Melioidosis in Animals, Thailand, 2006–2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bangkok Anesthesia Regional Training Center
RoleRole ofof BARTCBARTC (Bangkok(Bangkok AnesthesiaAnesthesia RegionalRegional TrainingTraining Center)Center) IInn cooperationcooperation inin educationeducation andand trainingtraining inin developingdeveloping countriescountries ProfProf TharaThara TritrakarnTritrakarn DirectorDirector ofof BARTCBARTC 14th WCA, Cape Town, South Africa, 3/1/2008 Oslo Center, Norway, 12/1/2008 ShortageShortage ofof anesthesiologistsanesthesiologists AA worldwideworldwide problemsproblems MoreMore seriousserious inin developingdeveloping poorpoor countriescountries MarkedMarked variationvariation amongamong countriescountries EconomyEconomy - Most important determining factors - Three levels of wealth & health - Rich countries (per capita GNP > $ 10,000) - Medium to low (GNP $ 1,000-10,000) - Poor countries (GNP < $ 1,000) RichRich && MediumMedium countriescountries GNPGNP PeoplePeople NumberNumber PeoplePeople perper capitacapita perper ofof perper (US(US $)$) doctordoctor anesthetistsanesthetists anesthetistanesthetist USA 33,799 387 23,300 11,500 Japan 34,715 522 4,229 20,000 Singapore 22,710 667 150 26,600 Hong Kong 23,597 772 150 40,000 Australia 19,313 2170 10,000 Malaysia 3,248 1,477 250 88,000 Thailand 1,949 2,461 500 124,000 Philippines 1,048 1,016 1176 64,600 MediumMedium && PoorPoor CountriesCountries GNPGNP PeoplePeople NumberNumber PeoplePeople perper capitacapita perper ofof perper (US(US $)$) doctordoctor anesthetistsanesthetists anesthetistanesthetist Indonesia 617 6,7866,786 350 591,000591,000 Pakistan 492 2,0002,000 400 340,000340,000 -

Cover Tjs 35-4-57
ISSN 0125-6068 TheThai Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand www.surgeons.or.th/ejournal Volume 35 October-December 2014 Number 4 ORIGINAL ARTICLES 121 Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, Porn Narischart 126 Open Surgical Management of Atherosclerotic Aortoiliac Occlusive Diseases (AIOD) Type 1 Anuwat Chantip 130 “Sawanpracharak” Connector: A Single Tube Intercostal Drainage Connector Wanchai Manakijsirisuthi 134 The Trainee’s Operative Experiences for General Surgery in Thailand Potchavit Aphinives CASE REPORT 139 Mitral and Tricuspid Valve Replacement in Uncommon Case of Situs Inversus with Dextrocardia Nuttapon Arayawudhikul, Boonsap Sakboon, Jareon Cheewinmethasiri, Angsu Chartirungsun, Benjamaporn Sripisuttrakul ABSTRACTS 143 Abstracts of the 39th Annual Scientific Congress of the Royal College of Surgeons of Thailand, 10-13 July 2014, Ambassador City Jomtien Hotel, Jomtien, Pattaya, Cholburi, Thailand (Part II) 169 Index Secretariat Office : Royal Golden Jubilee Building, 2 Soi Soonvijai, New Petchaburi Road, Huaykwang, Bangkok 10310, Thailand Tel. +66 2716 6141-3 Fax +66 2716 6144 E-mail: [email protected] www.surgeons.or.th The THAI Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand Vol. 35 October - December 2014 No. 4 Original Article Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, MD Porn Narischart, MD Prasat Neurological Institute, Department of Medical Services, Ministry of Pubic Health, Bangkok, Thailand Abstract Background and Objective: Hydrocephalus is a common problem in neurosurgical field. In current clinical practice guidelines, ventriculoatrial shunt and ventriculoperitoneal shunt are recommended treatment options. No previous study reported differences between two procedures in term of complications and revision rates. -

