General Disease Finder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Increased Nuchal Translucency Precision Panel
Increased Nuchal Translucency Precision Panel Overview Increased Nuchal Translucency (NT) is defined as an abnormal accumulation of fluid in the nuchal area, which is visualized as a thickened sonolucent area. It is a standardized measure obtained between 11 and 14 weeks of gestation to calculate the risk of a fetus being affected by a chromosomal aneuploidy. NT>3.5mm has been found to be associated with fetal chromosomal abnormalities and single-gene disorders as well as cardiac defects and other structural abnormalities in euploid and aneuploid fetuses. Proportionally as NT increases, even with a normal karyotype, there is a higher risk of adverse pregnancy outcomes such as miscarriage, intrauterine death, congenital heart defects and numerous other structural and genetic syndromes. There is not one single cause of increased NT, it is based on a complex and multifactorial process, linked to one or more embryonic processes. It has been shown that a persistently increased NT with a normal karyotype and aCGH has a 4-10% probability of being associated to Noonan Syndrome and/or other RASopathies using Whole Exome Sequencing (WES). However, the general tendency following detection of isolated enlarged NT in an euploid fetus is that most babies with normal detailed ultrasound examination and echocardiography will have uneventful outcomes. The Igenomix Increased Nuchal Translucency Precision Panel can be used to make a directed and accurate prenatal differential diagnosis of increased nuchal translucency in patients with or without a normal karyotype ultimately leading to a better management and prognosis of the associated comorbidities. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. -

(12) Patent Application Publication (10) Pub. No.: US 2007/0254315 A1 Cox Et Al
US 20070254315A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2007/0254315 A1 Cox et al. (43) Pub. Date: Nov. 1, 2007 (54) SCREENING FOR NEUROTOXIC AMINO (60) Provisional application No. 60/494.686, filed on Aug. ACID ASSOCATED WITH NEUROLOGICAL 12, 2003. DSORDERS Publication Classification (75) Inventors: Paul A. Cox, Provo, UT (US); Sandra A. Banack, Fullerton, CA (US); Susan (51) Int. Cl. J. Murch, Cambridge (CA) GOIN 33/566 (2006.01) GOIN 33/567 (2006.01) Correspondence Address: (52) U.S. Cl. ............................................................ 435/721 PILLSBURY WINTHROP SHAW PITTMAN LLP (57) ABSTRACT ATTENTION: DOCKETING DEPARTMENT Methods for screening for neurological disorders are dis P.O BOX 105OO closed. Specifically, methods are disclosed for screening for McLean, VA 22102 (US) neurological disorders in a Subject by analyzing a tissue sample obtained from the subject for the presence of (73) Assignee: THE INSTITUTE FOR ETHNO elevated levels of neurotoxic amino acids or neurotoxic MEDICINE, Provo, UT derivatives thereof associated with neurological disorders. In particular, methods are disclosed for diagnosing a neu (21) Appl. No.: 11/760,668 rological disorder in a subject, or predicting the likelihood of developing a neurological disorder in a Subject, by deter (22) Filed: Jun. 8, 2007 mining the levels of B-N-methylamino-L-alanine (BMAA) Related U.S. Application Data in a tissue sample obtained from the subject. Methods for screening for environmental factors associated with neuro (63) Continuation of application No. 10/731,411, filed on logical disorders are disclosed. Methods for inhibiting, treat Dec. 8, 2003, now Pat. No. 7,256,002. -

Peripheral Neuropathy in Complex Inherited Diseases: an Approach To
PERIPHERAL NEUROPATHY IN COMPLEX INHERITED DISEASES: AN APPROACH TO DIAGNOSIS Rossor AM1*, Carr AS1*, Devine H1, Chandrashekar H2, Pelayo-Negro AL1, Pareyson D3, Shy ME4, Scherer SS5, Reilly MM1. 1. MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology and National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 2. Lysholm Department of Neuroradiology, National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 3. Unit of Neurological Rare Diseases of Adulthood, Carlo Besta Neurological Institute IRCCS Foundation, Milan, Italy. 4. Department of Neurology, University of Iowa, 200 Hawkins Drive, Iowa City, IA 52242, USA 5. Department of Neurology, University of Pennsylvania, Philadelphia, PA 19014, USA. * These authors contributed equally to this work Corresponding author: Mary M Reilly Address: MRC Centre for Neuromuscular Diseases, 8-11 Queen Square, London, WC1N 3BG, UK. Email: [email protected] Telephone: 0044 (0) 203 456 7890 Word count: 4825 ABSTRACT Peripheral neuropathy is a common finding in patients with complex inherited neurological diseases and may be subclinical or a major component of the phenotype. This review aims to provide a clinical approach to the diagnosis of this complex group of patients by addressing key questions including the predominant neurological syndrome associated with the neuropathy e.g. spasticity, the type of neuropathy, and the other neurological and non- neurological features of the syndrome. Priority is given to the diagnosis of treatable conditions. Using this approach, we associated neuropathy with one of three major syndromic categories - 1) ataxia, 2) spasticity, and 3) global neurodevelopmental impairment. Syndromes that do not fall easily into one of these three categories can be grouped according to the predominant system involved in addition to the neuropathy e.g. -

