MURDOCH RESEARCH REPOSITORY This Is the Author's
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

TRP Mediation
molecules Review Remedia Sternutatoria over the Centuries: TRP Mediation Lujain Aloum 1 , Eman Alefishat 1,2,3 , Janah Shaya 4 and Georg A. Petroianu 1,* 1 Department of Pharmacology, College of Medicine and Health Sciences, Khalifa University of Science and Technology, Abu Dhabi 127788, United Arab Emirates; [email protected] (L.A.); Eman.alefi[email protected] (E.A.) 2 Center for Biotechnology, Khalifa University of Science and Technology, Abu Dhabi 127788, United Arab Emirates 3 Department of Biopharmaceutics and Clinical Pharmacy, Faculty of Pharmacy, The University of Jordan, Amman 11941, Jordan 4 Pre-Medicine Bridge Program, College of Medicine and Health Sciences, Khalifa University of Science and Technology, Abu Dhabi 127788, United Arab Emirates; [email protected] * Correspondence: [email protected]; Tel.: +971-50-413-4525 Abstract: Sneezing (sternutatio) is a poorly understood polysynaptic physiologic reflex phenomenon. Sneezing has exerted a strange fascination on humans throughout history, and induced sneezing was widely used by physicians for therapeutic purposes, on the assumption that sneezing eliminates noxious factors from the body, mainly from the head. The present contribution examines the various mixtures used for inducing sneezes (remedia sternutatoria) over the centuries. The majority of the constituents of the sneeze-inducing remedies are modulators of transient receptor potential (TRP) channels. The TRP channel superfamily consists of large heterogeneous groups of channels that play numerous physiological roles such as thermosensation, chemosensation, osmosensation and mechanosensation. Sneezing is associated with the activation of the wasabi receptor, (TRPA1), typical ligand is allyl isothiocyanate and the hot chili pepper receptor, (TRPV1), typical agonist is capsaicin, in the vagal sensory nerve terminals, activated by noxious stimulants. -

102 the Effects of Intravesical
102 Harper M, Brady C. M, Scaravilli F, Fowler C. J. Institute of Neurology, London THE EFFECTS OF INTRAVESICAL RESINIFERATOXIN ON SUBUROTHELIAL NERVE DENSITY IN PATIENTS WITH NEUROGENIC DETRUSOR OVERACTIVITY Aims of Study Somatic and autonomic neural pathways integrated in the CNS regulate urine storage and voiding. When spinal cord lesions disrupt these pathways, an aberrant segmental sacral reflex emerges, the afferent limb of which is comprised of small unmyelinated C-fibres that originate in the suburothelium. This pathological reflex is thought to be the underlying cause of “spinal” neurogenic detrusor overactivity (NDO). We are currently evaluating the role of resiniferatoxin (RTX) in the treatment of refractory “spinal” NDO. RTX is an ultra-potent capsaicin analogue purified from the dried latex of the succulent plant Euphorbia Resinifera. The vanillyl group of RTX facilitates the action of the vanilloid receptor (VR-1), a non-selective cation channel expressed on suburothelial C-fibres. Intravesical therapy with a single dose of RTX results in early acute excitatory effects (“sensitisation”) followed by inhibition of neuropeptide release and neuronal terminal field degeneration (“desensitisation”) (Avelino et al., 2001). In patients with refractory NDO, it has been shown that intravesical therapy with vanilloid compounds such as RTX or capsaicin significantly decreases lower urinary tract symptoms for a period of weeks or months, depending on factors such as dose and disease progression. It is thought that the eventual recurrence of symptoms is related to C-fibre regeneration. We have previously shown that the mean suburothelial nerve density decreases in patients who respond to capsaicin. Our experimental aim is to measure suburothelial nerve density in flexible cystoscopic biopsies in controls and patients with NDO before and after intravesical RTX or placebo. -

TRP CHANNELS AS THERAPEUTIC TARGETS TRP CHANNELS AS THERAPEUTIC TARGETS from Basic Science to Clinical Use
TRP CHANNELS AS THERAPEUTIC TARGETS TRP CHANNELS AS THERAPEUTIC TARGETS From Basic Science to Clinical Use Edited by ARPAD SZALLASI MD, PHD Department of Pathology, Monmouth Medical Center, Long Branch, NJ, USA AMSTERDAM • BOSTON • HEIDELBERG • LONDON NEW YORK • OXFORD • PARIS • SAN DIEGO SAN FRANCISCO • SINGAPORE • SYDNEY • TOKYO Academic Press is an imprint of Elsevier Academic Press is an imprint of Elsevier 125 London Wall, London, EC2Y 5AS, UK 525 B Street, Suite 1800, San Diego, CA 92101-4495, USA 225 Wyman Street, Waltham, MA 02451, USA The Boulevard, Langford Lane, Kidlington, Oxford OX5 1GB, UK First published 2015 Copyright © 2015 Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangement with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). Notices Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. -