Reimagine Thailand Hotel Participating List AVISTA GRANDE
Reimagine Thailand Hotel Participating List AVISTA GRANDE PHUKET KARON HOTEL BARAQUDA PATTAYA MGALLERY GRAND MERCURE ASOKE RESIDENCE GRAND MERCURE BANGKOK FORTUNE GRAND MERCURE BANGKOK WINDSOR GRAND MERCURE KHAO LAK GRAND MERCURE PHUKET PATONG HOTEL MUSE BANGKOK LANGSUAN IBIS BANGKOK IMPACT IBIS BANGKOK RIVERSIDE IBIS BANGKOK SATHORN IBIS BANGKOK SIAM IBIS BANGKOK SUKHUMVIT 24 IBIS BANGKOK SUKHUMVIT 4 IBIS HUA HIN IBIS PATTAYA IBIS PHUKET KATA IBIS PHUKET PATONG IBIS SAMUI BOPHUT IBIS STYLES BANGKOK RATCHADA IBIS STYLES BANGKOK SILOM IBIS STYLES BANGKOK SUKHUMVIT 4 IBIS STYLES BANGKOK SUKHUMVIT 50 IBIS STYLES KOH SAMUI CHAWENG IBIS STYLES KRABI AO NANG IBIS STYLES PHUKET CITY MERCURE BANGKOK SIAM MERCURE BANGKOK SUKHUMVIT 24 MERCURE CHIANG MAI MERCURE KOH CHANG HIDEAWAY MERCURE KOH SAMUI BEACH RESORT MERCURE PATTAYA MERCURE PATTAYA OCEAN RESORT MERCURE RAYONG LOMTALAY MOVENPICK ASARA HUA HIN MOVENPICK BANGTAO BEACH PHUKET MOVENPICK RESORT KHAO YAI MOVENPICK SIAM HOTEL PATTA NOVOTEL BANGKOK ON SIAM SQUARE NOVOTEL BANGKOK IMPACT NOVOTEL BANGKOK PLATINUM NOVOTEL BANGKOK SUKHUMVIT 20 NOVOTEL BANGKOK SUKHUMVIT 4 NOVOTEL CHIANGMAI NIMMAN NOVOTEL HUA HIN CHA AM RESORT NOVOTEL PHUKET CITY PHOKEETHRA NOVOTEL RAYONG RIM PAE RESORT NOVOTEL SRIRACHA MARINA BAY NOVOTEL SUITES SUKHUMVIT 34 NOVOTEL SUVARNABHUMI AIRPORT PULLMAN BANGKOK HOTEL G PULLMAN BANGKOK KING POWER PULLMAN KHAO LAK RESORT PULLMAN KHON KAEN RAJA ORCHID PULLMAN PATTAYA HOTEL G PULLMAN PHUKET ARCADIA RESORT PULLMAN PHUKET PANWA SO SOFITEL HUA HIN SO/ BANGKOK SOFITEL BANGKOK SUKHUMVIT SOFITEL KRABI PHOKEETHRA SWISSOTEL BANGKOK RATCHADA VERANDA HIGH RESORT MGALLERY VERANDA RESORT HUA HIN VERANDA RESORT PATTAYA VIE HOTEL BANGKOK MGALLERY *Latest update: 22 Feb 2021 . -

Thailand's First Provincial Elections Since the 2014 Military Coup
ISSUE: 2021 No. 24 ISSN 2335-6677 RESEARCHERS AT ISEAS – YUSOF ISHAK INSTITUTE ANALYSE CURRENT EVENTS Singapore | 5 March 2021 Thailand’s First Provincial Elections since the 2014 Military Coup: What Has Changed and Not Changed Punchada Sirivunnabood* Thanathorn Juangroongruangkit, founder of the now-dissolved Future Forward Party, attends a press conference in Bangkok on January 21, 2021, after he was accused of contravening Thailand's strict royal defamation lese majeste laws. In December 2020, the Progressive Movement competed for the post of provincial administrative organisations (PAO) chairman in 42 provinces and ran more than 1,000 candidates for PAO councils in 52 of Thailand’s 76 provinces. Although Thanathorn was banned from politics for 10 years, he involved himself in the campaign through the Progressive Movement. Photo: Lillian SUWANRUMPHA, AFP. * Punchada Sirivunnabood is Associate Professor in the Faculty of Social Sciences and Humanities of Mahidol University and Visiting Fellow in the Thailand Studies Programme of the ISEAS – Yusof Ishak Institute. 1 ISSUE: 2021 No. 24 ISSN 2335-6677 EXECUTIVE SUMMARY • On 20 December 2020, voters across Thailand, except in Bangkok, elected representatives to provincial administrative organisations (PAO), in the first twinkle of hope for decentralisation in the past six years. • In previous sub-national elections, political parties chose to separate themselves from PAO candidates in order to balance their power among party allies who might want to contest for the same local positions. • In 2020, however, several political parties, including the Phuea Thai Party, the Democrat Party and the Progressive Movement (the successor of the Future Forward Party) officially supported PAO candidates. -