Case Vignettes
“Doc, DO I Have Neuropathy?” Case Vignettes Susan, 50 Gwenn, 32 John, 52 Sally, 42 DM – 12 yrs Hypothyroidism No PMH No PMH B/N/T – 2 yrs N/T at night B/N/T – 6 days B/N/T – few months 3 months Stanley Jones P. Iyadurai, MSc, PhD, MD Hands, Hands, Arms Hands, Feet Assistant Professor of Neurology Feet Right hand Feet, Legs Burning Pain Neuromuscular Division, Department of Neurology Arms, Difficulty Pain Pain The Ohio State University Wexner Medical Center Legs Opening jars Breathing Redness Imbalance Normal gait Imbalance Normal Strength “Neuropathy” - Definition Neuropathy - General Theme • Symmetric • “Neuron” and “Pathos” (Greek) • Insidious • More prominent distally and starts in • Disease of the Peripheral Nerve legs • Involves both motor and sensory • Dysfunction of the nerves outside of components the central nervous system • May cause pain • May cause loss of balance • Progressive, but not debilitating 1 Not all that tingles is Classification - Functional neuropathy ‘numbness and tingling’ • Motor – affects the motor nerves Weakness • not all numbness and tingling is • Sensory peripheral nerve ‒ Pain • RLS ‒ Small Fiber ‒ Large Fiber • edema ‒ Large and Small Fiber • deconditioning ‒ Neuronopathy (ganglionopathy) • central nervous system • Autonomic • Sweating Changes, Blood Pressure Changes • nerve root [‘sciatica’] Classification – Time-course Classification – Time-course • Acute Immune-mediated • Congenital/Hereditary • Infantile Weakness • Childhood-onset • Acquired • Relapsing ‒ Reversible? • Hereditary ‒ Demyelinating? -

POEMS Syndrome: an Atypical Presentation with Chronic Diarrhoea and Asthenia
European Journal of Case Reports in Internal Medicine POEMS Syndrome: an Atypical Presentation with Chronic Diarrhoea and Asthenia Joana Alves Vaz1, Lilia Frada2, Maria Manuela Soares1, Alberto Mello e Silva1 1 Department of Internal Medicine, Egas Moniz Hospital, Lisbon, Portugal 2 Department of Gynecology and Obstetrics, Espirito Santo Hospital, Evora, Portugal Doi: 10.12890/2019_001241 - European Journal of Case Reports in Internal Medicine - © EFIM 2019 Received: 28/07/2019 Accepted: 13/11/2019 Published: 16/12/2019 How to cite this article: Alves Vaz J, Frada L, Soares MM, Mello e Silva A. POEMS syndrome: an atypical presentation with chronic diarrhoea and astenia. EJCRIM 2019;7: doi:10.12890/2019_001241. Conflicts of Interests: The Authors declare that there are no competing interest This article is licensed under a Commons Attribution Non-Commercial 4.0 License ABSTRACT POEMS syndrome is a rare paraneoplastic condition associated with polyneuropathy, organomegaly, monoclonal gammopathy, endocrine and skin changes. We report a case of a man with Castleman disease and monoclonal gammopathy, with a history of chronic diarrhoea and asthenia. Gastrointestinal involvement in POEMS syndrome is not frequently referred to in the literature and its physiopathology is not fully understood. Diagnostic criteria were met during hospitalization but considering the patient’s overall health condition, therapeutic options were limited. Current treatment for POEMS syndrome depends on the management of the underlying plasma cell disorder. This report outlines the importance of a thorough review of systems and a physical examination to allow an attempted diagnosis and appropriate treatment. LEARNING POINTS • POEMS syndrome should be suspected in the presence of peripheral polyneuropathy associated with monoclonal gammopathy; diagnostic workup is challenging and delay in treatment is very common. -