The Role of Phytotoxic and Antimicrobial Compounds of Euphorbia Gummifera in the Cause and Maintenance of the Fairy Circles of Namibia
The role of phytotoxic and antimicrobial compounds of Euphorbia gummifera in the cause and maintenance of the fairy circles of Namibia by Nicole Galt Submitted in partial fulfillment of the requirements for the degree Magister Scientiae Department of Plant and Soil Sciences Faculty of Natural and Agricultural Sciences University of Pretoria Pretoria Supervisor: Prof. J.J.M. Meyer March 2018 i The role of phytotoxic and antimicrobial compounds of Euphorbia gummifera in the cause and maintenance of the fairy circles of Namibia by Nicole Galt Department of Plant and Soil Sciences Faculty of Natural and Agricultural Sciences University of Pretoria Pretoria Supervisor: Prof. J.J.M. Meyer Degree: MSc Medicinal Plant Science Abstract Fairy circles (FC) are unexplained botanical phenomena of the pro-Namib desert and parts of the West Coast of South Africa. They are defined as circular to oval shaped anomalies of varying sizes that are left bereft of vegetation. Even though there are several distinctly different hypotheses that have aimed to explain the origin of fairy circles, none have done so to satisfaction of the scientific community. The aim of this study was to determine if phytotoxic and antibacterial properties of a co-occurring Euphorbia species, E. gummifera plays a role in the creation of fairy circles. Representative soil samples (from inside-, outside fairy circles and underneath dead E. gummifera plants) and plant samples (aerial ii parts of E. gummifera and intact grasses, Stipagrostis uniplumis) were collected from the area. The collected samples were used for a several biological assays. A soil bed bio-assay was done using the three collected soil types. -

TRPV1 and Endocannabinoids: Emerging Molecular Signals That Modulate Mammalian Vision
Cells 2014, 3, 914-938; doi:10.3390/cells3030914 OPEN ACCESS cells ISSN 2073-4409 www.mdpi.com/journal/cells Review TRPV1 and Endocannabinoids: Emerging Molecular Signals that Modulate Mammalian Vision 1,2,†, 1,2,† 1,† 1,2,3,4, Daniel A. Ryskamp *, Sarah Redmon , Andrew O. Jo and David Križaj * 1 Department of Ophthalmology & Visual Sciences, Moran Eye Institute, University of Utah School of Medicine, Salt Lake City, UT 84132, USA; E-Mails: [email protected] (S.R.); [email protected] (A.O.J.) 2 Interdepartmental Program in Neuroscience, University of Utah School of Medicine, Salt Lake City, UT 84132, USA 3 Department of Neurobiology & Anatomy, University of Utah School of Medicine, Salt Lake City, UT 84132, USA 4 Center for Translational Medicine, University of Utah School of Medicine, Salt Lake City, UT 84132, USA † Those authors contributed equally to this work. * Authors to whom correspondence should be addressed; E-Mails: [email protected] (D.A.R.); [email protected] (D.K.); Tel.: +1-801-213-2777 (D.K.); Fax: +1-801-587-8314 (D.K.). Received: 1 July 2014; in revised form: 27 August 2014 / Accepted: 5 September 2014 / Published: 12 September 2014 Abstract: Transient Receptor Potential Vanilloid 1 (TRPV1) subunits form a polymodal cation channel responsive to capsaicin, heat, acidity and endogenous metabolites of polyunsaturated fatty acids. While originally reported to serve as a pain and heat detector in the peripheral nervous system, TRPV1 has been implicated in the modulation of blood flow and osmoregulation but also neurotransmission, postsynaptic neuronal excitability and synaptic plasticity within the central nervous system. -

