Srhr and Hiv Linkages Indicator Baseline Survey Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
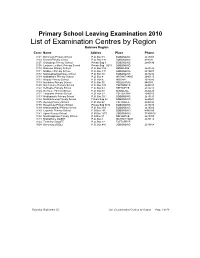
List of Examination Centres by Region Bobirwa Region Centr Name Addres Place Phone 0101 Bobonong Primary School P.O
Primary School Leaving Examination 2010 List of Examination Centres by Region Bobirwa Region Centr Name Addres Place Phone 0101 Bobonong Primary School P.O. Box 48 BOBONONG 2619207 0103 Borotsi Primary School P.O. Box 136 BOBONONG 819208 0107 Gobojango Primary School Private Bag 8 BOBONONG 2645436 0108 Lentswe-Le-Moriti Primary School Private Bag 0019 BOBONONG 0110 Mabolwe Primary School P.O. Box 182 SEMOLALE 2645422 0111 Madikwe Primary School P.O. Box 131 BOBONONG 2619221 0112 Mafetsakgang primary school P.O. Box 46 BOBONONG 2619232 0114 Mathathane Primary School P.O. Box 4 MATHATHANE 2645110 0117 Mogapi Primary School P.O. Box 6 MOGAPI 2618545 0119 Molalatau Primary School P.O. Box 50 MOLALATAU 845374 0120 Moletemane Primary School P.O. Box 176 TSETSEBYE 2646035 0123 Sefhophe Primary School P.O. Box 41 SEFHOPHE 2618210 0124 Semolale Primary School P.O. Box 10 SEMOLALE 2645422 0131 Tsetsejwe Primary School P.O. Box 33 TSETSEJWE 2646103 0133 Modisaotsile Primary School P.O. Box 591 BOBONONG 2619123 0134 Motlhabaneng Primary School Private Bag 20 BOBONONG 2645541 0135 Busang Primary School P.O. Box 47 TSETSEBJE 2646144 0138 Rasetimela Primary School Private Bag 0014 BOBONONG 2619485 0139 Mabumahibidu Primary School P.O. Box 168 BOBONONG 2619040 0140 Lepokole Primary School P O Box 148 BOBONONG 4900035 0141 Agosi Primary School P O Box 1673 BOBONONG 71868614 0142 Motsholapheko Primary School P O Box 37 SEFHOPHE 2618305 0143 Mathathane DOSET P.O. Box 4 MATHATHANE 2645110 0144 Tsetsebye DOSET P.O. Box 33 TSETSEBYE 3024 Bobonong DOSET P.O. Box 483 BOBONONG 2619164 Saturday, September 25, List of Examination Centres by Region Page 1 of 39 Boteti Region Centr Name Addres Place Phone 0201 Adult Education Private Bag 1 ORAPA 0202 Baipidi Primary School P.O. -
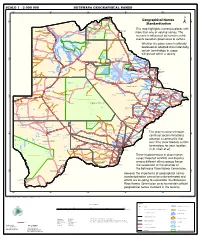
Geographical Names Standardization BOTSWANA GEOGRAPHICAL
SCALE 1 : 2 000 000 BOTSWANA GEOGRAPHICAL NAMES 20°0'0"E 22°0'0"E 24°0'0"E 26°0'0"E 28°0'0"E Kasane e ! ob Ch S Ngoma Bridge S " ! " 0 0 ' ' 0 0 ° Geographical Names ° ! 8 !( 8 1 ! 1 Parakarungu/ Kavimba ti Mbalakalungu ! ± n !( a Kakulwane Pan y K n Ga-Sekao/Kachikaubwe/Kachikabwe Standardization w e a L i/ n d d n o a y ba ! in m Shakawe Ngarange L ! zu ! !(Ghoha/Gcoha Gate we !(! Ng Samochema/Samochima Mpandamatenga/ This map highlights numerous places with Savute/Savuti Chobe National Park !(! Pandamatenga O Gudigwa te ! ! k Savu !( !( a ! v Nxamasere/Ncamasere a n a CHOBE DISTRICT more than one or varying names. The g Zweizwe Pan o an uiq !(! ag ! Sepupa/Sepopa Seronga M ! Savute Marsh Tsodilo !(! Gonutsuga/Gonitsuga scenario is influenced by human-centric Xau dum Nxauxau/Nxaunxau !(! ! Etsha 13 Jao! events based on governance or culture. achira Moan i e a h hw a k K g o n B Cakanaca/Xakanaka Mababe Ta ! u o N r o Moremi Wildlife Reserve Whether the place name is officially X a u ! G Gumare o d o l u OKAVANGO DELTA m m o e ! ti g Sankuyo o bestowed or adopted circumstantially, Qangwa g ! o !(! M Xaxaba/Cacaba B certain terminology in usage Nokaneng ! o r o Nxai National ! e Park n Shorobe a e k n will prevail within a society a Xaxa/Caecae/Xaixai m l e ! C u a n !( a d m a e a a b S c b K h i S " a " e a u T z 0 d ih n D 0 ' u ' m w NGAMILAND DISTRICT y ! Nxai Pan 0 m Tsokotshaa/Tsokatshaa 0 Gcwihabadu C T e Maun ° r ° h e ! 0 0 Ghwihaba/ ! a !( o 2 !( i ata Mmanxotae/Manxotae 2 g Botet N ! Gcwihaba e !( ! Nxharaga/Nxaraga !(! Maitengwe -