Ataxia with Loss of Purkinje Cells in a Mouse Model for Refsum Disease
Ataxia with loss of Purkinje cells in a mouse model for Refsum disease Sacha Ferdinandussea,1,2, Anna W. M. Zomerb,1, Jasper C. Komena, Christina E. van den Brinkb, Melissa Thanosa, Frank P. T. Hamersc, Ronald J. A. Wandersa,d, Paul T. van der Saagb, Bwee Tien Poll-Thed, and Pedro Britesa Academic Medical Center, Departments of aClinical Chemistry (Laboratory of Genetic Metabolic Diseases) and dPediatrics, Emma’s Children Hospital, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; bHubrecht Institute, Royal Netherlands Academy of Arts and Sciences 3584 CT Utrecht, The Netherlands; and cRehabilitation Hospital ‘‘De Hoogstraat’’ Rudolf Magnus Institute of Neuroscience, 3584 CG Utrecht, The Netherlands Edited by P. Borst, The Netherlands Cancer Institute, Amsterdam, The Netherlands, and approved October 3, 2008 (received for review June 23, 2008) Refsum disease is caused by a deficiency of phytanoyl-CoA hy- Clinically, Refsum disease is characterized by cerebellar droxylase (PHYH), the first enzyme of the peroxisomal ␣-oxidation ataxia, polyneuropathy, and progressive retinitis pigmentosa, system, resulting in the accumulation of the branched-chain fatty culminating in blindness, (1, 3). The age of onset of the symptoms acid phytanic acid. The main clinical symptoms are polyneuropathy, can vary from early childhood to the third or fourth decade of cerebellar ataxia, and retinitis pigmentosa. To study the patho- life. No treatment is available for patients with Refsum disease, genesis of Refsum disease, we generated and characterized a Phyh but they benefit from a low phytanic acid diet. Phytanic acid is knockout mouse. We studied the pathological effects of phytanic derived from dietary sources only, specifically from the chloro- acid accumulation in Phyh؊/؊ mice fed a diet supplemented with phyll component phytol. -
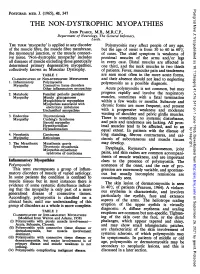
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

ICD9 & ICD10 Neuromuscular Codes
ICD-9-CM and ICD-10-CM NEUROMUSCULAR DIAGNOSIS CODES ICD-9-CM ICD-10-CM Focal Neuropathy Mononeuropathy G56.00 Carpal tunnel syndrome, unspecified Carpal tunnel syndrome 354.00 G56.00 upper limb Other lesions of median nerve, Other median nerve lesion 354.10 G56.10 unspecified upper limb Lesion of ulnar nerve, unspecified Lesion of ulnar nerve 354.20 G56.20 upper limb Lesion of radial nerve, unspecified Lesion of radial nerve 354.30 G56.30 upper limb Lesion of sciatic nerve, unspecified Sciatic nerve lesion (Piriformis syndrome) 355.00 G57.00 lower limb Meralgia paresthetica, unspecified Meralgia paresthetica 355.10 G57.10 lower limb Lesion of lateral popiteal nerve, Peroneal nerve (lesion of lateral popiteal nerve) 355.30 G57.30 unspecified lower limb Tarsal tunnel syndrome, unspecified Tarsal tunnel syndrome 355.50 G57.50 lower limb Plexus Brachial plexus lesion 353.00 Brachial plexus disorders G54.0 Brachial neuralgia (or radiculitis NOS) 723.40 Radiculopathy, cervical region M54.12 Radiculopathy, cervicothoracic region M54.13 Thoracic outlet syndrome (Thoracic root Thoracic root disorders, not elsewhere 353.00 G54.3 lesions, not elsewhere classified) classified Lumbosacral plexus lesion 353.10 Lumbosacral plexus disorders G54.1 Neuralgic amyotrophy 353.50 Neuralgic amyotrophy G54.5 Root Cervical radiculopathy (Intervertebral disc Cervical disc disorder with myelopathy, 722.71 M50.00 disorder with myelopathy, cervical region) unspecified cervical region Lumbosacral root lesions (Degeneration of Other intervertebral disc degeneration, -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Disease Mutations in the Ryanodine Receptor N-Terminal Region Couple to a Mobile Intersubunit Interface
ARTICLE Received 1 Oct 2012 | Accepted 15 Jan 2013 | Published 19 Feb 2013 DOI: 10.1038/ncomms2501 OPEN Disease mutations in the ryanodine receptor N-terminal region couple to a mobile intersubunit interface Lynn Kimlicka1, Kelvin Lau1, Ching-Chieh Tung1 & Filip Van Petegem1 Ryanodine receptors are large channels that release Ca2 þ from the endoplasmic and sar- coplasmic reticulum. Hundreds of RyR mutations can cause cardiac and skeletal muscle disorders, yet detailed mechanisms explaining their effects have been lacking. Here we compare pseudo-atomic models and propose that channel opening coincides with widen- ing of a cytoplasmic vestibule formed by the N-terminal region, thus altering an interface targeted by 20 disease mutations. We solve crystal structures of several disease mutants that affect intrasubunit domain–domain interfaces. Mutations affecting intrasubunit ionic pairs alter relative domain orientations, and thus couple to surrounding interfaces. Buried disease mutations cause structural changes that also connect to the intersubunit contact area. These results suggest that the intersubunit contact region between N-terminal domains is a prime target for disease mutations, direct or indirect, and we present a model whereby ryanodine receptors and inositol-1,4,5-trisphosphate receptors are activated by altering domain arrangements in the N-terminal region. 1 Department of Biochemistry and Molecular Biology, Life Sciences Institute, University of British Columbia, Vancouver, British Columbia, Canada V6T 1Z3. Correspondence and requests for materials should be addressed to F.V.P. (email: fi[email protected]). NATURE COMMUNICATIONS | 4:1506 | DOI: 10.1038/ncomms2501 | www.nature.com/naturecommunications 1 & 2013 Macmillan Publishers Limited. All rights reserved. -