Office of the Board of Investment E-Mail:Head
Office of the Board of Investment 555 Vibhavadi-Rangsit Rd., Chatuchak, Bangkok 10900, Thailand Tel. 0 2553 8111 Fax. 0 2553 8315 http://www.boi.go.th E-mail:[email protected] The Investor Information Services Center Press Release No. 75/2562 (A.36) Tuesday 21st May 2019 On Tuesday 21st May 2019 the Board of Investment has approved 16 projects in the Board's Working-Committee Meeting No. 19/2562 with details as follows: Project Location/ Products/Services Nationalities No. Company Contact (Promotion Activity) of Ownership 1 Ms.Wasana Mongkonrob (Sakon Nakhon) Specialty medical center Thai 126/166 (7.28.2) M.Huansaikam Soi 12 Prabaht Subdistrict Muang District Lampang 2 MEBROM INDUSTRIAL (Bangkok) International Business Chinese COMPANY LIMITED 100/64 Sathorn Nakorn Center: IBC Belgian Tower, 30th Flr., North Sathorn (7.34) Silom Subdistrict Bangrak District Bangkok 3 KLOOK TECHNOLOGY (Bangkok) International Business Singaporean (THAILAND) COMPANY LIMITED 26/46 Orakarn Building, Center: IBC 12th Flr. A (7.34) Soi Chidlom Lumphini Subdistrict Pathumwan District Bangkok Page 1 of 4 Project Location/ Products/Services Nationalities No. Company Contact (Promotion Activity) of Ownership 4 MR. SIMON BUTROS BICHARA (Bangkok) Trade and Investment Support British England Office (7.7) 5 UNITOP RUBBER (Bangkok) Synthetic rubber for industrial Thai COMPANY LIMITED 67 Soi Chalonggrung 31 use Ladkrabang Subdistrict (6.6) Lamplatiew District Bangkok 6 SEITEK INTERNATIONAL (Chonburi) Electrical appliances with Chinese (THAILAND) COMPANY LIMITED 475/3 m.7 advanced technology and WHA Industrial Estate product design process Eastern Seaboard 2 (5.1.1.1) Banbueng District Chonburi 7 SUGINO PRESS (THAILAND) (Rayong) Metal pressed parts n/a COMPANY LIMITED 64/158 m.4 (4.1.3) Pluagdang Sub-/District Rayong 8 MR. -

Youthquake Evokes the 1932 Revolution and Shakes Thailand's
ISSUE: 2020 No. 127 ISSN 2335-6677 RESEARCHERS AT ISEAS – YUSOF ISHAK INSTITUTE ANALYSE CURRENT EVENTS Singapore | 6 November 2020 Youthquake Evokes the 1932 Revolution and Shakes Thailand’s Establishment Supalak Ganjanakhundee* EXECUTIVE SUMMARY • Grievance and frustration resulting from the government’s authoritarian style, its restrictions on freedom of expression and the dissolution of the Future Forward Party have been accumulating among students and youths in Thailand since the 2014 military coup. • While high school and college students are overwhelmingly represented among participants in the ongoing protests, young people from various other sectors across the country have also joined the demonstrations. • The flash-mob style of demonstration is a venting of anger against the political system, expressed in calls for the resignation of Prime Minister Prayut Chan-ocha, a new Constitution and, more importantly, reform of the Thai monarchy. • The protests are a flashback to the 1932 Revolution, in that they are conveying the message that ordinary people, not the traditional establishment, own the country and have the legitimate right to determine its future course. • In response, the crown and the royalists are using traditional methods of smears and labels to counteract the youths. * Supalak Ganjanakhundee was Visiting Fellow in the Thailand Studies Programme, ISEAS – Yusof Ishak Institute from 1 October 2019 to 30 June 2020. He is the former editor of The Nation (Bangkok). 1 ISSUE: 2020 No. 127 ISSN 2335-6677 INTRODUCTION A number of Thais have gathered annually at Thammasat University’s Tha Phrachan campus and at the 14 October 1973 Memorial site on nearby Ratchadamnoen Avenue to commemorate the student uprising on that date which restored democracy to the country. -