Demographic and Economic Activity in the Four Orange Basin States
Orange IWRMP Task 10: Demographics & Economic Activity Study Name: Orange River Integrated Water Resources Management Plan Report Title: Demographic and Economic Activity in the four Orange Basin States Submitted By: WRP Consulting Engineers, Jeffares and Green, Sechaba Consulting, WCE Pty Ltd, Water Surveys Botswana (Pty) Ltd Authors: D Hall, G Jennings Date of Issue: August 2007 Distribution: Botswana: DWA: 2 copies (Katai, Setloboko) Lesotho: Commissioner of Water: 2 copies (Ramosoeu, Nthathakane) Namibia: MAWRD: 2 copies (Amakali) South Africa: DWAF: 2 copies (Pyke, van Niekerk) GTZ: 2 copies (Vogel, Mpho) Reports: Review of Existing Infrastructure in the Orange River Catchment Review of Surface Hydrology in the Orange River Catchment Flood Management Evaluation of the Orange River Review of Groundwater Resources in the Orange River Catchment Environmental Considerations Pertaining to the Orange River Summary of Water Requirements from the Orange River Water Quality in the Orange River Demographic and Economic Activity in the four Orange Basin States Current Analytical Methods and Technical Capacity of the four Orange Basin States Institutional Structures in the four Orange Basin States Legislation and Legal Issues Surrounding the Orange River Catchment Summary Report 13/11/2007 i Final Orange IWRMP Task 10: Demographics & Economic Activity TABLE OF CONTENTS 1 INTRODUCTION ..................................................................................................................... 2 2 OVERVIEW OF DEMOGRAPHIC TRENDS IN THE -
Statistics Botswana
STATISTICS BOTSWANA TOURISM STATISTICS ANNUAL REPORT 2014 Copyrights © Statistics Botswana 2016 Statistics Botswana. Private Bag 0024 Botswana Tel: (267) 367 1300. Fax: (267) 395 2201.Email: [email protected] Website: www.cso.gov.bw TOURISM STATISTICS ANNUAL REPORT 2014 Published by Statistics Botswana, Private Bag 0024, Gaborone Tel: (267) 3931300 Fax: (267) 3952201/3935628 E-mail: [email protected] Website: www.cso.gov.bw COPYRIGHT RESERVED Extracts may be published if source is duly acknowledged. ISBN: 978-99968-464-4-1 PREFACE The Tourism Statistics Annual report is one of Statistics Botswana’s annual publications. The purpose of this report is to provide up to date statistics to policy makers and all other stakeholders in the development and management of the Tourism Sector in Botswana. The information contained in this publication is compiled from completed immigration arrival/departure forms. Travelers entering and leaving the country are required to complete arrival/departure forms at all gazetted points of entry/departure. This covers all land borders as well as airports. The report gives arrivals and departures statistics during 2014 and follows the 2013 report released in June 2015. Due to technical challenges, the 2011 report will never be released and the series of Tourism Statistics Annual Reports as a result has no data for that year. Users who require more information can contact the Directorate of Stakeholder Relations at 3671300. All Statistics Botswana outputs/publications are available on the website at www.cso.gov.bw and at the Statistics Botswana Library (Head-Office, Gaborone). We sincerely thank all stakeholders involved in the formulation of this report, particularly the Department of Immigration and Citizenship for their continued support and feedback, as we strive to better serve Batswana and all other important users of our services. -

