(Pteropus Lylei) in Thailand
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fruit Bats As Natural Foragers and Potential Pollinators in Fruit Orchard: a Reproductive Phenological Study
Journal of Agricultural Research, Development, Extension and Technology, 25(1), 1-9 (2019) Full Paper Fruit bats as natural foragers and potential pollinators in fruit orchard: a reproductive phenological study Camelle Jane D. Bacordo, Ruffa Mae M. Marfil and John Aries G. Tabora Department of Biological Sciences, College of Arts and Sciences, University of Southern Mindanao, Kabacan, Cotabato, Philippines Received: 27 February 2019 Accepted: 10 June 2019 Abstract Family Pteropodidae could consume either fruit or flower parts to sustain their energy requirement. In some species of fruit bats, population growth is sometimes dependent on the food availability and in return bats could be pollinators of certain species of plants. In this study, 152 female bats captured from the Manilkara zapota orchard of the University of Southern Mindanao were examined for their reproductive stages. Lactation of fruit bat species Ptenochirus jagori and Ptenochirus minor were positively correlated with the fruiting of M. zapota. While the lactation of Cynopterus brachyotis, Eonycteris spelaea and Rousettus amplexicaudatus were positively associated with the flowering of M. zapota. Together, thirty M. zapota trees were observed for their generative stage (fruiting or flowering) in 6 months. Based on the canonical correspondence analysis, only P. jagori was considered as the natural forager as its lactating stage coincides with the fruiting peaks and only C. brachyotis and E. spelaea were the potential pollinators since its lactating stage coincides with the flowering peaks ofM. zapota tree. The method in this study can be used to identify potential pollinators and foragers in other fruit trees. Keywords - agroforest, chiropterophily, frugivore, nocturnal, Sapotaceae Introduction pollination process is called chiropterophily. -

Chiroptera: Pteropodidae)
Chapter 6 Phylogenetic Relationships of Harpyionycterine Megabats (Chiroptera: Pteropodidae) NORBERTO P. GIANNINI1,2, FRANCISCA CUNHA ALMEIDA1,3, AND NANCY B. SIMMONS1 ABSTRACT After almost 70 years of stability following publication of Andersen’s (1912) monograph on the group, the systematics of megachiropteran bats (Chiroptera: Pteropodidae) was thrown into flux with the advent of molecular phylogenetics in the 1980s—a state where it has remained ever since. One particularly problematic group has been the Austromalayan Harpyionycterinae, currently thought to include Dobsonia and Harpyionycteris, and probably also Aproteles.Inthis contribution we revisit the systematics of harpyionycterines. We examine historical hypotheses of relationships including the suggestion by O. Thomas (1896) that the rousettine Boneia bidens may be related to Harpyionycteris, and report the results of a series of phylogenetic analyses based on new as well as previously published sequence data from the genes RAG1, RAG2, vWF, c-mos, cytb, 12S, tVal, 16S,andND2. Despite a striking lack of morphological synapomorphies, results of our combined analyses indicate that Boneia groups with Aproteles, Dobsonia, and Harpyionycteris in a well-supported, expanded Harpyionycterinae. While monophyly of this group is well supported, topological changes within this clade across analyses of different data partitions indicate conflicting phylogenetic signals in the mitochondrial partition. The position of the harpyionycterine clade within the megachiropteran tree remains somewhat uncertain. Nevertheless, biogeographic patterns (vicariance-dispersal events) within Harpyionycterinae appear clear and can be directly linked to major biogeographic boundaries of the Austromalayan region. The new phylogeny of Harpionycterinae also provides a new framework for interpreting aspects of dental evolution in pteropodids (e.g., reduction in the incisor dentition) and allows prediction of roosting habits for Harpyionycteris, whose habits are unknown. -
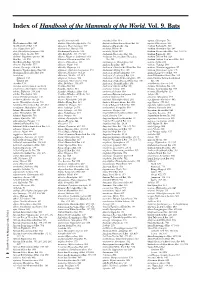
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -

Social Structure of a Polygynous Tent-Making Bat, Cynopterus Sphinx (Megachiroptera)
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Jay F. Storz Publications Papers in the Biological Sciences 6-2000 Social structure of a polygynous tent-making bat, Cynopterus sphinx (Megachiroptera) Jay F. Storz University of Nebraska - Lincoln, [email protected] Hari Bhat National Institute of Virology, Pune, 411 001, India Thomas H. Kunz Boston University, 5 Cummington Street, Boston, MA Follow this and additional works at: https://digitalcommons.unl.edu/bioscistorz Part of the Genetics and Genomics Commons Storz, Jay F.; Bhat, Hari; and Kunz, Thomas H., "Social structure of a polygynous tent-making bat, Cynopterus sphinx (Megachiroptera)" (2000). Jay F. Storz Publications. 30. https://digitalcommons.unl.edu/bioscistorz/30 This Article is brought to you for free and open access by the Papers in the Biological Sciences at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Jay F. Storz Publications by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Published in Journal of Zoology 251:2 (June 2000), pp. 151–165; doi 10.1111/j.1469-7998.2000.tb00600.x Copyright © 2000 The Zoological Society of London; published by Blackwell Publishing. Used by permission. http://www3.interscience.wiley.com/journal/118535410/home Accepted for publication June 2, 1999. Social structure of a polygynous tent-making bat, Cynopterus sphinx (Megachiroptera) Jay F. Storz,1 Hari R. Bhat,2 and Thomas H. Kunz 1 1 Department of Biology, Boston University, 5 Cummington Street, Boston, MA 02215, USA 2 National Institute of Virology, Pune, 411 001, India; present address: 107 Awanti, OPP: Kamala Nehru Park, Erandawana, Pune, 411 004, India Abstract The social structure of an Old World tent-making bat Cynopterus sphinx (Megachiroptera), was investigated in western India. -

Taxonomy and Natural History of the Southeast Asian Fruit-Bat Genus Dyacopterus
Journal of Mammalogy, 88(2):302–318, 2007 TAXONOMY AND NATURAL HISTORY OF THE SOUTHEAST ASIAN FRUIT-BAT GENUS DYACOPTERUS KRISTOFER M. HELGEN,* DIETER KOCK,RAI KRISTIE SALVE C. GOMEZ,NINA R. INGLE, AND MARTUA H. SINAGA Division of Mammals, National Museum of Natural History (NHB 390, MRC 108), Smithsonian Institution, P.O. Box 37012, Washington, D.C. 20013-7012, USA (KMH) Forschungsinstitut Senckenberg, Senckenberganlage 25, Frankfurt, D-60325, Germany (DK) Philippine Eagle Foundation, VAL Learning Village, Ruby Street, Marfori Heights, Davao City, 8000, Philippines (RKSCG) Department of Natural Resources, Cornell University, Ithaca, NY 14853, USA (NRI) Division of Mammals, Field Museum of Natural History, Chicago, IL 60605, USA (NRI) Museum Zoologicum Bogoriense, Jl. Raya Cibinong Km 46, Cibinong 16911, Indonesia (MHS) The pteropodid genus Dyacopterus Andersen, 1912, comprises several medium-sized fruit-bat species endemic to forested areas of Sundaland and the Philippines. Specimens of Dyacopterus are sparsely represented in collections of world museums, which has hindered resolution of species limits within the genus. Based on our studies of most available museum material, we review the infrageneric taxonomy of Dyacopterus using craniometric and other comparisons. In the past, 2 species have been described—D. spadiceus (Thomas, 1890), described from Borneo and later recorded from the Malay Peninsula, and D. brooksi Thomas, 1920, described from Sumatra. These 2 nominal taxa are often recognized as species or conspecific subspecies representing these respective populations. Our examinations instead suggest that both previously described species of Dyacopterus co-occur on the Sunda Shelf—the smaller-skulled D. spadiceus in peninsular Malaysia, Sumatra, and Borneo, and the larger-skulled D. -