24/7 Emergency Operation Center for Flood, Storm and Landslide
No. 17/2011, Saturday September 10, 2011, 11:00 AM 24/7 Emergency Operation Center for Flood, Storm and Landslide DATE: Saturday, September 10, 2011 TIME: 09.00 LOCATION: Meeting Room 2, Ministry of Interior CHAIRPERSON: Mr. Chatpong Chatraphuti Deputy Director-General, Department of Disaster Prevention and Mitigation 1. CURRENT SITUATION 1.1 Current flooded provinces: there are 14 recent flooded provinces: Sukhothai, Phichit, Phitsanulok, Nakhon Sawan, Phra Nakhon Si Ayutthaya, Ang Thong, Chai Nat, Ubon Ratchathani, Sing Buri, Nakhon Pathom,, Suphan Buri, Nonthaburi, Uthai Thani and Chacheongsao. The total of 65 Districts, 483 Sub-Districts, 2,942 Villages, 186,045 families and/or 476,775 people are affected by the flood. The total fatalities are 72 deaths and 1 missing. (Fatalities: 1 in Udon Thani, Sakon Nakhon, Uttaradit, Phetchabun, Suphan Buri; 2 in Tak, Nakhon Phanom, Roi Et, and Phang-Nga; 3 in Chiang Mai; 4 in Prachin Buri, Nakhon Sawan; 5 in Phitsanulok; 7 in Mae Hong Son and Sukhothai; 8 in Phrae; and 21 in Phichit: Missing: 1 in Mae Hong Son due to landslide) 1.2 Weather Condition: The active monsoon trough lies over the Central, Northeast and East of Thailand. The strong southwest monsoon prevails over the Andaman Sea, southern Thailand and the Gulf of Thailand. Torrential rain is likely over upper Thailand and isolated heavy to very heavy falls in the Northeast and the East. People in the low land and the riverside in the Central and the East should beware of flooding during the period. (Thai Meteorological Department : TMD) 1.3 Amount of Rainfall: The heaviest rainfall in the past 24 hours is at Phubphlachai District, Burirum Province at 126.5 mm. -

THAILAND Last Updated: 2006-12-05
Vitamin and Mineral Nutrition Information System (VMNIS) WHO Global Database on Anaemia The database on Anaemia includes data by country on prevalence of anaemia and mean haemoglobin concentration THAILAND Last Updated: 2006-12-05 Haemoglobin (g/L) Notes Age Sample Proportion (%) of population with haemoglobin below: Mean SD Method Reference General Line Level Date Region and sample descriptor Sex (years) size 70 100 110 115 120 130 S 2002 Ubon Ratchathani province: SAC B 6.00- 12.99 567 C 5227 * 1 LR 1999 Songkhla Province: Hat Yai rural area: SAC: Total B 6.00- 13.99 397 A 3507 * 2 Songkhla Province: Hat Yai rural area: SAC by inter B 6.00- 13.99 140 121 10 3 Songkhla Province: Hat Yai rural area: SAC by inter B 6.00- 13.99 134 121 9 4 Songkhla Province: Hat Yai rural area: SAC by inter B 6.00- 13.99 123 122 10 5 S 1997P Northeast-Thailand: Women F 15.00- 45.99 607 17.3 A 2933 * 6 SR 1996 -1997 Sakon Nakhon Province: All B 1.00- 90.99 837 132 14 A 3690 * 7 Sakon Nakhon Province: Adults: Total B 15.00- 60.99 458 139 14 8 Sakon Nakhon Province: Elderly: Total B 61.00- 90.99 35 113 11 9 Sakon Nakhon Province: Children: Total B 1.00- 14.99 344 129 13 10 Sakon Nakhon Province: All by sex F 1.00- 90.99 543 11 Sakon Nakhon Province: All by sex M 1.00- 90.99 294 12 Sakon Nakhon Province: Adults by sex F 15.00- 60.99 323 13 Sakon Nakhon Province: Adults by sex M 15.00- 60.99 135 14 Sakon Nakhon Province: Children by sex F 1.00- 14.99 194 15 Sakon Nakhon Province: Children by sex M 1.00- 14.99 150 16 L 1996P Chiang Mai: Pre-SAC B 0.50- 6.99 340 -

