Background and Anatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anklyosed Spine: Fractures in DISH and Anklyosing Spondylitis
The Anklyosed Spine: Fractures in DISH and Anklyosing Spondylitis Lee F. Rogers, MD ACCR, Oct 26, 2012 Dallas, Texas Diffuse idiopathic skeletal hyperostosis (DISH) and ankylosing spondylitis (AS) are the most common diseases associated with spinal ankylosis. While they share the characteristic of ankylosis they are, in fact two separate diseases with distinct clinical, pathologic, and radiologic features. DISH: Diffuse idiopathic skeletal hyperostosis is a disease of older persons characterized by extensive ossification of the paraspinal ligaments anteriorly and laterally, bridging the intervening disc spaces. Bony bridging may be continuous or discontinuous. The anterior cortex of the vertebral body can be seen within the ossification. These findings are much more pronounced in the thoracic and lower cervical spine than in the lumbar area. Minor expressions of this disorder are commonly encountered in the mid-dorsal spine on lateral views of the chest. DISH characteristically spares the SI joints. The SI joints remain patent and clearly visible on radiographs or CT even in the presence of extensive disease in the thoracolumbar and cervical spine. DISH is also characterized by enthesopathy; ossification of ligaments or tendon insertions, forming so-called entheses. These appear as whiskering of the iliac crest, ischial tuberosites and greater trochanters. The radiographic appearance bears a superficial resemblance to that of AS. In DISH the spinal ossification is very irregular and unlike the thin, vertical syndesmophytes see in AS. The relative absence of changes in the lumbosacral spine, the patency of the SI joints, and absence of ankylosis of the facet and costovertebral joints should allow differentiation of DISH from AS. -

Ligaments of the Costovertebral Joints Including Biomechanics, Innervations, and Clinical Applications: a Comprehensive Review W
Open Access Review Article DOI: 10.7759/cureus.874 Ligaments of the Costovertebral Joints including Biomechanics, Innervations, and Clinical Applications: A Comprehensive Review with Application to Approaches to the Thoracic Spine Erfanul Saker 1 , Rachel A. Graham 2 , Renee Nicholas 3 , Anthony V. D’Antoni 2 , Marios Loukas 1 , Rod J. Oskouian 4 , R. Shane Tubbs 5 1. Department of Anatomical Sciences, St. George's University School of Medicine, Grenada, West Indies 2. Department of Anatomy, The Sophie Davis School of Biomedical Education 3. Department of Physical Therapy, Samford University 4. Neurosurgery, Complex Spine, Swedish Neuroscience Institute 5. Neurosurgery, Seattle Science Foundation Corresponding author: Erfanul Saker, [email protected] Abstract Few studies have examined the costovertebral joint and its ligaments in detail. Therefore, the following review was performed to better elucidate their anatomy, function and involvement in pathology. Standard search engines were used to find studies concerning the costovertebral joints and ligaments. These often- overlooked ligaments of the body serve important functions in maintaining appropriate alignment between the ribs and spine. With an increasing interest in minimally invasive approaches to the thoracic spine and an improved understanding of the function and innervation of these ligaments, surgeons and clinicians should have a good working knowledge of these structures. Categories: Neurosurgery, Orthopedics, Rheumatology Keywords: costovertebral joint, spine, anatomy, thoracic Introduction And Background The costovertebral joint ligaments are relatively unknown and frequently overlooked anatomical structures [1]. Although small and short in size, they are abundant, comprising 108 costovertebral ligaments in the normal human thoracic spine, and they are essential to its stability and function [2-3]. -

Chapter 21 Fractures of the Upper Thoracic Spine: Approaches and Surgical Management
Chapter 21 Fractures of the Upper Thoracic Spine: Approaches and Surgical Management Sean D Christie, M.D., John Song, M.D., and Richard G Fessler, M.D., Ph.D. INTRODUCTION Fractures occurring in the thoracic region account for approximately 17 to 23% of all traumatic spinal fractures (1), with 22% of traumatic spinal fractures occurring between T1 and T4 (16). More than half of these fractures result in neurological injury, and almost three-quarters of those impaired suffer from complete paralysis. Obtaining surgical access to the anterior vertebral elements of the upper thoracic vertebrae (T1–T6) presents a unique anatomic challenge. The thoracic cage, which narrows significantly as it approaches the thoracic inlet, has an intimate association between the vertebral column and the superior mediastinal structures. The supraclavicular, transmanubrial, transthoracic, and lateral parascapular extrapleural approaches each provide access to the anterior vertebral elements of the upper thoracic vertebrae. However, each of these approaches has distinct advantages and disadvantages and their use should be tailored to each individual patient’s situation. This chapter reviews these surgical approaches. Traditional posterior approaches are illustrated in Figure 21.1, but will not be discussed in depth here. ANATOMIC CONSIDERATIONS AND STABILITY The upper thoracic spine possesses unique anatomic and biomechanical properties. The anterior aspects of the vertebral bodies are smaller than the posterior aspects, which contribute to the physiological kyphosis present in this region of the spine. Furthermore, this orientation results in a ventrally positioned axis of rotation, predisposing this region to compression injuries. The combination and interaction of the vertebral bodies, ribs, and sternum increase the inherent biomechanical stability of this segment of the spine to 2 to 3 times that of the thoracolumbar junction. -