Habitat Selection of Endangered and Endemic Large Flying-Foxes in Subic
Biological Conservation 126 (2005) 93–102 www.elsevier.com/locate/biocon Habitat selection of endangered and endemic large Xying-foxes in Subic Bay, Philippines Tammy L. Mildenstein a,¤, Sam C. Stier a, C.E. Nuevo-Diego b, L. Scott Mills c a c/o US Peace Corps, Patio Madrigal Compound, 2775 Roxas Blvd., Pasay City, Metro Manila, Philippines b 9872 Isarog St. Umali Subdivision, Los Baños, Laguna 4031, Philippines c Wildlife Biology Program, School of Forestry, University of Montana, Missoula, MT 59812-0596, USA Received 6 June 2004 Available online 5 July 2005 Abstract Large Xying-foxes in insular Southeast Asia are the most threatened of the Old World fruit bats due to high levels of deforestation and hunting and eVectively little local conservation commitment. The forest at Subic Bay, Philippines, supports a rare, large colony of vulnerable Philippine giant fruit bats (Pteropus vampyrus lanensis) and endangered and endemic golden-crowned Xying-foxes (Acerodon jubatus). These large Xying-foxes are optimal for conservation focus, because in addition to being keystone, Xagship, and umbrella species, the bats are important to Subic Bay’s economy and its indigenous cultures. Habitat selection information stream- lines management’s eVorts to protect and conserve these popular but threatened animals. We used radio telemetry to describe the bats’ nighttime use of habitat on two ecological scales: vegetation and microhabitat. The fruit bats used the entire 14,000 ha study area, including all of Subic Bay Watershed Reserve, as well as neighboring forests just outside the protected area boundaries. Their recorded foraging locations ranged between 0.4 and 12 km from the roost. -

Galorio A. H. N., Nuneza O. M., 2014 Diet of Cave-Dwelling Bats In
ABAH BIOFLUX Animal Biology & Animal Husbandry International Journal of the Bioflux Society Diet of cave-dwelling bats in Bukidnon and Davao Oriental, Philippines Al H. N. Galorio, Olga M. Nuñeza Department of Biological Sciences, College of Science and Mathematics, Mindanao State University - Iligan Institute of Technology, Iligan City, Philippines. Corresponding author: O. M. Nuñeza, [email protected] Abstract. The Philippine archipelago has high species richness of bats, many of which are cave-dwellers. Information on the feeding behavior of these species is important toward their conservation. This study was conducted to determine the diet of 8 species of cave-dwelling bats from 13 cave sites in Mindanao, Philippines based on percentage occurrence of the diet items in the gut contents. Among the frugivorous species, Rousettus amplexicaudatus had the highest percentage occurrence of fruit bits (73.68 %) and fruit fibers (36.84 %) suggesting high fruit consumption. Some individuals of Cynopterus brachyotis were found to consume Ficus sp. seeds while a Ptenochirus jagori individual had an unidentified seed in the gut. Insect limbs were present in the diet of R. amplexicaudatus and P. jagori. Presence of insects in these fruit-eating bats implies that these bats might have consumed fruits along with the insects associated with the fruits. Among the insect-eating bats, digested insect parts, wings, limbs, and exoskeletons of Hymenoptera, Formicidae, Orthoptera, and Scotinophara sp. were observed in their gut. Fruit bits and fruit fibers observed in Hipposideros diadema, Miniopterus schreibersii and Taphozous melanopogon suggest that these bats consumed insects as well as fruits or fruits associated with certain insects. -