11661287 31.Pdf
The Study on the Integrated Regional Development Plan for the Northeastern Border Region in the Kingdom of Thailand Sector Plan: Chapter16 Transportation CHAPTER 16 TRANSPORTATION 16.1 International and Inter-Urban Transport System of Thailand 16.1.1 National Highway System in Thailand The DOH1 network of national highways has a total route length of approximately 55,000 km, of which there are about 20,000 km of 1-, 2- and 3-digit roads and 30,000 km of 4-digit roads. All provinces (changwats) are connected to this network and most long-distance (inter-province) traffic uses these roads. Table 16.1 Highway Classification by Numbering System 1-digit route Highway Route No.1: Bangkok - Chiangrai (Phaholyothin Road) Highway Route No.2: Saraburi - Nongkai (Friendship Road) Highway Route No.3: Bangkok - Trad (Sukhumvit Road) Highway Route No.4: Bangkok - Amphoe Sadao, Songkla (Petchkasem Road) 2- digit route Primary highway in the regions 3-digit route Secondary highway in the regions 4-digit route Highway linking Changwat and Amphoe or important places in that province. Source: Department of Highways, Ministry of Transport and Communications 1 Department of Highway, Ministry of Transport and Communication, Thailand 16-1 PLANET NESDB - JICA Table 16.2 Highway Classification by Jurisdiction (1) Special Highway and Highways registered at the Department of Highways (DOH) by the order of National Highway the Director-General with the approval of the Minister. Highways registered at the Department of Highways (DOH) by the order of (2) Concession Highways the Director-General with the approval of the Minister. Roads registered at Provincial City Hall by the order of the Governor with (3) Rural Roads the consent of the Director-General of the Public Works, Department of the Secretary-General of the Office of the Accelerated Rural Development. -

Final Project Report English Pdf 463.15 KB
CEPF Final Project Completion Report Organization Legal Name Bird Conservation Society of Thailand Project Title Building a Network for Monitoring Important Bird Areas in Thailand CEPF GEM No. CEPF-032-2014 Date of Report Report Author Thattaya Bidayabha 221 Moo 2 Soi Ngamwongwan 27 Ngamwongwan Road, Bangkhen, Muang, Nonthaburi 11000 Thailand Author Contact Information Tel.: +66 2 588 2277 Fax: +66 2 588 2277 E-mail: [email protected] CEPF Region: Indo-Burma Strategic Direction: Strategic Direction 8: "Strengthen the capacity of civil society to work on biodiversity, communities and livelihoods at regional, national, local and grassroots levels" Grant Amount: $19,999 Project Dates: November 1st, 2014 to October 31st, 2015 1. Implementation Partners for this Project Department of National Parks, Wildlife, and Plant Conservation - the government agency that is responsible for the management of and law enforcement in protected areas. Universities - Kasetsart University, Chiang Mai University, Khon Kaen University, and Walailuck University hosted the IBA monitoring workshops. Local Conservation Clubs; - Khok Kham Conservation Club, Khok Kham district, Samut Sakhon province. They were involved in IBA monitoring in the Inner Gulf of Thailand - Lanna Bird Club, Chiang Mai province. They were involved in IBA monitoring in northern Thailand. - Nan Birding Club, Nan province. They were involved in IBA monitoring in northern Thailand. - Mae Moh Bird Conservation Club, Lampang province. They were involved in IBA monitoring in northern Thailand. - Chun Conservation Club, Phayao province. They were involved in IBA monitoring in northern Thailand. - Flyway Foundation, Chumphon province. They were involved in IBA monitoring in southern Thailand. - Khao Luang Bird Conservation Club, Nakhon Sri Thammarat province. -

