Neurological Diseases Caused by Ion-Channel Mutations Frank Weinreich and Thomas J Jentsch*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SRC Antibody - N-Terminal Region (ARP32476 P050) Data Sheet
SRC antibody - N-terminal region (ARP32476_P050) Data Sheet Product Number ARP32476_P050 Product Name SRC antibody - N-terminal region (ARP32476_P050) Size 50ug Gene Symbol SRC Alias Symbols ASV; SRC1; c-SRC; p60-Src Nucleotide Accession# NM_005417 Protein Size (# AA) 536 amino acids Molecular Weight 60kDa Product Format Lyophilized powder NCBI Gene Id 6714 Host Rabbit Clonality Polyclonal Official Gene Full Name V-src sarcoma (Schmidt-Ruppin A-2) viral oncogene homolog (avian) Gene Family SH2D This is a rabbit polyclonal antibody against SRC. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Peptide Sequence Synthetic peptide located within the following region: QTPSKPASADGHRGPSAAFAPAAAEPKLFGGFNSSDTVTSPQRAGPLAGG This gene is highly similar to the v-src gene of Rous sarcoma virus. This proto-oncogene may play a role in the Description of Target regulation of embryonic development and cell growth. SRC protein is a tyrosine-protein kinase whose activity can be inhibited by phosphorylation by c-SRC kinase. Mutations in this gene could be involved in the -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Transcriptomic Analysis of Native Versus Cultured Human and Mouse Dorsal Root Ganglia Focused on Pharmacological Targets Short
bioRxiv preprint doi: https://doi.org/10.1101/766865; this version posted September 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Transcriptomic analysis of native versus cultured human and mouse dorsal root ganglia focused on pharmacological targets Short title: Comparative transcriptomics of acutely dissected versus cultured DRGs Andi Wangzhou1, Lisa A. McIlvried2, Candler Paige1, Paulino Barragan-Iglesias1, Carolyn A. Guzman1, Gregory Dussor1, Pradipta R. Ray1,#, Robert W. Gereau IV2, # and Theodore J. Price1, # 1The University of Texas at Dallas, School of Behavioral and Brain Sciences and Center for Advanced Pain Studies, 800 W Campbell Rd. Richardson, TX, 75080, USA 2Washington University Pain Center and Department of Anesthesiology, Washington University School of Medicine # corresponding authors [email protected], [email protected] and [email protected] Funding: NIH grants T32DA007261 (LM); NS065926 and NS102161 (TJP); NS106953 and NS042595 (RWG). The authors declare no conflicts of interest Author Contributions Conceived of the Project: PRR, RWG IV and TJP Performed Experiments: AW, LAM, CP, PB-I Supervised Experiments: GD, RWG IV, TJP Analyzed Data: AW, LAM, CP, CAG, PRR Supervised Bioinformatics Analysis: PRR Drew Figures: AW, PRR Wrote and Edited Manuscript: AW, LAM, CP, GD, PRR, RWG IV, TJP All authors approved the final version of the manuscript. 1 bioRxiv preprint doi: https://doi.org/10.1101/766865; this version posted September 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Spinocerebellar Ataxia Type 19/22 Mutations Alter Heterocomplex Kv4.3 Channel Function and Gating in a Dominant Manner
Cell. Mol. Life Sci. (2015) 72:3387–3399 DOI 10.1007/s00018-015-1894-2 Cellular and Molecular Life Sciences RESEARCH ARTICLE Spinocerebellar ataxia type 19/22 mutations alter heterocomplex Kv4.3 channel function and gating in a dominant manner 1 4 1 2 1 Anna Duarri • Meng-Chin A. Lin • Michiel R. Fokkens • Michel Meijer • Cleo J. L. M. Smeets • 1 2 1 3 4 Esther A. R. Nibbeling • Erik Boddeke • Richard J. Sinke • Harm H. Kampinga • Diane M. Papazian • Dineke S. Verbeek1 Received: 31 July 2014 / Revised: 5 March 2015 / Accepted: 24 March 2015 / Published online: 9 April 2015 Ó The Author(s) 2015. This article is published with open access at Springerlink.com Abstract The dominantly inherited cerebellar ataxias are SCA19/22 mutations may lead to Purkinje cell loss, neu- a heterogeneous group of neurodegenerative disorders rodegeneration and ataxia. caused by Purkinje cell loss in the cerebellum. Recently, we identified loss-of-function mutations in the KCND3 Keywords KCND3 Á Kv4.3 Á Spinocerebellar ataxia Á gene as the cause of spinocerebellar ataxia type 19/22 Purkinje cells Á Voltage-gated potassium channel (SCA19/22), revealing a previously unknown role for the voltage-gated potassium channel, Kv4.3, in Purkinje cell survival. However, how mutant Kv4.3 affects wild-type Introduction Kv4.3 channel functioning remains unknown. We provide evidence that SCA19/22-mutant Kv4.3 exerts a dominant Spinocerebellar ataxia type 19/22 (SCA19/22) is a negative effect on the trafficking and surface expression of dominantly inherited neurodegenerative, clinically hetero- wild-type Kv4.3 in the absence of its regulatory subunit, geneous disorder caused by mutations in KCND3, which KChIP2. -
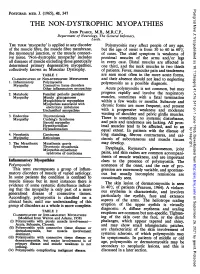
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