Osher Mini Medical School Feb 10 2016 Schumacher HAND OUT.Pptx
2/10/16! Back to the Future of Pain Medicine ! What is Pain?! ! Pain: “An unpleasant sensory and emotional Mark Schumacher Ph.D.,M.D.! experience associated with actual or potential Professor and Chief, Division of Pain Medicine! tissue damage, or described in terms of such Dept. of Anesthesia & Perioperative Care! damage (IASP).”! Medical Director, UCSF Pain Services! University of California, San Francisco! Plant derivatives imitate endogenous Have we made any progress in the analgesic systems pharmacologic treatment of pain?! ! Morphine! " 1805 - Primary therapy for severe pain is:! " Morphine! ! Endorphin! " 2016 - Primary therapy for severe pain is:! " Morphine! •" Sustained Release! Ideal analgesic ?! A revolution is underway in our understanding of the pain pathway! Acts selectively on the “pain-sensing” nerves! Does not depress CNS - respiration! .. and its origin began thousands of Use over time maintains analgesia! years ago with the physicians of ancient times! Easy to administer! Is not addictive! Affordable $$! ! 1! 2/10/16! # Anti-Atlas Mountains-Morocco! Capsaicin vs. Resiniferatoxin (RTX)! ! ! ! ! # Euphorbia Resinifera! Share a Common Modification ! Perception! Peppers Sail the Ocean Blue! Transmission! 2000 BC 63 BC 1428 1492 Euphobia Resinifera Transduction! Descartes 1644 ! Sherrington and the development ! of modern neurobiology - nociceptor! Primary Afferent Nociceptors! Sherrington (1906) ... Proposed: the experience of pain is based on nerves that responded to specific 2000 BC 63 BC 1428 1492 1906 noxious stimuli -

THE VANILLOID RECEPTOR: a Molecular Gateway to the Pain
P1: FMF December 11, 2000 14:7 Annual Reviews AR121-17 Annu. Rev. Neurosci. 2001. 24:487–517 Copyright c 2001 by Annual Reviews. All rights reserved THE VANILLOID RECEPTOR:AMolecular Gateway to the Pain Pathway Michael J Caterina1 and David Julius2 1Department of Biological Chemistry, Johns Hopkins University School of Medicine, Baltimore, Maryland 21205; e-mail: [email protected] 2Department of Cellular and Molecular Pharmacology, University of California at San Francisco, San Francisco, California 94143; e mail: [email protected] Key Words capsaicin, pain, nociceptor, ion channel, heat sensation, hyperalgesia ■ Abstract The detection of painful stimuli occurs primarily at the peripheral termi- nals of specialized sensory neurons called nociceptors. These small-diameter neurons transduce signals of a chemical, mechanical, or thermal nature into action potentials and transmit this information to the central nervous system, ultimately eliciting a perception of pain or discomfort. Little is known about the proteins that detect nox- ious stimuli, especially those of a physical nature. Here we review recent advances in the molecular characterization of the capsaicin (vanilloid) receptor, an excitatory ion channel expressed by nociceptors, which contributes to the detection and integration of pain-producing chemical and thermal stimuli. The analysis of vanilloid receptor gene knockout mice confirms the involvement of this channel in pain sensation, as well as in hypersensitivity to noxious stimuli following tissue injury. At the same time, these studies demonstrate the existence of redundant mechanisms for the sensation of heat-evoked pain. by SCELC Trial on 10/04/10. For personal use only. INTRODUCTION Annu. Rev. Neurosci. 2001.24:487-517. -

Homeopathic Remedies
HOMEOPATHIC REMEDIES ABIES CANADENSIS ABIES NIGRA ABROTANUM ABSINTHIUM ACALYPHA INDICA ACANTHIA LECTULARIUS ACARUS ACETANILIDE ACHYRANTHES ACIDUM ACETICUM ACIDUM BENZOICUM ACIDUM BORICUM ACIDUM BUTYRICUM ACIDUM CAMPHORICUM ACIDUM CARBOLICUM ACIDUM CHROMICUM ACIDUM CHRYSOPHANICUM ACIDUM CITRICUM ACIDUM TANNICUM ACIDUM FLOURICUM ACIDUM FORMICUM ACIDUM GALLICUM ACIDUM HIPPURICUM ACIDUM HYDROBROMICUM ACIDUM HYDROCYANICUM ACIDUM LACTICUM ACIDUM MURIATICUM ACIDUM NITRICUM ACIDUM NITRO-HYDROCHLORICUM ACIDUM NITRO-MURIATICUM ACIDUM OXALICUM ACIDUM PHOSPHORICUM ACIDUM PICRICUM ACIDUM SALICYLICUM ACIDUM SARCOLACTICUM ACIDUM SUCCINICUM ACIDUM SULPHURICUM ACIDUM SULFUROSUM ACIDUM TARTARICUM ACIDUM URICUM ACONITINE 3 ACONITUM CAMMARUM ACONITUM FEROX ACONITUM LYCOTONUM ACONITUM NAPELLUS ACTAEA RACEMOSA ACTAEA SPICATA ADEPS SUIS ADONIDINE ADONIS VERNALIS ADRENALINE AESCULUS GLABRA AESCULUS HYPOCASTANUM AETHER NITRE SPIRITUS AETHIOPS ANTIMONIALIS AETHIOPS MERCURIUS MINERALIS AETHUSA CYNAPIUM AGARICIN AGARICUS EMETICUS AGARICUS MUSCARIUS AGARICUS PHALLOID AGAVE AMERICANA AGNUS CASTUS AGRAPHIS NUTANS AGRIMONIA EUPATORIA AGROPYRON REPENS AGROSTEMA GITHAGO AILANTHUS GLANDULOSA ALCOHOL SULPHURIS ALETRIS FARINOSA ALFALFA ALKEKENGI OFFICINARUM ALLIUM CEPA ALLIUM SATIVUM ALNUS RUBRA ALOE SOCOTRINA ALSTONIA CONSTRICTA ALSTONIA SCHOLARIS ALTHAE OFFICINALIS ALUMEN ALUMINA ALUMINIUM ACETICUM ALUMINIUM CHLORIDE ALUMINIUM SILICATUM ALUMINIUM SILICO SULPHOCALCATE AMANITA MUSCARIUS 4 AMANITA PHALLOIDES AMANITA PHALLOIDES ALBA AMANITA VERNUS AMBER SUCCINUM AMBRA GRISEA -