Questions 1. Kgosi Ds Toto Ii (Kgalagadi South Region)
NTLO YA DIKGOSI O R D E R P A P E R (TUESDAY 25TH JUNE, 2019) QUESTIONS 1. KGOSI D. S. TOTO II (KGALAGADI SOUTH REGION): To ask the Minister (701) of Finance and Economic Development whether he will upgrade the Makopong, Middlepits and Bokspits border posts to cater for good livestock breeds purchased from South Africa by Batswana so as to address the long distance currently travelled to McCarthy’s Rust and Bray border posts to access services. 2. KGOSI D. S. TOTO II (KGALAGADI SOUTH REGION): To ask the Minister (703) of Finance and Economic Development if he will extend the hours of operation at Hereford, Makopong, Middlepits and Bokspits border posts. 3. KGOSI D. S. TOTO II (KGALAGADI SOUTH REGION): To ask the Minister (707) of Environment, Natural Resources Conservation and Tourism to update this Honourable House on progress made to give farmers including Young Farmers, part of the Wildlife Management Areas to address shortage of grazing land, stock theft and movement of animals to South Africa. 4. KGOSI C. COCK (THAMAGA REGION): To ask the Minister of (708) Employment, Labour Productivity and Skills Development to explain:- (i) what the law states on employment of security personnel regarding emolument; (ii) if he is aware that there are security companies that pay such workers as late as mid-month following the supposed month of payment; and if so, (iii) what action can be taken against such companies. 5. KGOSI P. J. CHIKA III (CHOBE REGION): To ask the Minister of Local (709) Government and Rural Development to explain why there has been an overstay of extension workers in the Chobe Region. -

List of Schools Visited for Monitoring Visits
LIST OF SCHOOLS VISITED FOR MONITORING VISITS CENTRAL INSPECTORAL AREA LOCATION NAME OF SCHOOL MMADINARE Diloro Diloro MMADINARE Mmadinare Kelele MMADINARE Kgagodi Kgagodi MMADINARE Mmadinare Mmadinare MMADINARE Mmadinare Phethu Mphoeng MMADINARE Robelela Robelela MMADINARE Gojwane Sedibe MMADINARE Serule Serule MMADINARE Mmadinare Tlapalakoma BOTETI Rakops Etsile BOTETI Khumaga Khumaga BOTETI Khwee Khwee BOTETI Mopipi Manthabakwe BOTETI Mmadikola Mmadikola BOTETI Letlhakane Mokane BOTETI Mokoboxane Mokoboxane BOTETI Mokubilo Mokubilo BOTETI Moreomaoto Moreomaoto BOTETI Mosu Mosu BOTETI Motlopi Motlopi BOTETI Letlhakane Retlhatloleng Selibe Phikwe Selibe Phikwe Boitshoko Selibe Phikwe Selibe Phikwe Boswelakgomo Selibe Phikwe Selibe Phikwe Phikwe Selibe Phikwe Selibe Phikwe Tebogo BOBIRWA Bobonong Bobonong BOBIRWA Gobojango Gobojango BOBIRWA Bobonong Mabumahibidu BOBIRWA Bobonong Madikwe BOBIRWA Mogapi Mogapi BOBIRWA Molalatau Molalatau BOBIRWA Bobonong Rasetimela BOBIRWA Semolale Semolale BOBIRWA Tsetsebye Tsetsebye 1 | P a g e MAHALAPYE WEST Bonwapitse Bonwapitse MAHALAPYE WEST Mahalapye Leetile MAHALAPYE WEST Mokgenene Mokgenene MAHALAPYE WEST Moralane Moralane MAHALAPYE WEST Mosolotshane Mosolotshane MAHALAPYE WEST Otse Setlhamo MAHALAPYE WEST Mahalapye St James MAHALAPYE WEST Mahalapye Tshikinyega MHALAPYE EAST Mahalapye Flowertown MHALAPYE EAST Mahalapye Mahalapye MHALAPYE EAST Matlhako Matlhako MHALAPYE EAST Mmaphashalala Mmaphashalala MHALAPYE EAST Sefhare Mmutle PALAPYE NORTH Goo-Sekgweng Goo-Sekgweng PALAPYE NORTH Goo-Tau Goo-Tau -