New Developments in Charcot–Marie–Tooth Neuropathy and Related Diseases
CE: Alpana; WCO 300505; Total nos of Pages: 10; WCO 300505 REVIEW CURRENT OPINION New developments in Charcot–Marie–Tooth neuropathy and related diseases Davide Pareyson, Paola Saveri, and Chiara Pisciotta Purpose of review Charcot–Marie–Tooth disease (CMT) and related neuropathies represent a heterogeneous group of hereditary disorders. The present review will discuss the most recent advances in the field. Recent findings Knowledge of CMT epidemiology and frequency of the main associated genes is increasing, with an overall prevalence estimated at 10–28/100 000. In the last years, the huge number of newly uncovered genes, thanks to next-generation sequencing techniques, is challenging the current classification of CMT. During the last 18 months other genes have been associated with CMT, such as PMP2, MORC2, NEFH, MME, and DGAT2. For the most common forms of CMT, numerous promising compounds are under study in cellular and animal models, mainly targeting either the protein degradation pathway or the protein overexpression. Consequently, efforts are devoted to develop responsive outcome measures and biomarkers for this overall slowly progressive disorder, with quantitative muscle MRI resulting the most sensitive-to-change measure. Summary This is a rapidly evolving field where better understanding of pathophysiology is paving the way to develop potentially effective treatments, part of which will soon be tested in patients. Intense research is currently devoted to prepare clinical trials and develop responsive outcome measures. Keywords -

Ion Channels 3 1
r r r Cell Signalling Biology Michael J. Berridge Module 3 Ion Channels 3 1 Module 3 Ion Channels Synopsis Ion channels have two main signalling functions: either they can generate second messengers or they can function as effectors by responding to such messengers. Their role in signal generation is mainly centred on the Ca2 + signalling pathway, which has a large number of Ca2+ entry channels and internal Ca2+ release channels, both of which contribute to the generation of Ca2 + signals. Ion channels are also important effectors in that they mediate the action of different intracellular signalling pathways. There are a large number of K+ channels and many of these function in different + aspects of cell signalling. The voltage-dependent K (KV) channels regulate membrane potential and + excitability. The inward rectifier K (Kir) channel family has a number of important groups of channels + + such as the G protein-gated inward rectifier K (GIRK) channels and the ATP-sensitive K (KATP) + + channels. The two-pore domain K (K2P) channels are responsible for the large background K current. Some of the actions of Ca2 + are carried out by Ca2+-sensitive K+ channels and Ca2+-sensitive Cl − channels. The latter are members of a large group of chloride channels and transporters with multiple functions. There is a large family of ATP-binding cassette (ABC) transporters some of which have a signalling role in that they extrude signalling components from the cell. One of the ABC transporters is the cystic − − fibrosis transmembrane conductance regulator (CFTR) that conducts anions (Cl and HCO3 )and contributes to the osmotic gradient for the parallel flow of water in various transporting epithelia. -