PC18 Inf. 6 (English Only / Únicamente En Inglés / Seulement En Anglais)
PC18 Inf. 6 (English only / Únicamente en inglés / Seulement en anglais) CONVENTION ON INTERNATIONAL TRADE IN ENDANGERED SPECIES OF WILD FAUNA AND FLORA ____________ Eighteenth meeting of the Plants Committee Buenos Aires (Argentina), 17-21 March 2009 TRADE SURVEY STUDY ON SUCCULENT EUPHORBIA SPECIES PROTECTED BY CITES AND USED AS COSMETIC, FOOD AND MEDICINE, WITH SPECIAL FOCUS ON CANDELILLA WAX The attached document has been submitted by the Scientific Authority of Germany*. * The geographical designations employed in this document do not imply the expression of any opinion whatsoever on the part of the CITES Secretariat or the United Nations Environment Programme concerning the legal status of any country, territory, or area, or concerning the delimitation of its frontiers or boundaries. The responsibility for the contents of the document rests exclusively with its author. PC18 Inf. 6 – p. 1 Trade survey study on succulent Euphorbia species protected by CITES and used as cosmetic, food and medicine, with special focus on Candelilla wax Dr. Ernst Schneider PhytoConsulting, D-84163 Marklkofen Commissioned by Bundesamt für Naturschutz CITES Scientific Authority, Germany February 2009 Content SUMMARY ................................................................................................................. 4 OBJECTIVE................................................................................................................ 5 CANDELILLA WAX, ITS USE AND THE PLANT SOURCE ....................................... 6 Candelilla wax -

Further Terpenoids from Euphorbia Tirucalli
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Archive Ouverte en Sciences de l'Information et de la Communication Further terpenoids from Euphorbia tirucalli Thuc-Huy Duong, Mehdi A Beniddir, Grégory Genta-Jouve, Huu-Hung Nguyen, Dinh-Phuoc Nguyen, Thi-Anh-Tuyet Nguyen, Dinh-Hung Mac, Joël Boustie, Kim-Phi-Phung Nguyen, Warinthorn Chavasiri, et al. To cite this version: Thuc-Huy Duong, Mehdi A Beniddir, Grégory Genta-Jouve, Huu-Hung Nguyen, Dinh-Phuoc Nguyen, et al.. Further terpenoids from Euphorbia tirucalli. Fitoterapia, Elsevier, 2019, 135, pp.44-51. 10.1016/j.fitote.2019.04.001. hal-02120745 HAL Id: hal-02120745 https://hal-univ-rennes1.archives-ouvertes.fr/hal-02120745 Submitted on 21 Jun 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. ACCEPTED MANUSCRIPT Further Terpenoids from Euphorbia tirucalli Thuc-Huy Duong,a,b Mehdi A. Beniddir,c Grégory Genta-Jouve,d Huu-Hung Nguyen,e Dinh-Phuoc Nguyen,f Thi-Anh-Tuyet Nguyen,g Dinh-Hung Mac,h Joël Boustie,i Kim-Phi-Phung Nguyen,j Warinthorn Chavasiri,f*and Pierre Le Pogamc* aDepartment for Management of Science and Technology Development, Ton Duc Thang University, Ho Chi Minh City, Vietnam bFaculty of Applied Sciences, Ton Duc Thang University, Ho Chi Minh City, Vietnam cBioCIS, Université Paris-Sud, CNRS, Université Paris-Saclay, 5 Rue J.-B. -