Bats of the Philippine Islands –A Review of Research Directions and Relevance to National- 2 Level Priorities and Targets 3 Krizler Cejuela
1 Bats of the Philippine Islands –a review of research directions and relevance to national- 2 level priorities and targets 3 Krizler Cejuela. Tanalgo & Alice Catherine Hughes 4 Landscape Ecology Group, Centre for Integrative Conservation, Xishuangbanna Tropical Botanical Garden, 5 Chinese Academy of Sciences, Yunnan, P.R. China 6 7 Abstract 8 Effective science-based conservation priorities and policies are crucially important to 9 effectively maintain biodiversity into the future. For many threatened species and systems 10 insufficient information exists to generate priorities, or the mechanisms needed to effectively 11 conserve species into the future, and this is especially important in megadiversity countries like 12 the Philippines, threatened by rapid rates of development and with few overarching strategies 13 to maintain their biodiversity. Here, using a bibliographic approach to indicate research 14 strengths and priorities, we summarised scientific information on Philippine bats from 2000- 15 2017. We examine relationships between thematic areas and effort allocated for each species 16 bat guild, and conservation status. We found that an average of 7.9 studies was published 17 annually with the majority focused on diversity and community surveys. However, research 18 effort is not even between taxonomic groups, thematic areas or species, with disproportionate 19 effort focusing on ‘taxonomy and systematics’ and ‘ecology’. Species effort allocation between 20 threatened and less threatened species does not show a significant difference, though this may 21 be because generalist species are found in many studies, whereas rarer species have single 22 species studies devoted to them. A growing collaborative effort in bat conservation initiatives 23 in the Philippines has focused on the protection of many endemic and threatened species (e.g., 24 flying foxes) and their habitats. -
STAAR Biology May 2021 RELEASED
STAAR® State of Texas Assessments of Academic Readiness Biology Administered May 2021 RELEASED Copyright © 2021, Texas Education Agency. All rights reserved. Reproduction of all or portions of this work is prohibited without express written permission from the Texas Education Agency. BIOLOGY Biology Page 3 DIRECTIONS Read each question carefully. Determine the best answer to the question from thefouranswerchoicesprovided.Thenfill in theansweronyouranswer document. 1 When the skin comes in contact with an irritant, receptors in the skin send signals to the spinal cord. The signal is then sent to the brain for processing, and the individual begins to scratch the affected area. Which two systems are most likely interacting when a person experiences itching caused by a skin irritant? A Circulatory and excretory B Integumentary and nervous C Digestive and muscular D Respiratory and lymphatic 2 During the cell cycle, proteins called cyclins bind to enzymes that send signals for the cell to progress through stages of cell replication. At the end of this cycle, the cyclins degrade to prevent further signaling for the cell to divide. Uncontrolled production of cyclins will most likely result in — F the formation of tumors G the immediate death of the cell H the transfer of cyclins to other cells J the formation of haploid cells Biology Page 4 3 An illustration of how a particular DNA mutation will most likely affect the polypeptide produced is shown. Original DNA strand 3’ 5’ GT AGT AG T AGT AG T AGT AG T A His His His His His His His Mutated DNA strand 3’ 5’ GT AGT AG T AG G AG T AGT AG T A His His His Pro His His His What type of mutation is illustrated? A Insertion B Translocation C Substitution D Deletion 4 Farmers spray pesticides on their plants to protect the plants from being eaten by insects. -

Anthropogenic Impacts on Cave-Roosting Bats
Available online athttp://www.ssstj.sci.ssru.ac.th Suan Sunandha Science and Technology Journal ©2018 Faculty of Science and Technology, Suan Sunandha Rajabhat University __________________________________________________________________________________ Anthropogenic Impacts on Cave-roosting Bats: A Call for Conservation Policy Implementation in Bukidnon, Philippines Kim-Lee Bustillo Domingo, Dave Paladin Buenavista* Department of Biology, Central Mindanao University, Musuan, Bukidnon 8710, Philippines Corresponding author e-mail: *[email protected] Abstract Many caves in the Philippines are amongst the most popular natural ecotourism sites, even though most of them are poorly regulated and understudied. This study investigates the anthropogenic impacts of unsustainable eco- tourism and exploitation on cave-roosting bats in Sumalsag Cave, Bukidnon, Mindanao Island, Philippines. The species richness of the cave-roosting bat fauna was determined using the standard mist-netting method and capture-mark and release technique. The conservation status was assessed based on the International Union for Conservation of Nature (IUCN) Red List. Ecological evaluation and assessment of the cave’s speleological characteristics and ecological condition was carried out using the Philippines’ standard cave assessment protocol. After completing 15 net-nights field sampling with a capture effort of 180 net/hours, results revealed a total of six (6) species of cave-roosting bats which belongs to three (3) families. Two Philippine endemic species, Ptenochirus jagori and Ptenochirus minor were documented including Miniopterus schreibersii, a species classified under near threatened category. Evidence of human activities were considered for identifying the indirect and direct threats on the bat fauna. Destroyed speleothems and speleogens, excavations, modifications of the cave’s features as well as graffiti in the cave walls were recorded. -