Disease Mutations in the Ryanodine Receptor N-Terminal Region Couple to a Mobile Intersubunit Interface
ARTICLE Received 1 Oct 2012 | Accepted 15 Jan 2013 | Published 19 Feb 2013 DOI: 10.1038/ncomms2501 OPEN Disease mutations in the ryanodine receptor N-terminal region couple to a mobile intersubunit interface Lynn Kimlicka1, Kelvin Lau1, Ching-Chieh Tung1 & Filip Van Petegem1 Ryanodine receptors are large channels that release Ca2 þ from the endoplasmic and sar- coplasmic reticulum. Hundreds of RyR mutations can cause cardiac and skeletal muscle disorders, yet detailed mechanisms explaining their effects have been lacking. Here we compare pseudo-atomic models and propose that channel opening coincides with widen- ing of a cytoplasmic vestibule formed by the N-terminal region, thus altering an interface targeted by 20 disease mutations. We solve crystal structures of several disease mutants that affect intrasubunit domain–domain interfaces. Mutations affecting intrasubunit ionic pairs alter relative domain orientations, and thus couple to surrounding interfaces. Buried disease mutations cause structural changes that also connect to the intersubunit contact area. These results suggest that the intersubunit contact region between N-terminal domains is a prime target for disease mutations, direct or indirect, and we present a model whereby ryanodine receptors and inositol-1,4,5-trisphosphate receptors are activated by altering domain arrangements in the N-terminal region. 1 Department of Biochemistry and Molecular Biology, Life Sciences Institute, University of British Columbia, Vancouver, British Columbia, Canada V6T 1Z3. Correspondence and requests for materials should be addressed to F.V.P. (email: fi[email protected]). NATURE COMMUNICATIONS | 4:1506 | DOI: 10.1038/ncomms2501 | www.nature.com/naturecommunications 1 & 2013 Macmillan Publishers Limited. All rights reserved. -

X-Linked Diseases: Susceptible Females
REVIEW ARTICLE X-linked diseases: susceptible females Barbara R. Migeon, MD 1 The role of X-inactivation is often ignored as a prime cause of sex data include reasons why women are often protected from the differences in disease. Yet, the way males and females express their deleterious variants carried on their X chromosome, and the factors X-linked genes has a major role in the dissimilar phenotypes that that render women susceptible in some instances. underlie many rare and common disorders, such as intellectual deficiency, epilepsy, congenital abnormalities, and diseases of the Genetics in Medicine (2020) 22:1156–1174; https://doi.org/10.1038/s41436- heart, blood, skin, muscle, and bones. Summarized here are many 020-0779-4 examples of the different presentations in males and females. Other INTRODUCTION SEX DIFFERENCES ARE DUE TO X-INACTIVATION Sex differences in human disease are usually attributed to The sex differences in the effect of X-linked pathologic variants sex specific life experiences, and sex hormones that is due to our method of X chromosome dosage compensation, influence the function of susceptible genes throughout the called X-inactivation;9 humans and most placental mammals – genome.1 5 Such factors do account for some dissimilarities. compensate for the sex difference in number of X chromosomes However, a major cause of sex-determined expression of (that is, XX females versus XY males) by transcribing only one disease has to do with differences in how males and females of the two female X chromosomes. X-inactivation silences all X transcribe their gene-rich human X chromosomes, which is chromosomes but one; therefore, both males and females have a often underappreciated as a cause of sex differences in single active X.10,11 disease.6 Males are the usual ones affected by X-linked For 46 XY males, that X is the only one they have; it always pathogenic variants.6 Females are biologically superior; a comes from their mother, as fathers contribute their Y female usually has no disease, or much less severe disease chromosome. -

SUPPLEMENTARY MATERIAL Effect of Next
SUPPLEMENTARY MATERIAL Effect of Next-Generation Exome Sequencing Depth for Discovery of Diagnostic Variants KKyung Kim1,2,3†, Moon-Woo Seong4†, Won-Hyong Chung3, Sung Sup Park4, Sangseob Leem1, Won Park5,6, Jihyun Kim1,2, KiYoung Lee1,2*‡, Rae Woong Park1,2* and Namshin Kim5,6** 1Department of Biomedical Informatics, Ajou University School of Medicine, Suwon 443-749, Korea 2Department of Biomedical Science, Graduate School, Ajou University, Suwon 443-749, Korea, 3Korean Bioinformation Center, Korea Research Institute of Bioscience and Biotechnology, Daejeon 305-806, Korea, 4Department of Laboratory Medicine, Seoul National University Hospital College of Medicine, Seoul 110-799, Korea, 5Department of Functional Genomics, Korea University of Science and Technology, Daejeon 305-806, Korea, 6Epigenomics Research Center, Genome Institute, Korea Research Institute of Bioscience and Biotechnology, Daejeon 305-806, Korea http//www. genominfo.org/src/sm/gni-13-31-s001.pdf Supplementary Table 1. List of diagnostic genes Gene Symbol Description Associated diseases ABCB11 ATP-binding cassette, sub-family B (MDR/TAP), member 11 Intrahepatic cholestasis ABCD1 ATP-binding cassette, sub-family D (ALD), member 1 Adrenoleukodystrophy ACVR1 Activin A receptor, type I Fibrodysplasia ossificans progressiva AGL Amylo-alpha-1, 6-glucosidase, 4-alpha-glucanotransferase Glycogen storage disease ALB Albumin Analbuminaemia APC Adenomatous polyposis coli Adenomatous polyposis coli APOE Apolipoprotein E Apolipoprotein E deficiency AR Androgen receptor Androgen insensitivity -