TRPV Channels and Their Pharmacological Modulation
Cellular Physiology Cell Physiol Biochem 2021;55(S3):108-130 DOI: 10.33594/00000035810.33594/000000358 © 2021 The Author(s).© 2021 Published The Author(s) by and Biochemistry Published online: online: 28 28 May May 2021 2021 Cell Physiol BiochemPublished Press GmbH&Co. by Cell Physiol KG Biochem 108 Press GmbH&Co. KG, Duesseldorf SeebohmAccepted: 17et al.:May Molecular 2021 Pharmacology of TRPV Channelswww.cellphysiolbiochem.com This article is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 Interna- tional License (CC BY-NC-ND). Usage and distribution for commercial purposes as well as any distribution of modified material requires written permission. Review Beyond Hot and Spicy: TRPV Channels and their Pharmacological Modulation Guiscard Seebohma Julian A. Schreibera,b aInstitute for Genetics of Heart Diseases (IfGH), Department of Cardiovascular Medicine, University Hospital Münster, Münster, Germany, bInstitut für Pharmazeutische und Medizinische Chemie, Westfälische Wilhelms-Universität Münster, Münster, Germany Key Words TRPV • Molecular pharmacology • Capsaicin • Ion channel modulation • Medicinal chemistry Abstract Transient receptor potential vanilloid (TRPV) channels are part of the TRP channel superfamily and named after the first identified member TRPV1, that is sensitive to the vanillylamide capsaicin. Their overall structure is similar to the structure of voltage gated potassium channels (Kv) built up as homotetramers from subunits with six transmembrane helices (S1-S6). Six TRPV channel subtypes (TRPV1-6) are known, that can be subdivided into the thermoTRPV 2+ (TRPV1-4) and the Ca -selective TRPV channels (TRPV5, TRPV6). Contrary to Kv channels, TRPV channels are not primary voltage gated. All six channels have distinct properties and react to several endogenous ligands as well as different gating stimuli such as heat, pH, mechanical stress, or osmotic changes. -
Resiniferatoxin CSPR GHS Format 2014
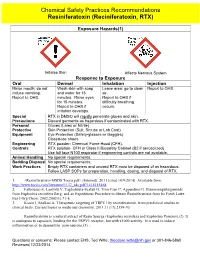
Chemical Safety Practices Recommendations Resiniferatoxin (Reciniferatoxin, RTX) Exposure Hazards(1) Irritates Skin Affects Nervous System Response to Exposure Oral Dermal Inhalation Injection Rinse mouth; do not Wash skin with soap Leave area; go to clean Report to OHS. induce vomiting. and water for 15 air. Report to OHS. minutes. Rinse eyes Report to OHS if for 15 minutes. difficulty breathing Report to OHS if occurs. irritation develops. Special RTX in DMSO will rapidly penetrate gloves and skin. Precautions Discard garments as hazardous if contaminated with RTX. Personal Gloves (Latex or Nitrile) Protective Skin Protection (Suit, Scrubs or Lab Coat) Equipment Eye Protection (Safety-glasses or Goggles) Closed-toe shoes Engineering RTX powder- Chemical Fume Hood (CFH). Controls RTX solution- CFH or Class II Biosafety Cabinet (B2 if aerosolized) Use full face N100 respirator if engineering controls are not available. Animal Handling No special requirements. Bedding Disposal No special requirements. Work Practices Empty RTX containers and unused RTX must be disposed of as hazardous. Follow LASP SOPs for preparation, handling, dosing, and disposal of RTX. 1. <Resiniferatoxin MSDS Tocris.pdf> [Internet]. 2011 [cited 10/9/2014]. Available from: http://www.tocris.com/literature/1137_sds.pdf?1414155468. 2. Fattorusso E, Lanzotti V, Taglialatela-Scafati O, Tron Gian C, Appendino G. Bisnorsesquiterpenoids from Euphorbia resinifera Berg. and an Expeditious Procedure to Obtain Resiniferatoxin from Its Fresh Latex. Eur J Org Chem. 2002;2002(1):71-8. 3. Kissin I, Szallasi A. Therapeutic targeting of TRPV1 by resiniferatoxin, from preclinical studies to clinical trials. Current topics in medicinal chemistry. 2011;11(17):2159-70.