Solar-Powered Desalination
The International Development Research Centre is a public corporation created by the Parliament of Canada in 1970 to support research designed to adapt science and technology to the needs of developing countries. The Centre's activity is concentrated in six sectors: agriculture, food, and nutrition sciences; health sciences; information sciences; social sciences; earth and engineering sciences; and commwtications. IDRC is financed solely by the Parliament of Canada; its policies, however, arc set by an international Board of Governors. The Centre's headquarters arc located in Africa, Asia, Latin America, and the Middle East. IDRC-TS65e Solar-Powered Desalination A case study from Botswana by R. Yates, T. Woto, and J.T. Tlhage © International Development Research Centre 1990 PO Box 8500, Ottawa, ON, Canada KlG 3H9 Yates, R. Woto, T. Tlhage, J.T. IDRC-TS65e Solar-powered desalination : a case study from Botswana. Ottawa, Ont., IDRC, 1990, viii + 55 p. : ill. (fechnical study I IDRC) /Desalination/, /drinking water/, /water supply/, /solar energy/, /Botswana/ - /appropriate technology/, /costs/, /maintenance and repair/, references. UDC: 551.464:628.16(681) ISBN: 0-88936-554-7 A microfiche edition is available. The views expressed in this publication are those of the authors and do not necessarily represent the views of the International Development Research Centre. Mention of proprietary names does not constitute erulorsement of the product and is given onl,y for information. Printed in Singapore Abstract In Africa, chronic drought conditions are reducing access to and the quality of drinking water. In Botswana, recurring droughts have left 80% of the population reliant on water from boreholes. -

Public Primary Schools
PRIMARY SCHOOLS CENTRAL REGION NO SCHOOL ADDRESS LOCATION TELE PHONE REGION 1 Agosi Box 378 Bobonong 2619596 Central 2 Baipidi Box 315 Maun Makalamabedi 6868016 Central 3 Bobonong Box 48 Bobonong 2619207 Central 4 Boipuso Box 124 Palapye 4620280 Central 5 Boitshoko Bag 002B Selibe Phikwe 2600345 Central 6 Boitumelo Bag 11286 Selibe Phikwe 2600004 Central 7 Bonwapitse Box 912 Mahalapye Bonwapitse 4740037 Central 8 Borakanelo Box 168 Maunatlala 4917344 Central 9 Borolong Box 10014 Tatitown Borolong 2410060 Central 10 Borotsi Box 136 Bobonong 2619208 Central 11 Boswelakgomo Bag 0058 Selibe Phikwe 2600346 Central 12 Botshabelo Bag 001B Selibe Phikwe 2600003 Central 13 Busang I Memorial Box 47 Tsetsebye 2616144 Central 14 Chadibe Box 7 Sefhare 4640224 Central 15 Chakaloba Bag 23 Palapye 4928405 Central 16 Changate Box 77 Nkange Changate Central 17 Dagwi Box 30 Maitengwe Dagwi Central 18 Diloro Box 144 Maokatumo Diloro 4958438 Central 19 Dimajwe Box 30M Dimajwe Central 20 Dinokwane Bag RS 3 Serowe 4631473 Central 21 Dovedale Bag 5 Mahalapye Dovedale Central 22 Dukwi Box 473 Francistown Dukwi 2981258 Central 23 Etsile Majashango Box 170 Rakops Tsienyane 2975155 Central 24 Flowertown Box 14 Mahalapye 4611234 Central 25 Foley Itireleng Box 161 Tonota Foley Central 26 Frederick Maherero Box 269 Mahalapye 4610438 Central 27 Gasebalwe Box 79 Gweta 6212385 Central 28 Gobojango Box 15 Kobojango 2645346 Central 29 Gojwane Box 11 Serule Gojwane Central 30 Goo - Sekgweng Bag 29 Palapye Goo-Sekgweng 4918380 Central 31 Goo-Tau Bag 84 Palapye Goo - Tau 4950117 -

