenge ABTS cation radical. We found that the concentration of antioxidants is different in different species and in various parts of the fruiting body of mushrooms. -

Comment on “Study of Biological Activity of Tricholoma Equestre Fruiting Bodies and Their Safety for Human”
European Food Research and Technology https://doi.org/10.1007/s00217-019-03236-w SHORT COMMUNICATION Comment on “Study of biological activity of Tricholoma equestre fruiting bodies and their safety for human” Piotr Rzymski1 · Piotr Klimaszyk2 · Denis Benjamin3 Received: 18 December 2018 / Accepted: 3 January 2019 © The Author(s) 2019 Keywords Mushrooms · Toxicity · Tricholoma equestre Dear Editor, countries (e.g., France, Spain, and Italy) to officially declare T. equestre as poisonous, releasing warnings to avoid its con- The paper by Muszyńska et al. [1] entitled “Study of biologi- sumption. Prior to this, it had a long -history of consumption cal activity of Tricholoma equestre fruiting bodies and their in many countries with no anecdotal or scientific evidence safety for human” published in the journal of European Food of toxic effects. It is still considered edible and widely con- Research and Technology (https ://doi.org/10.1007/s0021 sumed in regions such as Poland [8]. As shown in a recent 7-018-3134-0) presents the results of a study on the compo- study, more than half of mushroom foragers in this country sition of T. equestre (syn. T. flavovirens, and syn. T. auratum) have consumed T. equestre at least once in their lifetime [9]. and in vitro anti-microbial and antioxidant activities of this This questionnaire survey and additional analysis of Polish mushroom. As reported, T. equestre can be a source of some registry of mushroom toxicity demonstrate that no rhabdo- essential minerals and has a favorable ratio of unsaturated- myolysis was reported in the last decade and that only mild to-saturated fatty acids, while its extracts exhibit antioxidant gastrointestinal effects were noted, at a lower frequency than effects (as shown in DPPH assay) at levels comparable to for other well-established edible wild mushrooms, such as other mushroom species, but weak anti-microbial activities. -

Ukrbotj-2016-73-4-382.Pdf
doi:10.15407/ukrbotj73.04.382 Я.М.МАКАРЕНКО ІнститутботанікиіменіМ.Г.ХолодногоНАНУкраїни вул.Терещенківська,2,м.Київ,01004,Україна ПолтавськийнаціональнийпедагогічнийуніверситетіменіВ.Г.Короленка вул.Остроградського,2,м.Полтава,36000,Україна [email protected] ПЕРША ЗНАХІДКА В УКРАЇНІ AGARICUS IODOSMUS (AGARICACEAE) MakarenkoYa.M. Тhe first record of Agaricus iodosmus (Agaricaceae) in Ukraine. Ukr.Bot.J.,2016,73(4):382–384. M.G.KholodnyInstituteofBotany,NationalAcademyofSciencesofUkraine 2,TereshchenkivskaStr.,Kyiv,01004,Ukraine V.G.KorolenkoPoltavaNationalPedagogicalUniversity 2,OstrohradskohoStr.,Poltava,36000,Ukraine Abstract. Agaricus iodosmusisreportedasanewspeciesofagaricfungiforUkraine.Previously,thisspecieswasalso knownasA. xanthodermusvar.pilatianusandA. pilatianus,notrecordedinUkraine.Thedescriptionofthespeciesis givenanditslocalitywithintheLeftBankForestSteppeisprovided(PoltavaRegion,ShyshakyDistrict,leftbankofthe PselRiver,Yareskyvillage).Morphologicalcharactersof A. iodosmus andrelatedspeciesarediscussed. Key words:Basidiomycota, Agaricales,Xanthodermatei,PselRiverbasin,PoltavaRegion Протягом 2012–2015 рр. ми вивчали агарикоїд режного Лісостепу, вважаємо за доцільне навести нігриби(Agaricales, Boletalesта Russulales)басейну йогоповнийопистаілюстрацію(рисунок). р. Псел (Полтавська обл.) з метою з'ясування їх Agaricus iodosmus Heinem.,Bull.Soc.Mycol.France -

Abstracts of Journals Received in the Library April-June 2011 Journals Abstracted
Abstracts of Journals Received in the Library April-June 2011 Journals Abstracted Cahiers Mycologiques Nantais – No 23, June 2011 Mykologicke Listy – No 116, 2011 Mushroom, - Issue 106, Vol 28, No 2-3, Spring-Summer 2010 Schweizerische Zeitschrift für Pilzkunde - Vol. 89, No. 1, 15th. February 2011 Schweizerische Zeitschrift für Pilzkunde vol. 89, no. 3, 15 June 2011 Annales Botanici Fennici – Vol 48, No 3, June 2011 Mycological Research Information about recent issues (including free access to contents lists and abstracts of published papers) can be found on the Elsevier website at www.elsevier.com/locate/mycres Cahiers Mycologiques Nantais – No 23, June 2011 Abstractor – Anne Andrews Ribollet P (pp. 3-6) [French] Descriiption of Pezoloma marchantiae an inoperculate ascomycete growing on the liverwort Marchantia polymorpha although its exact relationship with it is not fully understood. It occurs on all parts of the liverwort. The hairs on the edge of the f/b may fall off with age. There is a strong reaction to |Cresyl Blue. The species is probably not rare if sought in the right place and occurs in several European countries and in North America. Illustrated with colour photos and b/w drawings (6 refs.) Larue P (pp. 7-9) [French] Description of Psathyrella melanthina found on woody debris of Poplar. This species looks more like a Tricholoma at first sight and has beige gills tinged with pink making it difficult to recognise as a Psathyrella. Illustrated with colour photos of f/bs, spores and habitat and b/w drawings. (4 refs.) Chereau R & Larue P (pp. 10-21) [French] Descriptions of five corticioid fungi collected in good condition in winter:- Serpula lacrimans; S.