List of 219 Inns, Including E75 and T50 Marking
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers with Topical Pharmaceutical Agents
Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Author Watts, Annabelle M, Cripps, Allan W, West, Nicholas P, Cox, Amanda J Published 2019 Journal Title FRONTIERS IN PHARMACOLOGY Version Version of Record (VoR) DOI https://doi.org/10.3389/fphar.2019.00294 Copyright Statement © Frontiers in Pharmacology 2019. The attached file is reproduced here in accordance with the copyright policy of the publisher. Please refer to the journal's website for access to the definitive, published version. Downloaded from http://hdl.handle.net/10072/386246 Griffith Research Online https://research-repository.griffith.edu.au fphar-10-00294 March 27, 2019 Time: 17:52 # 1 REVIEW published: 29 March 2019 doi: 10.3389/fphar.2019.00294 Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Annabelle M. Watts1*, Allan W. Cripps2, Nicholas P. West1 and Amanda J. Cox1 1 Menzies Health Institute Queensland, School of Medical Science, Griffith University, Southport, QLD, Australia, 2 Menzies Health Institute Queensland, School of Medicine, Griffith University, Southport, QLD, Australia Allergic rhinitis (AR) is a chronic upper respiratory disease estimated to affect between 10 and 40% of the worldwide population. The mechanisms underlying AR are highly complex and involve multiple immune cells, mediators, and cytokines. As such, the development of a single drug to treat allergic inflammation and/or symptoms is confounded by the complexity of the disease pathophysiology. Complete avoidance of allergens that trigger AR symptoms is not possible and without a cure, the available therapeutic options are typically focused on achieving symptomatic relief. -

Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis
Journal of Allergy Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis Guest Editors: Ralph Mösges, Carlos E. Baena-Cagnani, and Desiderio Passali Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis Journal of Allergy Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis Guest Editors: Ralph Mosges,¨ Carlos E. Baena-Cagnani, and Desiderio Passali Copyright © 2014 Hindawi Publishing Corporation. All rights reserved. This is a special issue published in “Journal of Allergy.” All articles are open access articles distributed under the Creative Commons At- tribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Editorial Board William E. Berger, USA Alan P. Knutsen, USA Fabienne Ranc, France Kurt Blaser, Switzerland Marek L. Kowalski, Poland Anuradha Ray, USA Eugene R. Bleecker, USA Ting Fan Leung, Hong Kong Harald Renz, Germany JandeMonchy,TheNetherlands Clare M Lloyd, UK Nima Rezaei, Iran Frank Hoebers, The Netherlands Redwan Moqbel, Canada Robert P. Schleimer, USA StephenT.Holgate,UK Desiderio Passali, Italy Massimo Triggiani, Italy Sebastian L. Johnston, UK Stephen P. Peters, USA Hugo Van Bever, Singapore Young J. Juhn, USA David G. Proud, Canada Garry Walsh, United Kingdom Contents Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis,RalphMosges,¨ Carlos E. Baena-Cagnani, and Desiderio Passali Volume 2014, Article ID 416236, 2 pages Clinical Efficacy of a Spray Containing Hyaluronic Acid and Dexpanthenol after Surgery in the Nasal Cavity (Septoplasty, Simple Ethmoid Sinus Surgery, and Turbinate Surgery), Ina Gouteva, Kija Shah-Hosseini, and Peter Meiser Volume 2014, Article ID 635490, 10 pages The Effectiveness of Acupuncture Compared to Loratadine in Patients Allergic to House Dust ,Mites Bettina Hauswald, Christina Dill, Jurgen¨ Boxberger, Eberhard Kuhlisch, Thomas Zahnert, and Yury M. -

Crohn's & Colitis Program, Patient Information Guide
Inflammatory Bowel Disease Program Patient Information Guide Page # Contents ..........................................................................................................................................1 Welcome! Welcome Letter ....................................................................................................................3 Important Things to Know Up Front ....................................................................................4 Meet Your Crohn’s & Colitis Team .....................................................................................6 How to Contact Us Crohn’s & Colitis Clinic Schedule .....................................................................................11 Physician and Nurse Contact Information..........................................................................12 Appointment Scheduling and Other Contact Information..................................................13 The Basics of Inflammatory Bowel Disease (IBD) Basic Information about Inflammatory Bowel Disease (IBD) ...........................................14 Frequently Asked Questions about Inflammatory Bowel Disease (IBD) ..........................18 Testing in IBD Colonoscopy and Flexible Sigmoidoscopy ........................................................................20 Upper Endoscopy ...............................................................................................................21 Capsule Endoscopy and Deep Enteroscopy .......................................................................22 -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