Canine Thoracic Costovertebral and Costotransverse Joints Three Case Reports of Dysfunction and Manual Therapy Guidelines for A
Topics in Compan An Med 29 (2014) 1–5 Topical review Canine Thoracic Costovertebral and Costotransverse Joints: Three Case Reports of Dysfunction and Manual Therapy Guidelines for Assessment and Treatment of These Structures Laurie Edge-Hughes, BScPT, MAnimSt (Animal Physiotherapy), CAFCI, CCRTn Keywords: The costovertebral and costotransverse joints receive little attention in research. However, pain costovertebral associated with rib articulation dysfunction is reported to occur in human patients. The anatomic costotransverse structures of the canine rib joints and thoracic spine are similar to those of humans. As such, it is ribs physical therapy proposed that extrapolation from human physical therapy practice could be used for the assessment and rehabilitation treatment of the canine patient with presumed rib joint pain. This article presents 3 case studies that manual therapy demonstrate signs of rib dysfunction and successful treatment using primarily physical therapy manual techniques. General assessment and select treatment techniques are described. & 2014 Elsevier Inc. All rights reserved. The Canine Fitness Centre Ltd, Calgary, Alberta, Canada nAddress reprint requests to Laurie Edge-Hughes, BScPT, MAnimSt (Animal Physiotherapy), CAFCI, CCRT, The Canine Fitness Centre Ltd, 509—42nd Ave SE, Calgary, Alberta, Canada T2G 1Y7 E-mail: [email protected] The articular structures of the thorax comprise facet joints, the erect spine and further presented that in reviewing the literature, intervertebral disc, and costal joints. Little research has been they were unable to find mention of natural development of conducted on these joints in human or animal medicine. However, idiopathic scoliosis in quadrupeds; however, there are reports of clinical case presentations in human journals, manual therapy avian models and adolescent models in man. -

1 the Thoracic Wall I
AAA_C01 12/13/05 10:29 Page 8 1 The thoracic wall I Thoracic outlet (inlet) First rib Clavicle Suprasternal notch Manubrium 5 Third rib 1 2 Body of sternum Intercostal 4 space Xiphisternum Scalenus anterior Brachial Cervical Costal cartilage plexus rib Costal margin 3 Subclavian 1 Costochondral joint Floating ribs artery 2 Sternocostal joint Fig.1.3 3 Interchondral joint Bilateral cervical ribs. 4 Xiphisternal joint 5 Manubriosternal joint On the right side the brachial plexus (angle of Louis) is shown arching over the rib and stretching its lowest trunk Fig.1.1 The thoracic cage. The outlet (inlet) of the thorax is outlined Transverse process with facet for rib tubercle Demifacet for head of rib Head Neck Costovertebral T5 joint T6 Facet for Tubercle vertebral body Costotransverse joint Sternocostal joint Shaft 6th Angle rib Costochondral Subcostal groove joint Fig.1.2 Fig.1.4 A typical rib Joints of the thoracic cage 8 The thorax The thoracic wall I AAA_C01 12/13/05 10:29 Page 9 The thoracic cage Costal cartilages The thoracic cage is formed by the sternum and costal cartilages These are bars of hyaline cartilage which connect the upper in front, the vertebral column behind and the ribs and intercostal seven ribs directly to the sternum and the 8th, 9th and 10th ribs spaces laterally. to the cartilage immediately above. It is separated from the abdominal cavity by the diaphragm and communicates superiorly with the root of the neck through Joints of the thoracic cage (Figs 1.1 and 1.4) the thoracic inlet (Fig. -

