Nano-Engineered Scaffold for Osteoarticular Regenerative Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nanotechnology Measurement Handbook a Guide to Electrical Measurements for Nanoscience Applications Nanotechnology Measurement Handbook Nanotechnology
NanoCov_grn.tiff 12/13/07 10:47 AM Page 1 www.keithley.com st 1Edition Nanotechnology Measurement Handbook A Guide to Electrical Measurements for Nanoscience Applications Nanotechnology Measurement Handbook Specifications are subject to change without notice. All Keithley trademarks and trade names are the property of Keithley Instruments, Inc. All other trademarks and trade names are the property of their respective companies. Keithley Instruments, Inc. Corporate Headquarters • 28775 Aurora Road • Cleveland, Ohio 44139 • 440-248-0400 • Fax: 440-248-6168 • 1-888-KEITHLEY (534-8453) www.keithley.com 1 st Edition © Copyright 2007 Keithley Instruments, Inc. No. 2819 Printed in the U.S.A. 020731KIPC Nanotechnology Measurement Handbook A Guide to Electrical Measurements for Nanoscience Applications 1st Edition A GREATER MEASURE OF CONFIDENCE Foreword Nanotechnology research often demands skills in multiple disciplines, from phys- ics and materials science to chemistry and measurement system design. Although it would be impossible to predict all the technical innovations that nano research will offer, it’s already clear that nanoscience will be a major driver of the economy of the future. However, characterizing tomorrow’s nanoscale components and materials will be far from trivial because many of their electrical properties lie at the very edge of the measurement envelope. To unravel tiny mysteries and turn nanoscale materials and devices into commercial products, researchers must have tools with the flexibility to handle a variety of electrical measurements, including current vs. voltage (I-V) characterization, resistance, resistivity and conductivity, differential conductance, transport, and optical spectrum and energy. They must also gain an in-depth understanding of the principles and pitfalls associated with low-level electrical measurements. -

Controlling Nanoparticle Dispersion for Nanoscopic Self-Assembly
CONTROLLING NANOPARTICLE DISPERSIONS FOR NANOSCOPIC SELF- ASSEMBLY A Project Report presented to the Faculty of California Polytechnic State University, San Luis Obispo In Partial Fulfillment of the Requirements for the Degree Master of Science in Polymers and Coatings by Nathan Stephen Starkweather March 2013 © 2013 Nathan Stephen Starkweather ALL RIGHTS RESERVED ii COMMITTEE MEMBERSHIP TITLE: Controlling Nanoparticle Dispersions for Nanoscopic Self- Assembly AUTHOR: Nathan Stephen Starkweather DATE SUBMITTED: March 2013 COMMITTEE CHAIR: Raymond H. Fernando, Ph.D. COMMITTEE MEMBER: Shanju Zhang, Ph.D. COMMITTEE MEMBER: Chad Immoos, Ph.D. iii ABSTRACT Controlling Nanoparticle Dispersions for Nanoscopic Self-Assembly Nathan Stephen Starkweather Nanotechnology is the manipulation of matter and devices on the nanometer scale. Below the critical dimension length of 100nm, materials begin to display vastly different properties than their macro- or micro- scale counterparts. The exotic properties of nanomaterials may trigger the start of a new technological revolution, similar to the electronics revolution of the late 20th century. Current applications of nanotechnology primarily make use of nanoparticles in bulk, often being made into composites or mixtures. While these materials have fantastic properties, organization of nano and microstructures of nanoparticles may allow the development of novel devices with many unique properties. By analogy, bulk copper may be used to form the alloys brass or bronze, which are useful materials, and have been used for thousands of years. Yet, organized arrays of copper allowed the development of printed circuit boards, a technology far more advanced than the mere use of copper as a bulk material. In the same way, organized assemblies of nanoparticles may offer technological possibilities far beyond our current understanding. -
![Arxiv:2005.01804V1 [Q-Bio.QM] 1 May 2020](https://docslib.b-cdn.net/cover/3679/arxiv-2005-01804v1-q-bio-qm-1-may-2020-903679.webp)
Arxiv:2005.01804V1 [Q-Bio.QM] 1 May 2020
Modeling in the Time of COVID-19: STATISTICAL AND RULE-BASED MESOSCALE MODELS APREPRINT Ngan Nguyen1, Ondrejˇ Strnad1, Tobias Klein2,4, Deng Luo1, Ruwayda Alharbi1, Peter Wonka1, Martina Maritan3, Peter Mindek2,4, Ludovic Autin3, David S. Goodsell3, and Ivan Viola1 1King Abdullah University of Science and Technology (KAUST), Saudi Arabia. E-mails: {ngan.nquyen j ondrej.strnad j deng.luo j ruwayda.alharbi j peter.wonka j ivan.viola }@kaust.edu.sa. , N. Nguyen and O. Strnad are co-first authors. 2TU Wien, Austria. E-mails: {tklein j mindek}@cg.tuwien.ac.at. 3Scripps Research Institute, US. E-mail: {mmaritan j autin j goodsell}@scripps.edu. 4Nanographics GmbH May 6, 2020 ABSTRACT We present a new technique for rapid modeling and construction of scientifically accurate mesoscale biological models. Resulting 3D models are based on few 2D microscopy scans and the latest knowledge about the biological entity represented as a set of geometric relationships. Our new technique is based on statistical and rule-based modeling approaches that are rapid to author, fast to construct, and easy to revise. From a few 2D microscopy scans, we learn statistical properties of various structural aspects, such as the outer membrane shape, spatial properties and distribution characteristics of the macromolecular elements on the membrane. This information is utilized in 3D model construction. Once all imaging evidence is incorporated in the model, additional information can be incorporated by interactively defining rules that spatially characterize the rest of the biological entity, such as mutual interactions among macromolecules, their distances and orientations to other structures. These rules are defined through an intuitive 3D interactive visualization and modeling feedback loop. -

The Nanobank Database Is Available at for Free Use for Research Purposes
Forthcoming: Annals of Economics and Statistics (Annales d’Economie et Statistique), Issue 115/116, in press 2014 NBER WORKING PAPER SERIES COMMUNITYWIDE DATABASE DESIGNS FOR TRACKING INNOVATION IMPACT: COMETS, STARS AND NANOBANK Lynne G. Zucker Michael R. Darby Jason Fong Working Paper No. 17404 http://www.nber.org/papers/w17404 NATIONAL BUREAU OF ECONOMIC RESEARCH 1050 Massachusetts Avenue Cambridge, MA 02138 September 2011 Revised March 2014 The construction of Nanobank was supported under major grants from the National Science Foundation (SES- 0304727 and SES-0531146) and the University of California’s Industry-University Cooperative Research Program (PP9902, P00-04, P01-02, and P03-01). Additional support was received from the California NanoSystems Institute, Sun Microsystems, Inc., UCLA’s International Institute, and from the UCLA Anderson School’s Center for International Business Education and Research (CIBER) and the Harold Price Center for Entrepreneurial Studies. The COMETS database (also known as the Science and Technology Agents of Revolution or STARS database) is being constructed for public research use under major grants from the Ewing Marion Kauffman Foundation (2008- 0028 and 2008-0031) and the Science of Science and Innovation Policy (SciSIP) Program at the National Science Foundation (grants SES-0830983 and SES-1158907) with support from other agencies. Our colleague Jonathan Furner of the UCLA Department of Information Studies played a leading role in developing the methodology for selecting records for Nanobank. We are indebted to our scientific and policy advisors Roy Doumani, James R. Heath, Evelyn Hu, Carlo Montemagno, Roger Noll, and Fraser Stoddart, and to our research team, especially Amarita Natt, Hsing-Hau Chen, Robert Liu, Hongyan Ma, Emre Uyar, and Stephanie Hwang Der. -

Cancer Nanomedicine: from Targeted Delivery to Combination Therapy
Review Cancer nanomedicine: from targeted delivery to combination therapy 1,2,3 1 1 1,2 Xiaoyang Xu , William Ho , Xueqing Zhang , Nicolas Bertrand , and 1 Omid Farokhzad 1 Laboratory of Nanomedicine and Biomaterials, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115, USA 2 The David H. Koch Institute for Integrative Cancer Research, Massachusetts Institute of Technology, Cambridge, MA 02139, USA 3 Department of Chemical, Biological and Pharmaceutical Engineering, New Jersey Institute of Technology, Newark, NJ 07102, USA The advent of nanomedicine marks an unparalleled op- advantages of NPs have brought widespread attention to portunity to advance the treatment of various diseases, the field of nanomedicine, including their large ratio of including cancer. The unique properties of nanoparticles volume to surface area, modifiable external shell, biode- (NPs), such as large surface-to-volume ratio, small size, gradability, and low cytotoxicity [4]. Furthermore, nano- the ability to encapsulate various drugs, and tunable medicine brings us dramatically closer to realizing the full surface chemistry, give them many advantages over their promise of personalized medicine [5]. bulk counterparts. This includes multivalent surface mod- Engineered therapeutic NPs offer numerous clinical ification with targeting ligands, efficient navigation of the advantages. Surface modification with polyethylene glycol complex in vivo environment, increased intracellular traf- (PEG) protects NPs from clearance from the blood by the ficking, and sustained release of drug payload. These mononuclear phagocytic system (MPS), markedly increasing advantages make NPs a mode of treatment potentially both circulation times and drug uptake by target cells superior to conventional cancer therapies. This review [2,6]. -

Information in Biological Systems and the Fluctuation Theorem
Entropy 2014, 16, 1931-1948; doi:10.3390/e16041931 OPEN ACCESS entropy ISSN 1099-4300 www.mdpi.com/journal/entropy Article Information in Biological Systems and the Fluctuation Theorem Yaşar Demirel Department of Chemical and Biomolecular Engineering, University of Nebraska-Lincoln, 820 N. 16th Street, Lincoln, NE, 68588, USA; E-Mail: [email protected]; Tel.: 1-402-472 2745; Fax: 1-402 472 6989 Received: 17 January 2014; in revised form: 27 March 2014 / Accepted: 28 March 2014 / Published: 1 April 2014 Abstract: Some critical trends in information theory, its role in living systems and utilization in fluctuation theory are discussed. The mutual information of thermodynamic coupling is incorporated into the generalized fluctuation theorem by using information theory and nonequilibrium thermodynamics. Thermodynamically coupled dissipative structures in living systems are capable of degrading more energy, and processing complex information through developmental and environmental constraints. The generalized fluctuation theorem can quantify the hysteresis observed in the amount of the irreversible work in nonequilibrium regimes in the presence of information and thermodynamic coupling. Keywords: information theory; biological systems; fluctuation theorem; thermodynamic coupling 1. Introduction Definition and quantification of information have created broad discussions; particularly, “information theory” in living systems is an evolving field [1–14]. Evolution is an axiomatic consequence of organismic information obeying the second law of thermodynamics; as entropy increases, the information within a biological system becomes more complex and diversifies at bifurcation points [15–18]. Behavior of living systems is decomposable into functional modes and the ensemble of modes at an agent’s disposal constitutes functional repertoire. The modes may be subjected to operational signals and a mechanism that sequentially selects a mode so that it controls the functional dynamics [18,19]. -
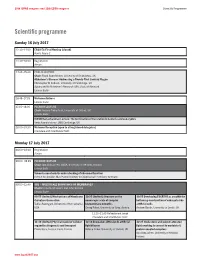
L CF IUPAB 0617 Programme-29.Indd
19th IUPAB congress and 11th EBSA congress Scientific Programme Scientific programme Sunday 16 July 2017 12:30–14:00 EBSA EC First Meeting (closed) Harris Room 1 13:30–18:00 Registration Atrium 14:30–15:30 PUBLIC LECTURE Chair: Frank Gunn-Moore, University of St Andrews, UK Alzheimer’s Disease: Addressing a Twenty-First Century Plague Christopher M Dobson, University of Cambridge, UK Sponsored by Alzheimer’s Research (UK), Scottish Network Lennox Suite 16:45–17:15 Welcome Address Lennox Suite 17:15–18:00 PLENARY LECTURE Chair: Andrew Turber field, University of Oxford, UK Lennox Suite IUPAB Ramachandran Lecture: The termination of translation in bacteria and eukaryotes Venki Ramakrishnan, LMB Cambridge, UK 18:00–19:30 Welcome Reception (open to all registered delegates) Cromdale and Strathblane Halls Monday 17 July 2017 08:00–18:00 Registration Atrium 09:00–09:45 PLENARY LECTURE Chair: Ilpo Vattulainen, EBSA, University of Helsinki, Finland Lennox Suite Towards a mechanistic understanding of ribosomal function Helmut Grubmüller, Max Planck Institute for Biophysical Chemistry, Germany 09:55–12:40 SO1 – MULTISCALE BIOPHYSICS OF MEMBRANES Chairs: Claudio M Soares and John Seddon Lennox Suite 09:55 (Invited) Mechanisms of Membrane 10:25 (Invited) Structure on the 10:55 Developing ESCRT-III as a toolkit for Curvature Generation nanoscopic scale of complex bottom-up construction of eukaryote-like Tobias Baumgart, University of Pennsylvania, biomembrane mimetics artificial cells USA Georg Pabst, University of Graz, Austria Andrew Booth, University -

New Biological Frontiers Illuminated by Molecular Sensors and Actuators JUNE 28 – JULY 1, 2015 | TAIPEI, TAIWAN