Inflammatory Bowel Disease Agents
Therapeutic Class Overview Inflammatory Bowel Disease Agents INTRODUCTION • Inflammatory bowel disease (IBD) is a spectrum of chronic idiopathic inflammatory intestinal conditions that cause gastrointestinal symptoms including diarrhea, abdominal pain, bleeding, fatigue, and weight loss. The exact cause of IBD is unknown; however, proposed etiologies involve a combination of infectious, genetic, and lifestyle factors (Bernstein et al 2015, Peppercorn 2019[a], Peppercorn 2020[c]). • Complications of IBD include hemorrhage, rectal fissures, fistulas, peri-rectal and intra-abdominal abscesses, and colon cancer. Possible extra-intestinal complications include hepatobiliary complications, anemia, arthritis and arthralgias, uveitis, skin lesions, and mood and anxiety disorders (Bernstein et al 2015). • Ulcerative colitis (UC) and Crohn’s disease (CD) are 2 forms of IBD that differ in pathophysiology and presentation; as a result of these differences, the approach to the treatment of each condition often differs (Peppercorn 2019[a]). • UC is characterized by recurrent episodes of inflammation of the mucosal layer of the colon. The inflammation, limited to the mucosa, commonly involves the rectum and may extend in a proximal and continuous fashion to affect other parts of the colon. The hallmark clinical symptom is an inflamed rectum with symptoms of urgency, bleeding, and tenesmus (Peppercorn 2020[c], Rubin et al 2019). • CD can involve any part of the gastrointestinal tract and is characterized by transmural inflammation and “skip areas.” Transmural inflammation may lead to fibrosis, strictures, sinus tracts, and fistulae (Peppercorn 2019[b]). • The immune system is known to play a critical role in the underlying pathogenesis of IBD. It is suggested that abnormal responses of both innate and adaptive immunity mechanisms induce aberrant intestinal tract inflammation in IBD patients (Geremia et al 2014). -

Interactions Medicamenteuses Index Des Classes Pharmaco
INTERACTIONS MEDICAMENTEUSES INDEX DES CLASSES PHARMACO-THERAPEUTIQUES Mise à jour avril 2006 acides biliaires (acide chenodesoxycholique, acide ursodesoxycholique) acidifiants urinaires adrénaline (voie bucco-dentaire ou sous-cutanée) (adrenaline alcalinisants urinaires (acetazolamide, sodium (bicarbonate de), trometamol) alcaloïdes de l'ergot de seigle dopaminergiques (bromocriptine, cabergoline, lisuride, pergolide) alcaloïdes de l'ergot de seigle vasoconstricteurs (dihydroergotamine, ergotamine, methylergometrine) alginates (acide alginique, sodium et de trolamine (alginate de)) alphabloquants à visée urologique (alfuzosine, doxazosine, prazosine, tamsulosine, terazosine) amidons et gélatines (gelatine, hydroxyethylamidon, polygeline) aminosides (amikacine, dibekacine, gentamicine, isepamicine, kanamycine, netilmicine, streptomycine, tobramycine) amprénavir (et, par extrapolation, fosamprénavir) (amprenavir, fosamprenavir) analgésiques morphiniques agonistes (alfentanil, codeine, dextromoramide, dextropropoxyphene, dihydrocodeine, fentanyl, hydromorphone, morphine, oxycodone, pethidine, phenoperidine, remifentanil, sufentanil, tramadol) analgésiques morphiniques de palier II (codeine, dextropropoxyphene, dihydrocodeine, tramadol) analgésiques morphiniques de palier III (alfentanil, dextromoramide, fentanyl, hydromorphone, morphine, oxycodone, pethidine, phenoperidine, remifentanil, sufentanil) analogues de la somatostatine (lanreotide, octreotide) androgènes (danazol, norethandrolone, testosterone) anesthésiques volatils halogénés -

Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy Using Machine Learning
Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy using Machine Learning Kate Wang et al. Supplemental Table S1. Drugs selected by Pharmacophore-based, ML-based and DL- based search in the FDA-approved drugs database Pharmacophore WEKA TF 1-Palmitoyl-2-oleoyl-sn-glycero-3- 5-O-phosphono-alpha-D- (phospho-rac-(1-glycerol)) ribofuranosyl diphosphate Acarbose Amikacin Acetylcarnitine Acetarsol Arbutamine Acetylcholine Adenosine Aldehydo-N-Acetyl-D- Benserazide Acyclovir Glucosamine Bisoprolol Adefovir dipivoxil Alendronic acid Brivudine Alfentanil Alginic acid Cefamandole Alitretinoin alpha-Arbutin Cefdinir Azithromycin Amikacin Cefixime Balsalazide Amiloride Cefonicid Bethanechol Arbutin Ceforanide Bicalutamide Ascorbic acid calcium salt Cefotetan Calcium glubionate Auranofin Ceftibuten Cangrelor Azacitidine Ceftolozane Capecitabine Benserazide Cerivastatin Carbamoylcholine Besifloxacin Chlortetracycline Carisoprodol beta-L-fructofuranose Cilastatin Chlorobutanol Bictegravir Citicoline Cidofovir Bismuth subgallate Cladribine Clodronic acid Bleomycin Clarithromycin Colistimethate Bortezomib Clindamycin Cyclandelate Bromotheophylline Clofarabine Dexpanthenol Calcium threonate Cromoglicic acid Edoxudine Capecitabine Demeclocycline Elbasvir Capreomycin Diaminopropanol tetraacetic acid Erdosteine Carbidopa Diazolidinylurea Ethchlorvynol Carbocisteine Dibekacin Ethinamate Carboplatin Dinoprostone Famotidine Cefotetan Dipyridamole Fidaxomicin Chlormerodrin Doripenem Flavin adenine dinucleotide -

Rhinitis - Allergic (1 of 15)
Rhinitis - Allergic (1 of 15) 1 Patient presents w/ signs & symptoms of rhinitis 2 • Consider other classifi cations of rhinitis DIAGNOSIS No - Please see Rhinitis Is allergic rhinitis - Nonallergic disease confi rmed? management chart Yes 3 ASSESS DURATION & SEVERITY OF ALLERGIC RHINITIS A Non-pharmacological therapy • Allergen avoidance • Patient education VAS <5 VAS ≥5 B Pharmacological therapy B Pharmacological therapy • Antihistamines (oral/nasal), &/or • Corticosteroids (nasal), w/ or without • Corticosteroids (nasal), or • Antihistamines (nasal), or • Cromone (nasal), or • LTRA • Leukotriene receptor antagonists (LTRA)MIMS TREATMENT © See next page Specifi cally for patients w/ asthma Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B167 © MIMS Pediatrics 2020 Rhinitis - Allergic (2 of 15) Previously treated symptomatic Previously treated symptomatic patient (VAS <5) on antihistamines patient (VAS ≥5) on intensifi ed (oral/nasal) &/or corticosteroids (nasal) therapy w/ corticosteroids (nasal) w/ or without antihistamines (nasal) Intermittent Persistent symptoms, symptoms or without allergen w/ allergen exposure exposure B Pharmacological therapy B Pharmacological therapy • Step down or discontinue therapy • Continue or step up therapy Untreated REASSESS DISEASE SEVERITY VAS symptomatic patient DAILY UP TO DAY 3 (VAS <5 or ≥5) 4 CONTINUE Yes THERAPY & STEP EVALUATION VAS <5 DOWN THERAPY1 Improvement of symptoms? No VAS ≥5 B Pharmacological therapy • Step-up therapy REASSESS DISEASE SEVERITY MIMSVAS DAILY UP TO DAY 7 4 Yes EVALUATION VAS <5 Improvement of symptoms? No TREATMENT © VAS ≥5 See next page Continue therapy if symptomatic; consider step-down or discontinuation of therapy if symptoms subside Not all products are available or approved for above use in all countries. -

The Efficacy of Probiotics, Prebiotic Inulin-Type Fructans, and Synbiotics in Human Ulcerative Colitis: a Systematic Review and Meta-Analysis
Supplementary Materials and Data of Review: The Efficacy of Probiotics, Prebiotic Inulin-Type Fructans, and Synbiotics in Human Ulcerative Colitis: A Systematic Review and Meta-Analysis Supplementary Data S1 Search strategy Only clinical trial publications and human filters were used in the literature search performed in PUBMED. The studies were searched using the terms “ulcerative colitis” in combination with “probiotic”, “synbiotic”, and “inflammatory bowel disease” in combination with “prebiotic”, “inulin”, “FOS” and “fructo-oligosaccharides”. The search in SCOPUS was performed using combinations of the terms “ulcerative colitis” AND “inulin” limited to document types “Article”. Another search used “ulcerative colitis” AND “probiotic” AND “human” limited to document type “Article” and the subareas “Medicine”, “Immunology and Microbiology” and “Health Professions” and the exact key words “Controlled Study”, “Clinical Article”, “Clinical Trials”, “Controlled Clinical Trial” and “Double-Blind Method”. An additional search using the combinations “ulcerative colitis” AND “synbiotic” AND “human” limited to document type “Article” and excluding the exact key word “Crohn Disease”. In all cases, the search was limited to the languages “Spanish” and “English” Supplementary Table S1 Risk of bias of selected studies and and data data bias bias of generation generation assessment) reporting outcome concealment sources (participants personnel) personnel) Sequence (outcome Selective Other Allocation Incomplete Blinding Random Blinding Matsuoka et al. 2018 ? + + + + + + Tamaki et al. 2016 ? + + ? - ? + Yoshimatsu et al. 2015 ? ? + ? - + + Petersen et al. 2014 ? + + ? + + + Groeger et al. 2013 - - + ? - ? + Oliva et al. 2012 + + + ? - + + Wildt et al. 2011 ? + + ? + + + Tursi et al. 2010 ? + + ? + ? + Matthes et al. 2010 ? + + ? - + + Ng et al. 2010 ? - + ? + ? + Sood et al. 2009 + + + ? - ? + Miele et al. 2009 + + + ? - ? + Furrie et al. -