Biomechanics of Thoracic Discectomy
Neurosurg Focus 11 (3):Article 6, 2001, Click here to return to Table of Contents Biomechanics of thoracic discectomy ANDREW E. WAKEFIELD, M.D., MICHAEL P. STEINMETZ, M.D., AND EDWARD C. BENZEL, M.D. Department of Neurosurgery, Hartford Hospital, Hartford, Connecticut; and The Cleveland Clinic Foundation, Department of Neurosurgery, Cleveland, Ohio The thoracic spine is a structurally unique region that renders it uniquely suceptible to thoracic disc herniation. Surgical management strategies are complicated, in part, by the regional anatomical and biomechanical nuances. Surgical approaches include posterior, posterolateral, and anterior routes. Each isassociated with specific indications and contraindications. The biomechanical principles and safe anatomical trajectories must be considered in the surgical deci- sion-making process. These issues are discussed in the pages that follow. KEY WORDS • biomechanics • thoracic spine • instability • discectomy The thoracic spine has structurally distinct characteris- RELEVANT THORACIC ANATOMY tics that distinguish it from the cervical and lumbar spine. The posterior thoracic VB height is greater than the an- A highly specialized region, it is uniquely adapted to an terior height, which explains, in part, the existence of tho- erect posture and the load-bearing demands required from 5 racic kyphosis. The size of the thoracic VBs increases as the daily activities of upright creatures. The thoracic the thoracic spine descends. The facet joints change their spine has been divided into three regions: 1) the cervical- orientation from the coronal plane in the cervicothoracic to-thoracic transition zone (T1–4) 2), the thoracic-to-lum- region to a more sagittal plane in the thoracolumbar re- bar transition zone (T10–12), and 3) the midthoracic re- 3 16 gion, and this affects spinal motion. -

Costovertebral and Costotransverse Joint Involvement in Rheumatoid Arthritis
Ann Rheum Dis: first published as 10.1136/ard.37.5.473 on 1 October 1978. Downloaded from Annals of the Rheumatic Diseases, 1978, 37, 473475 Costovertebral and costotransverse joint involvement in rheumatoid arthritis MICHAEL J. COHEN, JOAN EZEKIEL, AND ROBERT H. PERSELLIN From the Division ofRheumatology, Department ofMedicine, and the Department ofRadiology, The University of Texas Health Science Center at San Antonio, USA SUMMARY Lesions of the costovertebral (CV) and costotransverse (CT) joints are distinctly unusual in rheumatoid arthritis. The patient presented had dramatic changes in these joints with destruction, ankylosis, and bony overgrowth. This led to a moderate respiratory impairment and a distinctive radiological presentation. The costovertebral (CV) and costotransverse (CT) palpation near the medial borders of the scapulae. joints are diarthrodial joints containing hyaline Chest expansion measured at the fourth intercostal articular cartilage and lined with synovial membrane space was 1.5 cm. She had diffuse tenderness of and can be involved in inflammatory joint disease multiple peripheral joints. There was extensive (Goldthwait, 1940; Dihlman and Frik, 1968; atrophy of the muscles of the hands. Erythema and Zimmer, 1968; Jaffe, 1972). However, lesions of the tenderness were detected over the right achilles copyright. ribs and their articulations with the vertebral column tendon. There were no rheumatoid nodules. are rare. The following is a case with unique involve- The haematocrit was 38 with a white blood cell ment of the CV and CT joints which has not been count of 4900/mm3. The erythrocyte sedimentation previously described. rate was 50 mm/hr (Westergren); a sensitised sheep cell agglutination titre was positive at 1:3584, and an Case report RA slide latex (Hyland) was 4+ positive (Cheng and Persellin, 1971). -
Powerpoint Handout: Lab 1, Thorax
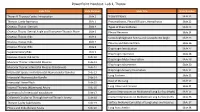
PowerPoint Handout: Lab 1, Thorax Slide Title Slide Number Slide Title Slide Number Thorax & Thoracic Cavity: Introduction Slide 2 Visceral Pleura Slide 21 Thoracic Cavity Apertures Slide 3 Pneumothorax, Pleural Effusion, Hemothorax Slide 22 Osseous Thorax: Sternum Slide 4 Types of Pneumothorax Slide 23 Osseous Thorax: Sternal Angle and Transverse Thoracic Plane Slide 5 Pleural Recesses Slide 24 Osseous Thorax: Ribs Slide 6 Costodiaphragmatic Recess and Costophrenic Angle Slide 25 Osseous Thorax: Ribs Slide 7 Pleurisy and Referred Pain Slide 26 Osseous Thorax: Ribs Slide 8 Diaphragm Introduction Slide 27 Supernumerary Ribs Slide 9 Diaphragm Apertures Slide 28 Osseous Thorax: Rib Joints Slide 10 Diaphragm Motor Innervation Slide 29 Muscular Thorax: Intercostal Muscles Slide 11 Diaphragm Movements Slide 30 Muscular Thorax: Intercostal Muscles (Continued) Slide 12 Diaphragm Sensory Innervation Slide 31 Intercostal Spaces and Intercostal Neurovascular Bundles Slide 13 Lung Surfaces Slide 32 Intercostal Neurovascular Bundle Slide 14 Root of the Lung Slide 33 Intercostal Nerve Block Slide 15 Slide 34 Internal Thoracic (Mammary) Artery Slide 16 Lung Lobes and Fissures Summary of of Intercostal Vasculature Slide 17 Contact Impressions on Mediastinal Lung Surface (Right) Slide 35 Collateral Circulation Through Internal Thoracic Artery Slide 18 Contact Impressions on Mediastinal Lung Surface (Left) Slide 36 Thoracic Cavity Subdivisions Slide 19 Surface Anatomy Correlates of Lung Lobes and Fissures Slide 37 Pleura and Endothoracic Fascia Slide 20 Lung Auscultation Slide 38 Thorax & Thoracic Cavity: Introduction The thorax refers to the region of the body between the neck https://3d4medic.al/enFsQOFf and the abdomen. The thoracic cavity is an irregularly shaped cylinder enclosed by the musculoskeletal walls of the thorax and the diaphragm. -