Come to Your Senses: Atypical Polyneuropathy
Come To Your Senses: Atypical Polyneuropathy Damian Campbell, DO; Joshua Lovell, DO; Krishna Pokala, MD; Yessar Hussain, MD The University of Texas at Austin, Department of Neurology, Dell Medical School Clinical History Workup Diagnosis and Discussion Pathophysiology 35 year old female was referred to the neurology clinic for evaluation of an Electrodiagnostics Our patients clinical history and genetic testing results were consistent and There is a great deal of variability in the presentation of symptoms; as there is abnormal gait. She reported slow but progressive changes in her gait over the she was diagnosed with PHARC: Polyneuropathy, Hearing Loss, Ataxia, variability amongst the gene mutations leading to inactive ABHD12. Despite the course of the last ten years. Her changes ranged from a sense of feeling off- Nerve Conductions Retinitis Pigmentosa, Cataracts. variability that exists within gene mutations, it is posited that all of the balanced to shooting pain down each leg She felt that her pain originated in her Distal Latency Peak Amplitude Conduction Velocity homozygous mutations result in complete loss-of-function of the ABHD12 low back and radiated posteriorly down each leg without any accompanying Latency (m/sec) PHARC was first described by Fiskerstrand et al in 2008.(1) At that time they enzyme. Reduction in ABHD12 results in increased levels of endocannabinoid Right Median CMAP 4.3 7.8 numbness, weakness, or bowel and bladder involvement. Of significance is her were attempting to genetically characterize a neurological disorder that arachidonoyl glycerol 2-AG, which has important functions in synaptic plasticity 11.6 5.8 26 resembled Refsum disease in a Norwegian family. -

Orphanet Report Series Rare Diseases Collection
Orphanet Report Series Rare Diseases collection January 2013 Disease Registries in Europe www.orpha.net 20102206 Table of contents Methodology 3 List of rare diseases that are covered by the listed registries 4 Summary 13 1- Distribution of registries by country 13 2- Distribution of registries by coverage 14 3- Distribution of registries by affiliation 14 Distribution of registries by country 15 European registries 38 International registries 41 Orphanet Report Series - Disease Registries in Europe - January 2013 2 http://www.orpha.net/orphacom/cahiers/docs/GB/Registries.pdf Methodology Patient registries and databases constitute key instruments to develop clinical research in the field of rare diseases (RD), to improve patient care and healthcare planning. They are the only way to pool data in order to achieve a sufficient sample size for epidemiological and/or clinical research. They are vital to assess the feasibility of clinical trials, to facilitate the planning of appropriate clinical trials and to support the enrolment of patients. Registries of patients treated with orphan drugs are particularly relevant as they allow the gathering of evidence on the effectiveness of the treatment and on its possible side effects, keeping in mind that marketing authorisation is usually granted at a time when evidence is still limited although already somewhat convincing. This report gather the information collected by Orphanet so far, regarding systematic collections of data for a specific disease or a group of diseases. Cancer registries are listed only if they belong to the network RARECARE or focus on a rare form of cancer. The report includes data about EU countries and surrounding countries participating to the Orphanet consortium.