Synercid I.V
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antimicrobial Resistance and Disinfectants Susceptibility of Persistent Bacteria in a Tertiary Care Hospital
Journal of Microbiology and Antimicrobials Vol. 2(7), pp. xx-xx, October 2010 Available online http://www.academicjournals.org/JMA ISSN 2141-2308 ©2010 Academic Journals Full Length Research Paper Antimicrobial resistance and disinfectants susceptibility of persistent bacteria in a tertiary care hospital Maria Lucia Morcerf Bouzada1, Vania Lucia Silva1, Felipe Augusto Sa Moreira1, Girlene Alves Silva2 and Claudio Galuppo Diniz1* 1Department of Parasitology, Microbiology and Immunology, Laboratory of Bacterial Physiology and Molecular Genetics, Institute of Biological Sciences, Federal University of Juiz de Fora, Juiz de Fora/MG,36036-900, Brazil. 2Department of Applied Nursing, School of Nursing, Federal University of Juiz de Fora, Juiz de Fora/MG, 36036-900, Brazil. Accepted 22 October, 2010 It is well known that putative pathogenic bacteria are ubiquitous and widely distributed in the hospital environment. This study aimed to detect bacterial persistence in the nosocomial environment (different critical areas of the hospital) after mopping by the cleaning staff. Susceptibility patterns to antimicrobial drugs and disinfectants commonly used in health services were also investigated by disk diffusion and agar dilution tests. Rinse water from mops was processed for isolation of Enterobacteriaceae (GNR), non-fermenting Gram-negative rods (NFGNR), coagulase-negative staphylococci (CNS) and enterococci (ENT). Microorganisms were biochemically characterized and 547 strains were recovered. Only CNS and NFGNR were isolated in all critical areas. Overall 67% of the isolated bacteria were resistant to more than three drugs, being considered as multiresistant. Disinfectants were effective in concentrations ranging from 0.125 to 1%. Hospitals provide reservoirs of multiresistant microorganisms borne by patients and staff, but the hospital environment may be an important repository. -

Identification of Genes Involved in Acid Tolerance, Antimicrobial Resistance and Virulence of Enterococcus Faecium
Identification of genes involved in acid tolerance, antimicrobial resistance and virulence of Enterococcus faecium Thesis submitted by Hashimatul Fatma binti Hashim For the degree of DOCTOR OF PHILOSOPHY in the Faculty of Medical Sciences University College London Division of Microbial Diseases UCL Eastman Dental Institute 256 Gray’s Inn Road London WC1X 8LD UK 2016 Declaration I hereby certify that the work embodied in this thesis is the result of my own investigation, except where otherwise stated. 2 Abstract Enterococcus faecium is an opportunistic human nosocomial pathogen that has developed resistance to many existing antimicrobial therapies. Treatment of enterococcal infections is becoming increasingly challenging and there are limited therapeutic options against multidrug-resistant enterococci. The work described in this thesis aimed to identify genes involved in resistance to host stresses and virulence as these could potentially be future therapeutic targets. An E. faecium transposon mutant library was screened for altered resistance to lysozyme and to nisin as a model antimicrobial peptide. This approach led to the identification of several genes that contribute to lysozyme and nisin resistance. A number of mutants that were sensitive to nisin had a transposon insertion in a gene predicted to encode a tyrosine decarboxylase. It was shown that the tyrosine decarboxylase plays a role in acid tolerance and mediates virulence of E. faecium in a Galleria mellonella larvae infection model. A targeted genetic approach was used to examine the role of an E. faecium serine threonine protein kinase (Stk1) in antimicrobials resistance, host cell stresses and virulence. Disruption of the stk1 gene led to higher sensitivity to antibiotics that target the penicillin- binding proteins and bile salts compared to the wild type. -
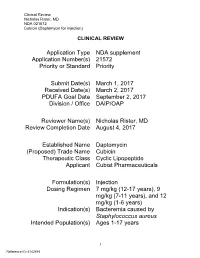
Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for Injection)
Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for injection) CLINICAL REVIEW Application Type NDA supplement Application Number(s) 21572 Priority or Standard Priority Submit Date(s) March 1, 2017 Received Date(s) March 2, 2017 PDUFA Goal Date September 2, 2017 Division / Office DAIP/OAP Reviewer Name(s) Nicholas Rister, MD Review Completion Date August 4, 2017 Established Name Daptomycin (Proposed) Trade Name Cubicin Therapeutic Class Cyclic Lipopeptide Applicant Cubist Pharmaceuticals Formulation(s) Injection Dosing Regimen 7 mg/kg (12-17 years), 9 mg/kg (7-11 years), and 12 mg/kg (1-6 years) Indication(s) Bacteremia caused by Staphylococcus aureus Intended Population(s) Ages 1-17 years 1 Reference ID: 4142515 Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for injection) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 7 1.1 Recommendation on Regulatory Action ............................................................. 7 1.2 Risk Benefit Assessment .................................................................................... 7 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies ... 8 1.4 Recommendations for Postmarket Requirements and Commitments ................ 8 2 INTRODUCTION AND REGULATORY BACKGROUND ........................................ 8 2.1 Product Information ............................................................................................ 8 2.2 Tables of Currently Available Treatments -