Alligator Mississippiensis): an XROMM Analysis Robert J
© 2017. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2017) 220, 3181-3190 doi:10.1242/jeb.156166 RESEARCH ARTICLE Rib kinematics during lung ventilation in the American alligator (Alligator mississippiensis): an XROMM analysis Robert J. Brocklehurst1,*, Sabine Moritz2, Jonathan Codd3, William I. Sellers1 and Elizabeth L. Brainerd2 ABSTRACT these, the two most important are costal aspiration and the hepatic The current hypothesis regarding the mechanics of breathing in piston (Movie 1) (Claessens, 2009b). crocodylians is that the double-headed ribs, with both a capitulum and The mechanics of the hepatic piston are relatively straightforward tuberculum, rotate about a constrained axis passing through the two and have been extensively studied (Farmer and Carrier, 2000; articulations; moreover, this axis shifts in the caudal thoracic ribs, as Uriona and Farmer, 2006; Munns et al., 2012), but costal aspiration the vertebral parapophysis moves from the centrum to the transverse is more complex. Ventilation is powered by the hypaxial muscles, process. Additionally, the ventral ribcage in crocodylians is thought to with the transverse abdominal responsible for exhalation, and the possess additional degrees of freedom through mobile intermediate intercostal muscles powering inhalation and exhalation (Gans and ribs. In this study, X-ray reconstruction of moving morphology Clark, 1976; Carrier, 1989; Brainerd and Owerkowicz, 2006). (XROMM) was used to quantify rib rotation during breathing in However, muscles can only do positive work and hence contribute American alligators. Whilst costovertebral joint anatomy predicted to ventilation when actively shortening, but in order to power overall patterns of motion across the ribcage (decreased bucket inhalation this muscular contraction must be converted into handle motion and increased calliper motion), there were significant expansion of the thorax (Brainerd and Owerkowicz, 2006; deviations: anatomical axes overestimated pump handle motion and, Brainerd, 2015). -

Anatomy of the Thoracic Region
Applied Anatomy Anatomy and Kinesiology 12 vertebrae of the Thoracic Spine 12 pairs of ribs Costovertebral joints Cosotransverse joints Costosternal joints Review of the basics before we get Interchondral/interc down to assessment and diagnosis ostal joints Facet joints Intervetebral discs Thoracic Vertebrae Thoracic Vertebrae Similar in basic make-up to the lower cervical and lumbar vertebrae Possess longer spinous processes which over lap considerably Design of the vertebrae lead to a natural mild kyphosis Contains less motion than either the lumbar or cervical regions 1 Facet Joints of the Thoracic Spine The Ribs Resting position: Midway between flexion and extension Close packed position: Extension Capsular pattern: Side flexion and rotation equally limited, then extension The Ribs Intercostal Muscles 12 pairs of ribs Muscles run between ribs in pairs Lowest pairs (11th and 12th) do not have an Internal intercostals extend from the front of anterior attachment – Floating Ribs the ribs, and go posteriorly past the rib Middle pairs (8th -10th) attach to sternum via angle. a combined cartilaginous attachment – False External intercostals (on the outside of the Ribs ribcase) wrap around from the back of the Uppermost pairs (1st-7th) have bony rib almost to the end of the rib anteriorly. attachments both anteriorly and posteriorly Diagonal direction improves elevation of the ribs during respiration. Costovertebral Joints Costotransverse Joint Synovial joints Synovial joints The tubercle of the rib articulates with the Head of the rib articulates with the vertebral transverse process of the thoracic vertebra body below, the intervertebral disc and the The 11th and 12th ribs do not articulate in vertebral body above. -