Geological Survey Department
REPUBLIC OF BOTSWANA ;". ANNUAL REPORT OFTHE GEOLOGICAL SURVEY DEPARTMENT FOR THE YEAR 199J-; PRICE: P3,OO Printed by the Government Printer, Gaborone Botswana GEOLOGICAL SURVEY DEPARTMENT (Director: T. P. Machacha) ANNUAL REPORT OF THE GEOLOGICAL SURVEY DEPARTMENT FOR THE YEAR 1992 PUblished by The Director Geological Survey Department Private Bag 14, Lobatse, Botswana. With the authority of The Ministry of Mineral Resources and Water Affairs Republic of Botswana 1. GENERAL The Geological Survey remained within the Ministry of Mineral Resources and Water Affairs and continued with its main functions of gathering, assessing and disseminating all data related to the rocks, mineral deposits and grouhdwater resources of Botswana. The departmental organisational structure continued to consist of the Directorate, four operational divisions of Regional Geology, Economic Geology, Hydrogeology and Geophysics together with an Administrative Division. Support to the main divisions was provided by the Drawing Office, Technical Records and Library, Chemistry and Mineral Dressing Laboratories. During the year the staffing position within the Department was consolidated with a full establishment of professional staff. There were no changes in the Directorate although the Deputy Director spent much of the year in Canada completing his PhD studies. The Principal Regional Geologist, Mr D P Piper, returned to the U K in July and was replaced by Dr R M Key who arrived from the U K in October. Within the Economic Division the evaluation of industrial minerals continued to be given priority with extensive investigations in the Dukwe-Matsitama, Selibe-Phikwe and Palapye areas. The writing of the gold monograph continued, as did the exploration for base and precious metals in the Maitengwe Schist Belt. -

Botswana & Namibia
0 200 km Botswana & Namibia 0 120 miles ZAMBIA Skeleton Coast Etosha National Park Victoria Falls ANGOLA Cubango Tsodilo Hills Steeped in myth and Watching wildlife doesn't Katima Mpalila Zambezi The mightiest waterfall Ruacana Ancient San Mulilo NP mist get easier ANGOLA Imusho Island Lakeon eaKaribarth Falls rock art Calueque Katwitwi Kasane Otjinungwa Oshikango River Calai Mudumu Chobe Livingstone ZIMBABWE Skelet Ruacana Nkurenkuru Andara NP River Victoria Falls Okongwati Oshakati CAPRIVI STRIP Linyanti Kasane Ehomba Bwabwata NP Chobe FR Zambezi (1868m) Ondangwa OWAMBO Rundu Mahango GR FR River on Ongandjera REGION Shakawe Mamili NP Kazuma KAOKOVELD Opuwo Lake KAVANGO Tsodilo 18ºS Coast Savuti FR Pandamatenga Chobe National Park Schwarze Kuppen Oponono REGION Hills An astounding array Mangetti Chobe NP Cabo Fria (1869m) Etosha Khaudum Xaa Moremi Wilderness Karakuwisa Etsha 6 Sibuyu of wildlife Pan NP Nxaunxau GR FR Purros Etosha Tsumeb Kudumane Kano Gumare Sesfontein NP Maroelaboom Tsumkwe Okavango Moremi Game Reserve Rocky Point Vlei Delta Nxai Botswana’s wildlife Nokaneng Shorobe Pan River River Kamanjab Otavi Grootfontein Nxai Pan NP central DAMARALAND Aha Hills Konde Hoanib OTJOZONDJUPA Maun Matlapaneng Gweta Palmwag (1250m) Gcwihaba Nata Nata Bulawayo Omatako River (Drotsky's) Cave Toteng Sanctuary Semowane Terrace Bay River Outjo Waterberg Petrified Plateau Park Sehithwa Tutume Otjosondjou Makgadikgadi Ntwetwe Plumtree 20ºS Torra Bay Uniab Forest Khorixas Pans NP Masunga Otjiwarongo Okakarara River Pan Siviya Twyfelfontein Sowa -