List of Taxa for Which MIL Has Images
LIST OF 27 ORDERS, 163 FAMILIES, 887 GENERA, AND 2064 SPECIES IN MAMMAL IMAGES LIBRARY 31 JULY 2021 AFROSORICIDA (9 genera, 12 species) CHRYSOCHLORIDAE - golden moles 1. Amblysomus hottentotus - Hottentot Golden Mole 2. Chrysospalax villosus - Rough-haired Golden Mole 3. Eremitalpa granti - Grant’s Golden Mole TENRECIDAE - tenrecs 1. Echinops telfairi - Lesser Hedgehog Tenrec 2. Hemicentetes semispinosus - Lowland Streaked Tenrec 3. Microgale cf. longicaudata - Lesser Long-tailed Shrew Tenrec 4. Microgale cowani - Cowan’s Shrew Tenrec 5. Microgale mergulus - Web-footed Tenrec 6. Nesogale cf. talazaci - Talazac’s Shrew Tenrec 7. Nesogale dobsoni - Dobson’s Shrew Tenrec 8. Setifer setosus - Greater Hedgehog Tenrec 9. Tenrec ecaudatus - Tailless Tenrec ARTIODACTYLA (127 genera, 308 species) ANTILOCAPRIDAE - pronghorns Antilocapra americana - Pronghorn BALAENIDAE - bowheads and right whales 1. Balaena mysticetus – Bowhead Whale 2. Eubalaena australis - Southern Right Whale 3. Eubalaena glacialis – North Atlantic Right Whale 4. Eubalaena japonica - North Pacific Right Whale BALAENOPTERIDAE -rorqual whales 1. Balaenoptera acutorostrata – Common Minke Whale 2. Balaenoptera borealis - Sei Whale 3. Balaenoptera brydei – Bryde’s Whale 4. Balaenoptera musculus - Blue Whale 5. Balaenoptera physalus - Fin Whale 6. Balaenoptera ricei - Rice’s Whale 7. Eschrichtius robustus - Gray Whale 8. Megaptera novaeangliae - Humpback Whale BOVIDAE (54 genera) - cattle, sheep, goats, and antelopes 1. Addax nasomaculatus - Addax 2. Aepyceros melampus - Common Impala 3. Aepyceros petersi - Black-faced Impala 4. Alcelaphus caama - Red Hartebeest 5. Alcelaphus cokii - Kongoni (Coke’s Hartebeest) 6. Alcelaphus lelwel - Lelwel Hartebeest 7. Alcelaphus swaynei - Swayne’s Hartebeest 8. Ammelaphus australis - Southern Lesser Kudu 9. Ammelaphus imberbis - Northern Lesser Kudu 10. Ammodorcas clarkei - Dibatag 11. Ammotragus lervia - Aoudad (Barbary Sheep) 12. -

Exploitation of Bats for Bushmeat and Medicine
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Chapter 12 Exploitation of Bats for Bushmeat and Medicine Tammy Mildenstein, Iroro Tanshi and Paul A. Racey Abstract Bat hunting for consumption as bushmeat and medicine is widespread and affects at least 167 species of bats (or c. 13 % of the world’s bat species), in Africa, Asia, across the islands of Oceania, and to a lesser extent in Central and South America. Hunting is particularly prevalent among the large-bodied fruit bats of the Old World tropics, where half (50 %, 92/183) the extant species in the family Pteropodidae are hunted. Pteropodids that are hunted are six times more likely to be Red Listed as threatened: 66 % of species in IUCN threatened categories (CR, EN, VU, NT), compared to 11 % of species in the ‘Least Concern’ (LC) category. However, there still appears to be an information gap at the international level. One third of the hunted species on the Red List are not considered threatened by that hunting, and nearly a quarter of the bat species included in this review are not listed as hunted in IUCN Red List species accounts. This review has resulted in a com- prehensive list of hunted bats that doubles the number of species known from either the IUCN Red List species accounts or a questionnaire circulated in 2004. More research is needed on the impacts of unregulated hunting, as well as on the sustain- ability of regulated hunting programs. In the absence of population size and growth data, legislators and managers should be precautionary in their attitude towards T.