Infant Antibiotic Exposure Search EMBASE 1. Exp Antibiotic Agent/ 2
Infant Antibiotic Exposure Search EMBASE 1. exp antibiotic agent/ 2. (Acedapsone or Alamethicin or Amdinocillin or Amdinocillin Pivoxil or Amikacin or Aminosalicylic Acid or Amoxicillin or Amoxicillin-Potassium Clavulanate Combination or Amphotericin B or Ampicillin or Anisomycin or Antimycin A or Arsphenamine or Aurodox or Azithromycin or Azlocillin or Aztreonam or Bacitracin or Bacteriocins or Bambermycins or beta-Lactams or Bongkrekic Acid or Brefeldin A or Butirosin Sulfate or Calcimycin or Candicidin or Capreomycin or Carbenicillin or Carfecillin or Cefaclor or Cefadroxil or Cefamandole or Cefatrizine or Cefazolin or Cefixime or Cefmenoxime or Cefmetazole or Cefonicid or Cefoperazone or Cefotaxime or Cefotetan or Cefotiam or Cefoxitin or Cefsulodin or Ceftazidime or Ceftizoxime or Ceftriaxone or Cefuroxime or Cephacetrile or Cephalexin or Cephaloglycin or Cephaloridine or Cephalosporins or Cephalothin or Cephamycins or Cephapirin or Cephradine or Chloramphenicol or Chlortetracycline or Ciprofloxacin or Citrinin or Clarithromycin or Clavulanic Acid or Clavulanic Acids or clindamycin or Clofazimine or Cloxacillin or Colistin or Cyclacillin or Cycloserine or Dactinomycin or Dapsone or Daptomycin or Demeclocycline or Diarylquinolines or Dibekacin or Dicloxacillin or Dihydrostreptomycin Sulfate or Diketopiperazines or Distamycins or Doxycycline or Echinomycin or Edeine or Enoxacin or Enviomycin or Erythromycin or Erythromycin Estolate or Erythromycin Ethylsuccinate or Ethambutol or Ethionamide or Filipin or Floxacillin or Fluoroquinolones -

Antimicrobial Stewardship Guidance
Antimicrobial Stewardship Guidance Federal Bureau of Prisons Clinical Practice Guidelines March 2013 Clinical guidelines are made available to the public for informational purposes only. The Federal Bureau of Prisons (BOP) does not warrant these guidelines for any other purpose, and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. Consult the BOP Clinical Practice Guidelines Web page to determine the date of the most recent update to this document: http://www.bop.gov/news/medresources.jsp Federal Bureau of Prisons Antimicrobial Stewardship Guidance Clinical Practice Guidelines March 2013 Table of Contents 1. Purpose ............................................................................................................................................. 3 2. Introduction ...................................................................................................................................... 3 3. Antimicrobial Stewardship in the BOP............................................................................................ 4 4. General Guidance for Diagnosis and Identifying Infection ............................................................. 5 Diagnosis of Specific Infections ........................................................................................................ 6 Upper Respiratory Infections (not otherwise specified) .............................................................................. -

Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020
First independent framework for assessing pharmaceutical company action Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020 ACKNOWLEDGEMENTS The Access to Medicine Foundation would like to thank the following people and organisations for their contributions to this report.1 FUNDERS The Antimicrobial Resistance Benchmark research programme is made possible with financial support from UK AID and the Dutch Ministry of Health, Welfare and Sport. Expert Review Committee Research Team Reviewers Hans Hogerzeil - Chair Gabrielle Breugelmans Christine Årdal Gregory Frank Fatema Rafiqi Karen Gallant Nina Grundmann Adrián Alonso Ruiz Hans Hogerzeil Magdalena Kettis Ruth Baron Hitesh Hurkchand Joakim Larsson Dulce Calçada Joakim Larsson Marc Mendelson Moska Hellamand Marc Mendelson Margareth Ndomondo-Sigonda Kevin Outterson Katarina Nedog Sarah Paulin (Observer) Editorial Team Andrew Singer Anna Massey Deirdre Cogan ACCESS TO MEDICINE FOUNDATION Rachel Jones The Access to Medicine Foundation is an independent Emma Ross non-profit organisation based in the Netherlands. It aims to advance access to medicine in low- and middle-income Additional contributors countries by stimulating and guiding the pharmaceutical Thomas Collin-Lefebvre industry to play a greater role in improving access to Alex Kong medicine. Nestor Papanikolaou Address Contact Naritaweg 227-A For more information about this publication, please contact 1043 CB, Amsterdam Jayasree K. Iyer, Executive Director The Netherlands [email protected] +31 (0) 20 215 35 35 www.amrbenchmark.org 1 This acknowledgement is not intended to imply that the individuals and institutions referred to above endorse About the cover: Young woman from the Antimicrobial Resistance Benchmark methodology, Brazil, where 40%-60% of infections are analyses or results. -