The CNS Phenotype of X-Linked Charcot-Marie-Tooth Disease More Than a Peripheral Problem
Views & Reviews CME The CNS phenotype of X-linked Charcot-Marie-Tooth disease More than a peripheral problem Robert A. Taylor, MD; Erin M. Simon, MD; Harold G. Marks, MD; and Steven S. Scherer, MD, PhD X-linked Charcot-Marie-Tooth disease (CMTX) is the lasting 4 hours. The following day, he developed the second most common form of inherited demyelinat- same symptoms, and mild right leg weakness, last- ing neuropathy, next to CMT type 1A, which is ing 10 hours. On day 3, he developed a complete caused by duplication of the PMP22 gene.1 CMTX is motor aphasia, right arm weakness, dysphagia, and caused by mutations in GJB1, the gene encoding loss of gag reflex, lasting 4 hours. MRI (on day 3) connexin32 (Cx32), which belongs to a highly con- showed abnormally increased T2 signal and reduced served family of proteins that form gap junctions in diffusion in the posterior portion of the centrum vertebrates. Myelinating Schwann cells express semiovale bilaterally (figure 1, A and B), as well as Cx32, which likely forms gap junctions between the in the splenium of the corpus callosum (figure 1, C layers of the myelin sheath, thereby providing a and D). These lesions spared the subcortical U fibers shorter pathway for the diffusion of small molecules and did not enhance (not shown). Three-dimensional and ions directly across the myelin sheath.2 Oligo- time-of-flight MR angiography of the intracranial dendrocytes also express Cx32, which participates in vessels, electroencephalography, and CSF were nor- the gap junction coupling of oligodendrocytes and mal, including a normal lactate level (1.1 mmol/L) astrocytes.3 and no oligoclonal bands. -

Full Disclosure Forms
Expanding genotype/phenotype of neuromuscular diseases by comprehensive target capture/NGS Xia Tian, PhD* ABSTRACT * Wen-Chen Liang, MD Objective: To establish and evaluate the effectiveness of a comprehensive next-generation * Yanming Feng, PhD sequencing (NGS) approach to simultaneously analyze all genes known to be responsible for Jing Wang, MD the most clinically and genetically heterogeneous neuromuscular diseases (NMDs) involving spi- Victor Wei Zhang, PhD nal motoneurons, neuromuscular junctions, nerves, and muscles. Chih-Hung Chou, MS Methods: All coding exons and at least 20 bp of flanking intronic sequences of 236 genes causing Hsien-Da Huang, PhD NMDs were enriched by using SeqCap EZ solution-based capture and enrichment method fol- Ching Wan Lam, PhD lowed by massively parallel sequencing on Illumina HiSeq2000. Ya-Yun Hsu, PhD ; 3 Thy-Sheng Lin, MD Results: The target gene capture/deep sequencing provides an average coverage of 1,000 per Wan-Tzu Chen, MS nucleotide. Thirty-five unrelated NMD families (38 patients) with clinical and/or muscle pathologic Lee-Jun Wong, PhD diagnoses but without identified causative genetic defects were analyzed. Deleterious mutations Yuh-Jyh Jong, MD were found in 29 families (83%). Definitive causative mutations were identified in 21 families (60%) and likely diagnoses were established in 8 families (23%). Six families were left without diagnosis due to uncertainty in phenotype/genotype correlation and/or unidentified causative Correspondence to genes. Using this comprehensive panel, we not only identified mutations in expected genes but Dr. Wong: also expanded phenotype/genotype among different subcategories of NMDs. [email protected] or Dr. Jong: Conclusions: Target gene capture/deep sequencing approach can greatly improve the genetic [email protected] diagnosis of NMDs.