Review of Groundwater Resources in the Orange River Catchment
Study Name: Orange River Integrated Water Resources Management Plan Report Title: Review of Groundwater Resources in the Orange River Catchment Submitted By: WRP Consulting Engineers, Jeffares and Green, Sechaba Consulting, WCE Pty Ltd, Water Surveys Botswana (Pty) Ltd Authors: A Viles Date of Issue: August 2007 Distribution: Botswana: DWA: 2 copies (Katai, Setloboko) Lesotho: Commissioner of Water: 2 copies (Ramosoeu, Nthathakane) Namibia: MAWRD: 2 copies (Amakali) South Africa: DWAF: 2 copies (Pyke, van Niekerk) GTZ: 2 copies (Vogel, Mpho) Reports: Review of Existing Infrastructure in the Orange River Catchment Review of Surface Hydrology in the Orange River Catchment Flood Management Evaluation of the Orange River Review of Groundwater Resources in the Orange River Catchment Environmental Considerations Pertaining to the Orange River Summary of Water Requirements from the Orange River Water Quality in the Orange River Demographic and Economic Activity in the four Orange Basin States Current Analytical Methods and Technical Capacity of the four Orange Basin States Institutional Structures in the four Orange Basin States Legislation and Legal Issues Surrounding the Orange River Catchment Summary Report TABLE OF CONTENTS 1 INTRODUCTION ..................................................................................................................... 1 1.1 Background ................................................................................................................... 1 1.2 SADC Protocol ............................................................................................................. -

Moswete N.Pdf
STAKEHOLDER PERSPECTIVES ON THE POTENTIAL FOR COMMUNITY-BASED ECOTOURISM DEVELOPMENT AND SUPPORT FOR THE KGALAGADI TRANSFRONTIER PARK IN BOTSWANA By NAOMI NOMSA MOSWETE A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2009 1 © 2009 Naomi Nomsa Moswete 2 To the memory of my beloved parents: Morwadi and Botha Moatshe, and to my husband, Mokgweetsi for his constant love and support during my academic journey. 3 ACKNOWLEDGMENTS My study program was made possible by the generous support of many individuals and organizations, which aided and financed this research. I am particularly indebted to the W.K. Kellogg Foundation via Leadership Initiatives for Southern Africa (LISA) without whom I could not have embarked on and completed this project. The study is a contribution to the Foundation’s mission in support of the development of healthy and sustainable rural communities in Southern Africa. I am deeply indebted to the Kellogg Foundation, which played a key role in all stages of my doctoral program – from course work to field data collection and analysis. I extend my sincere appreciation to all staff at AED in Botswana (Imelda, Disa, Thandi, Moniemang), and those in Washington DC, for the invaluable support they granted me throughout my academic and spiritual journeys. I would like to express my profound gratitude to Viwe Mtshontshi and Phillip Hesser for the patience, cooperation and kind support accorded me throughout my doctoral study at the University of Florida. I also thank the University of Botswana, which played an important role throughout this program.