Stems for Nonproprietary Drug Names
USAN STEM LIST STEM DEFINITION EXAMPLES -abine (see -arabine, -citabine) -ac anti-inflammatory agents (acetic acid derivatives) bromfenac dexpemedolac -acetam (see -racetam) -adol or analgesics (mixed opiate receptor agonists/ tazadolene -adol- antagonists) spiradolene levonantradol -adox antibacterials (quinoline dioxide derivatives) carbadox -afenone antiarrhythmics (propafenone derivatives) alprafenone diprafenonex -afil PDE5 inhibitors tadalafil -aj- antiarrhythmics (ajmaline derivatives) lorajmine -aldrate antacid aluminum salts magaldrate -algron alpha1 - and alpha2 - adrenoreceptor agonists dabuzalgron -alol combined alpha and beta blockers labetalol medroxalol -amidis antimyloidotics tafamidis -amivir (see -vir) -ampa ionotropic non-NMDA glutamate receptors (AMPA and/or KA receptors) subgroup: -ampanel antagonists becampanel -ampator modulators forampator -anib angiogenesis inhibitors pegaptanib cediranib 1 subgroup: -siranib siRNA bevasiranib -andr- androgens nandrolone -anserin serotonin 5-HT2 receptor antagonists altanserin tropanserin adatanserin -antel anthelmintics (undefined group) carbantel subgroup: -quantel 2-deoxoparaherquamide A derivatives derquantel -antrone antineoplastics; anthraquinone derivatives pixantrone -apsel P-selectin antagonists torapsel -arabine antineoplastics (arabinofuranosyl derivatives) fazarabine fludarabine aril-, -aril, -aril- antiviral (arildone derivatives) pleconaril arildone fosarilate -arit antirheumatics (lobenzarit type) lobenzarit clobuzarit -arol anticoagulants (dicumarol type) dicumarol -

National Quality Forum
NQF #PSM-030-10 NATIONAL QUALITY FORUM Measure Evaluation 4.1 January 2010 This form contains the measure information submitted by stewards. Blank fields indicate no information was provided. Attachments also may have been submitted and are provided to reviewers. The sub-criteria and most of the footnotes from the evaluation criteria are provided in Word comments and will appear if your cursor is over the highlighted area (or in the margin if your Word program is set to show revisions in balloons). Hyperlinks to the evaluation criteria and ratings are provided in each section. TAP/Workgroup (if utilized): Complete all yellow highlighted areas of the form. Evaluate the extent to which each sub-criterion is met. Based on your evaluation, summarize the strengths and weaknesses in each section. Note: If there is no TAP or workgroup, the SC also evaluates the sub-criteria (yellow highlighted areas). Steering Committee: Complete all pink highlighted areas of the form. Review the workgroup/TAP assessment of the sub-criterion, noting any areas of disagreement; then evaluate the extent to which each major criterion is met; and finally, indicate your recommendation for the endorsement. Provide the rationale for your ratings. Evaluation ratings of the extent to which the criteria are met C = Completely (unquestionably demonstrated to meet the criterion) P = Partially (demonstrated to partially meet the criterion) M = Minimally (addressed BUT demonstrated to only minimally meet the criterion) N = Not at all (NOT addressed; OR incorrectly addressed; OR demonstrated to NOT meet the criterion) NA = Not applicable (only an option for a few sub-criteria as indicated) (for NQF staff use) NQF Review #: PSM-030-10 NQF Project: Patient Safety Measures MEASURE DESCRIPTIVE INFORMATION De.1 Measure Title: Patient(s) with inflammatory bowel disease taking methotrexate, sulfasalazine, mercaptopurine, or azathioprine that had a CBC in last 3 reported months. -
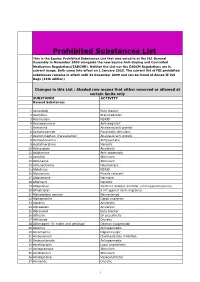
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR).