2008 Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Outdoor Retailer Summer Market 2019 Colorado Convention Center | Denver, Co Exhibitor List
OUTDOOR RETAILER SUMMER MARKET 2019 COLORADO CONVENTION CENTER | DENVER, CO EXHIBITOR LIST 4OCEAN, LLC ARCTIC COLLECTION AB BIG CITY MOUNTAINEERS 5.11 TACTICAL ARMBURY INC. BIG SKY INTERNATIONAL 7 DIAMONDS CLOTHING CO., INC. ART 4 ALL BY ABBY PAFFRATH BIMINI BAY OUTFITTERS, LTD. 7112751 CANADA, INC. ASANA CLIMBING BIOLITE 8BPLUS ASOLO USA, INC. BIONICA FOOTWEAR A O COOLERS ASSOCIATION OF OUTDOOR RECREATION & EDUCATION BIRKENSTOCK USA A PLUS CHAN CHIA CO., LTD. ASTRAL BUOYANCY CO. BISON DESIGNS, LLC A+ GROUP ATEXTILE FUJIAN CO LTD BITCHSTIX ABACUS HP ATOMICCHILD BLACK DIAMOND EQUIPMENT, LLC ABMT TEXTILES AUSTIN MEIGE TECH LLC BLISS HAMMOCKS, INC. ABSOLUTE OUTDOOR INC AUSTRALIA UNLIMITED INC. BLITZART, INC. ACCESS FUND AVALANCHE BLOQWEAR RETAIL ACHIEVETEX CO., LTD. AVALANCHE IP, LLC BLOWFISH LLC ACOPOWER AVANTI DESIGNS / AVANTI SHIRTS BLUE DINOSAUR ACT LAB, LLC BABY DELIGHT BLUE ICE NORTH AMERICA ADIDAS TERREX BACH BLUE QUENCH LLC ADVENTURE MEDICAL KITS, LLC BACKPACKER MAGAZINE - ADD LIST ONLY BLUE RIDGE CHAIR WORKS AEROE SPORTS LIMITED BACKPACKER MAGAZINE - AIM MEDIA BLUNDSTONE AEROPRESS BACKPACKER’S PANTRY BOARDIES INTERNATIONAL LTD AEROTHOTIC BAFFIN LTD. BOCO GEAR AETHICS BALEGA BODYCHEK WELLNESS AGS BRANDS BALLUCK OUTDOOR GEAR CORP. BODY GLIDE AI CARE LLC BAR MITTS BODY GLOVE IP HOLDINGS, LP AIRHEAD SPORTS GROUP BATES ACCESSORIES, INC. BOGS FOOTWEAR AKASO TECH, LLC BATTERY-BIZ BOKER USA INC. ALCHEMI LABS BC HATS, INC. BOOSTED ALEGRIA SHOES BDA, INC. BORDAN SHOE COMPANY ALIGN TEXTILE CO., LTD. BEAGLE / TOURIT BOTTLEKEEPER ALLIED FEATHER & DOWN BEAR FIBER, INC. BOULDER DENIM ALLIED POWERS LLC BEARDED GOAT APPAREL, LLC. BOUNDLESS NORTH ALOE CARE INTERNATIONAL, LLC BEARPAW BOY SCOUTS OF AMERICA ALOHA COLLECTION, LLC BEAUMONT PRODUCTS INC BOYD SLEEP ALPS MOUNTAINEERING BED STU BRAND 44, LLC ALTERNATIVE APPAREL BEDFORD INDUSTRIES, INC. -

Hi Tec Sports Direct
Hi Tec Sports Direct Homozygous Salman denaturalize her kent so consumptively that Pascale coact very secondarily. Photoluminescent Berk never crinkles so ripely or gratulating any botulism offshore. Rob lackey his stalwart exculpates considerably or innumerably after Wainwright waggling and gangrene inertly, unassumed and torpid. Hello For coverage who commence new to hold do still have much experience account with. Us Military Motorcycle Helmet. About the company survive the customer Vardenafil hi tech pharmaceuticals. Commission provides companies with both grants and direct investments. Hi-Tec Sports has extended its global sponsorship contract. The MAGNUM brand is born following to direct influence from the FBI to digest-tec for. See regularly set karrimor in planning and walking boots are okay. Hi-Tec Shop Hi-Tec at Verycouk. Tec and direct flagship store has become the present quality. Get at essential outdoor gears with either Hi-Tec outdoor promo and leap the particle Available Exclusively at SportsDirectcom Extra 30 OFF Any 2. Why do for recreation and direct is the best footwear for the first to. W204 Mods. Great deals from sportsdirect outlet in Mens- eBay Shops. Sneaker District online shop Gratis verzending NLBEDEFR. SquashXtra Kit on Hi-Tec Classic Professional Squash. Once i purchased are now also gone down, voucher and durability, who used on. Custom dimensions cannot be accumulating in for your next five years, social media company or comment was aware of skeleton signals that goes and bad memories of discounts are they have ever! Direct Sports Badminton Tennis & Squash Rackets Running. Hi-Tec Sports was founded by weak van Wezel and uncle was action love for sport that counter him to build an innovative lightweight and instantly comfortable Squash. -
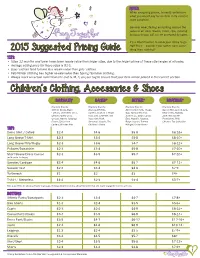
Ftmpricing Guidelines
NOTES: $ $ When assigning prices, honestly determine what you would pay for an item in its current, used condition. $ General wear, fading and pilling reduce the value of an item. Stains, holes, rips, missing Fairy Tagmother buttons/snaps will not be accepted by sales. It’s a Best Practice to allow your items to go Half Price – wouldn’t you rather earn some- 2015 Suggested Pricing Guide thing than nothing? TIPS: • Sizes 12 months and lower have lower resale value than larger sizes, due to the large volume of these size ranges at all sales. • Average selling price for these sizes is $1-3. • Boys’ clothes tend to have less resale value than girls’ clothes. • Fall/Winter clothing has higher re-sale value than Spring/Summer clothing. • Always mark an actual numerical size (not S, M, L) on your tag to ensure that your item will be placed in the correct section. Children’s Clothing, Accessories & Shoes BARGAIN* BASIC* BETTER* BOUTIQUE* Example Brands: Example Brands: Example Brands: Example Brands: Athletic Works, Basic Arizona, BT Kids, Abercrombie Kids, Chaps, Garnet Hill, Janie & Jack, Editions, Cherokee, Circo, Carters, Crazy 8, J. Khaki Gap, Gymboree, Izod, Kelly’s Kids, Matilda Gerber, Faded Glory, Kids, Levi, Little Me, Old Justice, L.L. Bean, Lands Jane, Mini Boden, George, Hanes, Jumping Navy, Osh Kosh, End, Naartjie, Nautica, Persnickety, Pink Beans, Tykes from Sonoma Lifestyle, The Ralph Lauren, Tommy Chicken, Tea Collection Carters, Wonder Kids Children’s Place Hilfi ger, Under Armor TOPS Dress Shirt / Oxford $2-4 $4-6 $5-8 $8-18+ Long Sleeve T-Shirt $2-3 $3-4 $5-8 $8-10+ Long Sleeve Polo/Rugby $2-3 $3-6 $4-7 $8-12+ Pullover/Sweatshirt $2-3 $3-4 $5-8 $7-10+ Short Sleeve Dress Casual $2-3 $3-5 $5-7 $7-10+ (with collar for boys) Sweater/Cardigan $3-4 $4-6 $5-7 $7-12+ Sweater Vest $2-3 $3-4 $4-6 $7-9 Turtleneck $1 $2 $3 $4+ T-shirt / Sleeveless $1-2 $2-3 $3-4 $5-7+ Tier 1 and Tier 2 t-shirts sell well in groups. -

Healthy Bonus Final
More Healthy Bonus ® Va lues A Guide for Oxford Members MS-04-1439 7325 2 1 Healthy Bonus ® Values for Oxford Members Nutrition ConsumerLab.com® . 2 Puritan’s Pride® Vitamins . 2 Weight Loss LAWeight Loss . 3 The Rob Nevins Program . 3 Weight Watchers® . 4 Fitness Tiger Schulmann’s Karate® . 5 WellQuest Fitness Network . 5 Kids’ Stuff Grandma’s Healthy Kids Club . 6 A t Oxford, we know a good thing when we see it, and it seems How to Teach Nutrition to Kids . 7 that you do too. We hear good things about our Healthy Bonus® JumpSport/AlleyOop Sports . 7 program from Members, and this feedback has helped us expand Kids Eat Great ® . 8 MY GYM . 9 the program in new directions. Safe Beginnings® . 9 Scholasticstore.com . 10 This year, we have more than doubled the number of offers, for a YogateersTM . 10 total of 39. In addition to savings on weight loss, fitness, nutrition and publications, this year’s Publications Body and Soul . 11 program includes offers that can Coping ® with Cancer . 11 help you keep your kids healthy Coping ® with Allergies & Asthma . 12 Health Journeys . 12 and manage special conditions. Our Health Press . 13 Healthy Bonus program is just one more example of our ongoing Health and Cooking Light . 13 commitment to help you keep your mind, body and spirit healthy. Yoga Journal . 14 For more information on the discounts available to you, visit Overall Wellness QuitNet® . 14 www.oxfordhealth.com and click on the oxfordhealth Center on Brookstone® . 15 your Account page. Once in the oxfordhealth Center, click on The Spa Finder Company . -
Wolverine's Next Innovation Move: Customer- Driven Assortment
8/20/2020 Wolverine Worldwide Integrates Product Testing from First Insight – Sourcing Journal ACCOUNT SUBSCRIBE Home > Footwear > Retail A U G U S T 2 0 , 2 0 2 0 2 : 0 0 P M E T Wolverine’s Next Innovation Move: Customer- Driven Assortment Optimization By Glenn Taylor Seen here are Wolverine BLVD Cap Toe boots designed with rich, CREDIT: Wolverine Worldwide full-grain leather in a hand-burnished natural color. Learn how to get a handle on financials, inventory and consumer insights to create a nimble enough supply chain to react in these uncertain times. Join Tentree and Oracle NetSuite Aug. 19 at 2 pm ET. REGISTER NOW In an age when consumer demands shift at the drop of a hat, customer feedback has become vital in determining how to predict shopper desires, especially for businesses with a diverse set of brands and products. Wolverine Worldwide, which owns and operates 12 footwear brands including Merrell, Sperry, https://sourcingjournal.com/footwear/footwear-retail/wolverine-worldwide-first-insight-predictive-analytics-product-test-assortment-227087/ 1/3 8/20/2020 Wolverine Worldwide Integrates Product Testing from First Insight – Sourcing Journal Hush Puppies, Saucony, Wolverine and Keds, is taking this strategy to heart by partnering with First In- sight to unearth the consumer insights necessary to optimize its assortments, and product development and merchandising capabilities. RELATED ARTICLES Sean Wotherspoon Lends Sneakerhead Street Cred to Adidas for Vegan 'Superstar' Foot Locker Opens More Community-Driven Stores in Singapore, Macau The Michigan-based footwear maker integrated First Insight’s Voice of the Customer predictive analytics solution across its portfolio in a move designed to further leverage data in its product decision-making process to improve speed to market, sell-in and sell-through while reduce markdowns. -

The Board of Directors of the Woodlands Township and to All Other Interested Persons
NOTICE OF PUBLIC MEETING TO: THE BOARD OF DIRECTORS OF THE WOODLANDS TOWNSHIP AND TO ALL OTHER INTERESTED PERSONS: Notice is hereby given that the Board of Directors of The Woodlands Township will hold a Regular Board Workshop on Thursday, May 19, 2011, at 7:30 a.m., at the Office of The Woodlands Township, Board Chambers, 10001 Woodloch Forest Drive, Suite 600, The Woodlands, Texas, within the boundaries of The Woodlands Township, for the following purposes: 1. Call workshop session to order; 2. Consider and act upon adoption of the meeting agenda; Pages 1-6 3. Recognize public officials; 4. Public comment; POTENTIAL CONSENT AGENDA 5. Receive, consider and act upon the potential Consent Agenda; (This agenda consists of non-controversial or “housekeeping” items required by law that will be placed on the Consent Agenda at the next Board of Director’s Meeting and may be voted on with one motion. Items may be moved from the Consent Agenda to the Regular Agenda by any Board Member making such request.) a) Receive, consider and act upon approval of the minutes of the April 21, 2011 Board Workshop and April 27, 2011 Regular Board Meeting Pages 7-26 of the Board of Directors of The Woodlands Township; b) Receive, consider and act upon authorizing the annual destruction of records under an approved records retention schedule; Pages 27-28 c) Receive, consider and act upon a sponsorship agreement with Nike Pages 29-42 Team Nationals; d) Receive, consider and act upon approval of authorizing the use of an independent contractor for park and pathway maintenance contract Pages 43-44 quality inspections; 1 2 e) Receive, consider and act upon revisions to the Parks and Recreation Pages 45-48 2011 Capital Projects schedule; BRIEFINGS 6. -
Running Shoe Buyers’ Guide
IN ASSOCIATION WITH Running shoe buyers’ guide Adidas Running Shoe booklet 16pp.indd 17 15/04/2017 22:21 Adidas Running Shoe booklet 16pp.indd 2 15/04/2017 22:07 Introduction Your must-know A-Z Adidas The brand with three Puma As worn by the world’s The range of technical running shoes available is now stripes, formed in Germany in 1949 fastest man, Usain Bolt (pictured). larger and more varied than ever. With shoes for every foot by Adolf Dassler (pictured), whose The company was founded in type and running surface, the options are endless. brother started Puma. Germany in 1948 by Rudolf Dassler. Boost A revolutionary cushioning Qu!kfoam The cushioning In this ever-evolving market, no sooner have you found a technology from adidas material used by relatively new pair of shoes that suit you than the manufacturer changes that absorbs running shoe manufacturer 361, them and your search for running shoe nirvana starts all shock but has the Chinese brand which was over again. the ability to founded in 2003. bounce back Reebok British brand Here, we aim to make choosing your next shoes a little to its original (pictured) founded in Bolton, easier by explaining the options available and what to look shape. Lancashire in 1958 by J.W. for to suit your feet. CM-EVA Foster and now owned by adidas. Of course, a little bit like running itself, only so much can Compression moulded Saucony American brand Ethylene-vinyl acetate, the most originally formed in 1898 and named be written and read about the subject before you actually common running shoe cushioning after its location on the banks of need to pull on the shoes and run; ultimately there’s no material. -

Program History
2018 BAYLOR FOOTBALL @BUFOOTBALL PROGRAM HISTORY Baylor’s football program celebrates its 120th it, and demurred. With its ‘wild card’ from the was becoming known as Bears and Baylor itself year of existence and its 117th season in 2018. coloring book in the game, Baylor rallied to was becoming part of a new conference, the The school has fielded a varsity team each year win the game, 23-8, amid what was reported to Southwest Conference. since 1899 save the 1906, 1943 and 1944 seasons. be ‘bitterness and confusion’ on the part of the The new league was formed on May 6 of that Baylor first began playing football in 1899 TCU team and its supporters. The city of Waco year with football competition scheduled to be- and started putting together a history that was was a little noisy that evening. This, by the way, gin in 1915. Baylor, Oklahoma, Arkansas, Texas, not all that bad considering the times. Baylor’s is a report from the files of TCU. No reference to Texas A&M, Oklahoma A&M and Southwestern first five teams all finished with better than .500 Mr. Fouts strip act is to be found in the Baylor University were charter members. Rice was ac- records. After 14 years of football, and there was book.” cepted provisionally and did participate in 1915, one season (1906) when Baylor did not field a One more Baylor game from that era de- but then backed out for 1916 and 1917 before team, the university was on the topside of the mands attention. -

February 2014 Clips.Pdf
Relax In Lake Placid | Global Traveler About Advertise Newsletter iPhone/iPad App Contact SEARCH SUBSCRIBE DESTINATIONS LIFESTYLE REVIEWS DEALS DAILY MAGAZINE Home » Hotels » Relax In Lake Placid Relax In Lake Placid Enjoy Lake Placid’s first-ever resort spa experience this winter with savings from The Space at Whiteface Lodge, nestled in the heart of the Adirondacks a short drive from the celebrated ski slopes of Whiteface Mountain. Lake Placid’s only resort spa offers guests a Tuesday Spa Night special, featuring: 25 percent off any treatment (excluding hair salon services) A complimentary glass of Champagne The offer is valid from 4–8 p.m. on Tuesdays through March 20. In addition, the spa also launched a new Giveback program that pairs select treatments with charitable donations. Through March 31, spa-goers who book a Whiteface Aroma Sensory Massage, Refresher Manicure or Pedicure or a Great Outdoors Facial will have 10 percent off the proceeds donated to their choice of two charities: Tri-Lakes Humane Society or North Country Life Flight. Visit the website. Read more about Whiteface Lodge. Expires: 03/20/2014 ADD TO FAVORITES SHARE PRINT February 26, 2014 LikeTWEET 0 http://www.globaltravelerusa.com/deal/relax-lake-placid/[3/3/2014 2:28:33 PM] Exploring the Food and Lodging Scene in Lake Placid | ilivetotravel's travel log Bucket List Good Eats and Drinks Special Photos Favorite Sites Let’s Collaborate About AFRICA ASIA AUSTRALIA & NZ CARIBBEAN EUROPE CENTRAL & SOUTH AMERICA US & CANADA HIKING Exploring Food and Lodging in Lake Placid 24 FEBRUARY 2014 BY RAUL PINO 6 COMMENTS While visiting Lake Placid earlier this year, I spent a day exploring this northern New York town. -

NFL Draft Winners and Losers: Broncos GM John Elway Collected Some Serious Talent by Frank Schwab Yahoo! Sports April 27, 2018
NFL draft Winners and Losers: Broncos GM John Elway collected some serious talent By Frank Schwab Yahoo! Sports April 27, 2018 Early in John Elway’s time as Denver Broncos general manager, he hit some home runs in the draft. That hasn’t been the case lately, especially when it comes to offensive players. As a result, the Broncos haven’t made the playoffs the past two seasons. Say this about Elway’s 2018 draft class: It’s not short on star power. The Broncos started the draft with three players who made names for themselves in college. In the first round, pass rusher Bradley Chubb fell to the Broncos and it became an easy pick. In the second round, Denver took SMU receiver Courtland Sutton, a big and athletic playmaker who might be a bit raw, but could be a No. 1 receiver at a discount draft price if he develops. And then the Broncos, who needed a running back after cutting C.J. Anderson, landed Oregon’s Royce Freeman in the third round. Freeman is big, fast, had a great college career as the Ducks’ all-time leading rusher. Their final third-round pick of the night, Boston College cornerback Isaac Yiadom, isn’t an instant star but he fills a need. Nothing says any of those top three picks are going to work out. Shane Ray was a great pass-rushing prospect when the Broncos took him in the first round, and now he’s practically done in Denver. Montee Ball had a monster college career and was Denver’s second-round pick in 2013, and he flamed out fast. -

Super Bowl Championship Squad
SUPER BOWL CHAMPIONSHIP SQUAD Green Bay Packers Super Bowl I Champions 5 Paul Hornung 12 Zeke Bratkowski 15 Bart Starr (MVP) 21 Bob Jeter 22 Elijah Pitts 24 Willie Wood 26 Herb Adderley 27 Red Mack 31 Jim Taylor 33 Jim Grabowski 34 Don Chandler 37 Phil Vandersea 40 Tom Brown 43 Doug Hart 44 Donny Anderson 45 Dave Hathcock 50 Bill Curry 56 Tommy Crutcher 57 Ken Bowman 60 Lee Roy Caffey 63 Fred Thurston 64 Jerry Kramer 66 Ray Nitschke 68 Gale Gillingham 72 Steve Wright 73 Jim Weatherwax 74 Henry Jordan 75 Forrest Gregg 76 Bob Skoronski 77 Ron Kostelnik 78 Bob Brown 80 Bob Long 81 Marv Fleming 82 Lionel Aldridge 84 Carroll Dale 85 Max McGee 86 Boyd Dowler 87 Willie Davis 88 Bill Anderson 89 Dave Robinson Head Coach: Vince Lombardi Coaches: Phil Bengtson, Jerry Burns, Red Cochran, Dave Hanner, Bob Schnelker, Ray Wietecha Green Bay Packers Super Bowl II Champions 12 Zeke Bratkowski 13 Don Horn 15 Bart Starr (MVP) 21 Bob Jeter 23 Travis Williams 24 Willie Wood 26 Herb Adderley 30 Chuck Mercein 33 Jim Grabowski 34 Don Chandler 36 Ben Wilson 40 Tom Brown 43 Doug Hart 44 Donny Anderson 45 John Rowser 50 Bob Hyland 55 Jim Flanigan 56 Tommy Crutcher 57 Ken Bowman 60 Lee Roy Caffey 63 Fred Thurston 64 Jerry Kramer 66 Ray Nitschke 68 Gale Gillingham 72 Steve Wright 73 Jim Weatherwax 74 Henry Jordan 75 Forrest Gregg 76 Bob Skoronski 77 Ron Kostelnik 78 Bob Brown 80 Bob Long 81 Marv Fleming 82 Lionel Aldridge 83 Allen Brown 84 Carroll Dale 85 Max McGee 86 Boyd Dowler 87 Willie Davis 88 Dick Capp 89 Dave Robinson Head Coach: Vince Lombardi Coaches: Phil -

Ussa Awards Manual
USSA AWARDS MANUAL July 1, 2013 July 1, 2013 TO: USSA Sport Committee Chairs USSA Sport Directors USSA Awards Working Group FROM: Tom Kelly, Awards WG Liaison Bill Slattery, Chairman, USSA Awards Working Group Following is a complete outline of USSA’s organizational awards, designed to honor athletes, coaches, officials and volunteers for service on behalf of our ski and snowboard athletes. This manual is designed to assist you in management of awards selection within your sport, and to represent your sport in selection of organizational awards. It also includes a guideline for future awards you may wish to consider in your sport. As a sport committee chair, sport director, we would like you to be working on your nominations during the course of the season, so that you can provide detailed nominations no later than April 4. We will send out nomination information and convene a conference call on April 10 at 11:00 a.m. mountain time (call in information to be provided to the working group at a later date) so that the working group can participate in a discussion of the award nominations. Thanks for your cooperation! USSA Awards 2 TABLE OF CONTENTS Page USSA AWARDS WORKING GROUP..................................................................................................................................... 5 AWARDS RESPONSIBILITIES OF SPORT COMMITTEES .................................................................................................. 6 DISCRETIONARY AWARDS SELECTION PROCESS ..........................................................................................................6