Biophysical Society Thematic Meeting | PROGRAM AND ABSTRACTS New Biological Frontiers Illuminated by Molecular Sensors and Actuators JUNE 28 – JULY 1, 2015 | TAIPEI, TAIWAN Organizing Committee Takanari Inoue, Johns Hopkins University, USA Robert E. Campbell, University of Alberta, Canada Chia-Fu Chou, Institute of Physics, Academia Sinica, Taiwan Jin-Der Wen, National Taiwan University, Taiwan New Biological Frontiers Illuminated by Molecular Sensors and Actuators Welcome Letter June 2015 Dear Colleagues, We would like to welcome you to the BPS Thematic Meeting on New Biological Frontiers Illuminated by Molecular Sensors and Actuators. This landmark international meeting brings together 25 of the leading minds in the areas of biological fluorescence imaging, biological tool development, and implementation of optogenetics, all of which are used to resolve fundamental biological questions that otherwise cannot be addressed by conventional techniques alone. We have more than 96 participants from all over the world. The goal of this meeting is to provide the attendees with a map of the new, and largely unexplored, landscape of powerful optical and chemical tools that enable researchers at the frontier to peer into and harness biological systems with a level of control that was previously unimaginable. More specifically, the recent emergence of biosensors based on fluorescent proteins, along with optogenetic and chemical dimerization techniques, have created the ability to both visualize and perturb biochemistry in live cells. In coming years we can expect complementary technologies based on magnetic- and force-based stimulation to join optical and chemical techniques as indispensable research tools for gaining novel insights into cellular biology. Due to the multidisciplinary applications of these tools, this meeting is attracting an extremely diversified audience from the fields of biotechnology, method development, chemical biology, material science, cell biology, general chemistry and engineering, computational biology, and synthetic biology. -
Self-Reporting Biological Nanosystems to Study and Control Bio-Molecular
BIOSCOPE Final Publishable Report BIOs cope Project no. NMP4-CT-2003-505211 Project acronym BIOSCOPE Project full name Self-reporting biological nanosystems to study and control bio- molecular mechanisms on the single molecule level Instrument type SPECIFIC TARGETED RESEARCH OR INNOVATION PROJECT Priority name Priority 3: Nanotechnology and nanoscience, knowledge-based multifunctional materials, new production processes and devices (NMP) Final Publishable Report Period covered: from February 1, 2006 to January 31, 2007 Date of preparation: April 19, 2007 Start date of project: Duration: February 1, 2004 36 month Project coordinator name Dr. Tommy Nylander Project coordinator organisation name Revision 2.0 Lund University (Div. Physical Chemistry 1) Page 1 of (26) BIOSCOPE Final Publishable Report BIOs cope www.BIOSCOPE.FKEM1.LU.SE Project execution The aim with BIOSCOPE was to pioneer the development of new leading edge nanoscale research tools and methodologies that will allow unprecedented insight into bio-molecular mechanisms at biological interfaces on the molecular scale. BIOSCOPE consider the biomolecular system itself as a part of the nanoscopic instrument, which in various ways reports to the out-side world about its current local state. Thereby it will be possible to study the local effects on the molecular level when e.g. a protein interacts with a biomembrane surface or when a lipase interacts with a lipid surface. The objectives of BIOSCOPE were: • To develop instrumentation and methods for manipulation of enzymes and enzyme activity at the nanoscale providing insight into the biomolecular mechanisms on a single molecule level. • To develop novel forms of integration, at the nanoscale level, of enzymes and non-biological systems such as nanoparticles, artificial membranes, electrical field or force field traps. -

Nano Brochure Copy
Nanotechnology in the San Francisco Bay Area: Dawn of a New Age Nanotechnology in the San Francisco Bay Area: Dawn of a New Age This report was produced by the Bay Area Science and Innovation Consortium (BASIC), an action-oriented collaboration of the region’s major research universities, national laboratories, independent research institutions, and research and development-driven businesses and organizations. Project Manager: Cheryl Fragiadakis, Lawrence Berkeley National Laboratory Writer: Lynn Yarris Designer: Dennis McKee With special appreciation to the following who assisted in the preparation of this report: Mark Alper, Lawrence Berkeley National Laboratory (Berkeley Lab) Yigal Blum, SRI International Grace Chou, SRI International Hans Coufal, IBM’s Almaden Research Center Nancy Garcia, Sandia National Laboratories Jonathan Goldstein, Integrated Nanosystems, Inc. Ty Jagerson, Palo Alto Research Center Tom Kalil, UC Berkeley Ted Kamins, Hewlett-Packard Dan Krotz, Berkeley Lab David Lackner, NASA Ames Research Center Dawn Levy, Stanford University Hari Manoharan, Stanford University Maya Meyyappan, NASA Ames Research Center Alexandra Navrotsky, UC Davis Anne Stark, Lawrence Livermore National Laboratory And special thanks to Mike Ross, IBM’s Almaden Research Center, and Pam Patterson, Berkeley Lab, for their editorial contributions. BASIC Bay Area Science and Innovation Consortium Advancing the Bay Area’s Leadership in Science, Technology, and Innovation Cover Cover: The next big thing in technology is going to be very very small. Nanotechnology offers the promise of manufacturing materials and products at the atomic and molecular levels, as shown by this depiction of a carbon nanotube. Economists are predicting a trillion dollar global market for nanoproducts within the next ten years. -

The Renaissance Man
NANO BIO SCIENCE: BACK TO THE RENAISSANCE MAN J. Ricardo Arias-González Madrid Institute of Advanced Studies in Nanoscience (IMDEA-Nanoscience) and National Centre of Biotechnology, CSIC. Physics and biology have been courting each other throughout the last century, and are celebrating their engagement in this century, a match arranged by Nano Bio Science. Molecular and Cell Biophysics are basically a modern conception of life sciences at the nanoscopic scale. The revolution brought about by microelectronics had a great impact in its time and its influence still surprises us today. We have not yet reached such a critical moment in nanotechnology, but from a scientific point of view, both revolutions are rooted in very different ways. Microelectronics, though highly influential in society at large, is limited to a very small part of science: the area of electronics, which does not even make up an area of knowledge in the discipline of physics. Nanotechnology, on the contrary, is expanding in such a way that it tends to involve all scientific disciplines. This is why a scientist working in nanotechnology must of necessity have wide-ranging up-to-date general knowledge; apart of course from specialist knowledge of the problems he deals with. The Renaissance man, as well as having the desire to recover all the knowledge of the classical and mediaeval world, sought to understand and interrelate it. Galileo, with his famous principle of relativity, engaged in an incredible endeavour for that time: to connect concepts in physics, the most highly developed natural science at that time. It was an age when the scientific mindset started to accept the idea of continuity in knowledge: everything must be related, even though at the moment we may not understand how. -

Nanomaterials for Bio-Medicine
NANOMATERIALS FOR BIO-MEDICINE Stefano Bellucci, PhD, Habil. Prof., First Researcher, Head of NEXT Group INSPYRE LNF 1 APRIL 2020 2 The National Institute of Nuclear Physics ( INFN - Istituto Nazionale di Fisica Nucleare) is an organization for research in nuclear physics. There are different divisions in Italy. The Frascati National Laboratories ( LNF ) is the largest and one of the most important ones. The research here is primarly concentrated on particle physics. e-mail: [email protected] Carbon nanotubes synthesis Microscopy Graphene SEM / AFM synthesis Raman/FTIR ON ° Structural & Transport Field Modelling & Emission simulation ACTIVITY360 (Bio) (Nanoco- sensors mposites NANOTECHNOLOGY Toxicology Intercon- & Drug nects delivery INTRODUCTION TO NANOPARTICLES AND THEIR USES OUTLINE Introduction Impact on health and environment Safe uses of nanotechnology Drug delivery nanosystems The science of manipulating matter at the atomic and molecular level to obtain materials with specifically enhanced chemical and physical properties. Energy Information Technology • More efficient and cost effective technologies for energy production • Smaller, faster, more energy − Solar cells − Fuel cells efficient and powerful computing − Batteries and other IT-based systems − Bio fuels Medicine Consumer Goods • Cancer treatment • Foods and beverages • Bone treatment − Advanced packaging materials, sensors, and lab- on-chips for food quality testing • Drug delivery • Appliances and textiles • Appetite control − Stain proof, water proof and wrinkle free textiles • Drug development • Household and cosmetics • Medical tools − Self-cleaning and scratch free products, paints, • Diagnostic tests and better cosmetics • Imaging THE BASICS OF NANOTECHNOLOGIES • You work at the atomic, molecular, and supramolecular levels... • The scale of lengths involved is approximately between 1 and 100 nm • The aim is the creation and use of materials, devices, systems with fundamentally innovative properties and functions, due to their very small (nanoscopic) structure.