Gallbladder and Extrahepatic Bile Duct
Surathat Pongnikorn, Nimit Martin Gallbladder and Extrahepatic Bile Duct In Thailand during the period males (377 cases) in a ratio of 1.9:1. 1995-1997, carcinoma of gallblad- Gallbladder cancer and extra- Chapter II der and extrahepatic duct is not in- hepatic bile duct carcinoma are the cluded in the top ten of the most tenth in frequency in Lampang in frequency. The estimated inci- both males (ASR = 3.6) and fe- dence rate is 1.6 per 100 000 among males (ASR = 3.3) which is the males and 2.4 per 100 000 among highest incidence rate among five females. Females (728 cases) are centers. Female are affected more affected by gallbladder and extra- than males in Chiang Mai, Bang- 8 hepatic bile duct cancer more than kok and Songkhla although in Figure 2.8.1 Gallbladder and extrahepatic bile duct cancer in different regions, 1995- GALLBLADDER 1997 AND EXTRAHEPATIC Male *USA, New Maxico 4.3 BILE DUCT American Indian ICD-10 C23-24 Thailand 1.6 Chiang Mai 1.5 Surathat Pongnikorn, M.D. Nimit Martin, M.D. Lampang 3.6 Khon Kaen 1.9 Bangkok 1.2 Songkhla 0.9 0510 ASR (World) Female *India, Delhi 8.8 Thailand 2.4 Chiang Mai 3.2 Lampang 3.3 Khon Kaen 1.6 Bangkok 1.4 Songkhla 1.1 0510 ASR (World) *The highest incidence in CI5 Vol. VIII 38 p. 38-¥” Gallbladder and Extrahepatic Bile Duct Surathat Pongnikorn, Nimit Martin Lampang and Khon Kaen males are Figure 2.8.2 Age-specific incidence rates of gallbladder and extrahepatic bile duct affected more than females. -
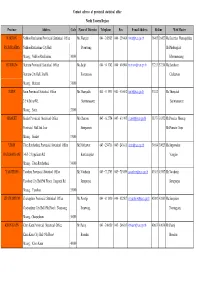
Province Address Code Name of Director Telephone Fax E-Mail
Contact adrress of provincial statistical office North Eastern Region Province Address Code Name of Director Telephone Fax E-mail AddressHotline Web Master NAKHON Nakhon Ratchasima Provincial Statistical Office Ms.Wanpen 044 - 242985 044 - 256406 [email protected] 36465 36427 Ms.Kanittha Wannapakdee RATCHASIMA Nakhon Ratchasima City Hall Poonwong Mr.Phadungkiat Muang , Nakhon Ratchasima 30000 Khmmamuang BURIRUM Burirum Provincial Statistical Office Ms.Saijit 044 - 611742 044 - 614904 [email protected] 37213 37214 Ms.Somboon Burirum City Hall, Jira Rd. Kootaranon Chaleewan Muang , Burirum 31000 SURIN Surin Provincial Statistical Office Ms.Thanyalak 044 - 511931 044 - 516062 [email protected] 37812 Ms.Thanyalak 2/5-6 Sirirat Rd. Surintarasaree Surintarasaree Muang , Surin 32000 SISAKET Sisaket Provincial Statistical Office Mr.Charoon 045 - 612754 045 - 611995 [email protected] 38373 38352 Mr.Preecha Meesup Provincial Hall 2nd floor Siengsanan Mr.Pramote Sopa Muang , Sisaket 33000 UBON Ubon Ratchathani Provincial Statistical Office Mr.Natthawat 045 - 254718 045 - 243811 [email protected] 39014 39023 Ms.Supawadee RATCHATHANI 146/1-2 Uppalisarn Rd. Kanthanaphat Vonglao Muang , Ubon Ratchathani 34000 YASOTHON Yasothon Provincial Statistical Office Mr.Vatcharin 045 - 712703 045 - 713059 [email protected] 43563 43567 Mr.Vatcharin Yasothon City Hall(5th Floor), Jangsanit Rd. Jermprapai Jermprapai Muang , Yasothon 35000 CHAIYAPHUM Chaiyaphum Provincial Statistical Office Ms.Porntip 044 - 811810 044 - 822507 [email protected] 42982 42983 Ms.Sanyakorn