Mechanical Role of the Spine, Ribcage and Interabdominal Pressure in The
DEVELOPMENT OF A NON-FUSION SCOLIOSIS CORRECTION DEVICE NUMERICAL MODELLING OF SCOLIOSIS CORRECTION This project, “A non-fusion scoliosis correction device”, was supported by a grant from the Dutch Technology Foundation (STW), applied science division of NWO and the Technology Program of the ministry of economic affairs (project number 07618). The printing of this thesis was financially supported by: Stichting Technologische Wetenschappen (STW) Samenstelling promotiecommissie: Voorzittert en secretaris: Prof. dr. F. Eising Universiteit Twente Promotoren: Prof. dr. ir. G.J. Verkerke Universiteit Twente Prof. dr. A.G. Veldhuizen Universitair Medisch Centrum Groningen Assistent promotor: Dr. ir. J.J. Homminga Universiteit Twente Leden: Prof. dr. ir. N.J.J. Verdonschot Universiteit Twente Prof. dr. ir. A. De Boer Universiteit Twente Prof. dr. K. Ito Technische Universiteit Eindhoven Prof. dr. J.H. van Dieën Vrije Universiteit Amsterdam Prof. dr. ir. N.M. Maurits Universitair Medisch Centrum Groningen Paranimfen: Tjitske Boonstra Evelien Platvoet Printed by: Ipskamp Drukkers BV, Enschede ISBN: 978-90-365-3229-7 Copyright © 2011 by G.J.M. Meijer, Enschede, The Netherlands. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording or any information storage or retrieval system, without permission in writing from the author. DEVELOPMENT OF A NON-FUSION SCOLIOSIS CORRECTION DEVICE NUMERICAL MODELLING OF SCOLIOSIS CORRECTION PROEFSCHRIFT ter verkrijging van de graad van doctor aan de Universiteit Twente, op gezag van de rector magnificus, prof. dr. H. Brinksma, volgens besluit van het College voor Promoties in het openbaar te verdedigen op vrijdag 14 oktober 2011 om 12.45 uur door Gerarda Johanna Maria Meijer geboren op 6 december 1978 te Oldenzaal Dit proefschrift is goedgekeurd door: Prof. -

16 Thoracic Spine
THORACIC SPINE Non-musculoskeletal causes of thoracic back pain are: • Heart - myocardial infarction, angina, pericarditis • Great vessels - dissecting aneurysm, pulmonary embolism, pulmonary infarction, pneumothorax, pneumonia, pleurisy • Esophagus - esophageal rupture, esophageal spasm, esophagitis • Subdiaphragmatic disorders - gall bladder, stomach, duodenum, pancreas, subphrenic collection • Infections - herpes zoster, Bornholm's disease, infective endocarditis Those that should be carefully considered are myocardial infarction and ) dissecting aneurysm. Investigations for acute infections should be considered for those patients presenting with poor general health and fever. Symptoms and signs that should alert the clinician to malignant disease are: • Back pain in an older person • Unrelenting back pain, unrelieved by rest • Night pain • Rapidly increasing back pain • Constitutional symptoms such as weight loss, fever, malaise • History of cancer • Two commonly misdiagnosed problems are penetrating duodenal ulcer presenting with lower thoracic pain, and esophageal spasm, which can cause thoracic back pain. Pain from the thoracic spine originates mainly from the zygapophyseal joints and rib articulations. Any one thoracic vertebra has ten separate articulations, so the potential for dysfunction is understandable. Pain of musculoskeletal origin in the upper costochondral region can arise from four sources: 1. it may be referred 2. be due to polyarthritis 3. post traumatic Section 16 Page 1 4. Tietze's syndrome The most common cause