Quinupristin/Dalfopristin
Reprinted from www.antimicrobe.org Quinupristin/Dalfopristin Antibiotic Class: Streptogramin Antimicrobial Activity: Gram-positive bacteria. In-vitro data suggests streptogramins possess activity against gram-negative upper respiratory tract pathogens and gram-negative anaerobes. Mechanism of Action: Inhibition of mRNA translation by binding to the 50S subunit of bacterial ribosomes. Pharmacodynamics: Predominantly independent of concentration once above four times the MIC of common Staphylococci and Streptococci. Pharmacokinetics: (7.5mg/kg dose at steady state) Cmax: 3.2 and 7.96mg/L (quinupristin and dalfopristin respectively) Half-life: 3.07 and 1.04 hours (quinupristin and dalfopristin respectively) Volume of distribution: 0.45 and 0.24L/kg (quinupristin and dalfopristin respectively) Adverse Effects: Venous irritation due to quinupristin/dalfopristin is common. In comparative trials approximately 40% of patients experienced infusion site adverse reactions compared to 25% of comparator treated patients. Increasing the infusion volume or administering the drug via central line may attenuate this reaction. In two compassionate use studies, arthralgias (9.1%) and myalgias (6.6%) were the most common adverse event related to quinupristin/dalfopristin. Hyperbilirubinemia was documented in up to 25% of quinupristin/dalfopristin treated patients in compassionate use/non-comparative studies. Dosage: Intravenous only – available as 500mg (150mg quinupristin and 350mg dalfopristin) and 600mg (180mg quinupristin and 420mg dalfopristin) powder for reconstitution vials Serious or life-threatening infections associated with vancomycin-resistant Enterococcus faecium – 7.5mg/kg every 8 hours Complicated skin and skin structure infection caused by methicillin-susceptible S. aureus or S. pyogenes – 7.5mg/kg every 12 hours Disease state based dosing: Hepatic failure: Although no dosage official dosage adjustment recommendations exist, pharmacokinetic data in patients with hepatic cirrhosis (Childs-Pugh class A or B) suggest that dosage adjustments may be necessary. -

General a Number of Factors Could Reduce the Efficacy of This
AUSTRALIAN PRODUCT INFORMATION Administration It is strongly recommended that every time that GAMUNEX® is administered to a patient, the name Use in the elderly GAMUNEX® If dilution is required, GAMUNEX® may be diluted with 5% dextrose in water (D5/W). Do not and batch number of the product are recorded using the supplied tear off labels in order to maintain See Section 4.4 Special warnings and precautions for use: Use in renal impairment. a link between the patient and the batch of the product. (NORMAL IMMUNOGLOBULIN (HUMAN), 10%, INTRAVENOUS SOLUTION VIAL) dilute with saline. Paediatric use Anaphylaxis GAMUNEX® should be inspected visually for particulate matter and discoloration prior to adminis - No data available. GAMUNEX® should be administered only intravenously or subcutaneously. On rare occasions, tration, whenever solution and container permit. Do not use if turbid and/or if discoloration is Effects on laboratory tests 1 NAME OF THE MEDICINE observed. treatment with an immune globulin preparation may cause a precipitous fall in blood pressure and a Interference with serological testing Normal immunoglobulin (Human), 10%, for Intravenous or Subcutaneous Administration For intravenous or subcutaneous administration, GAMUNEX® should be at room temperature during clinical picture of anaphylaxis, even when the patient is not known to be sensitive to immune globulin administration. preparations. Adrenalin and other appropriate supportive care should be available for the treatment After injection of immunoglobulin the transitory rise of the various passively transferred antibodies of an acute anaphylactic reaction. in the patient’s blood may result in misleading positive results in serological testing. Passive Intravenous (IV) True anaphylactic reactions to GAMUNEX® may occur in recipients with documented prior histories transmission of antibodies to erythrocyte antigens e.g. -

Polymyxin B Use Associated with Severe Hypotensive Episodes
ntimicrob Mehta et al., J Antimicro 2015, 1:1 A ia f l o A l g DOI: 10.4172/2472-1212.1000102 a e n n r Journal of t u s o J ISSN: 2472-1212 Antimicrobial Agents Case Report Open Access Polymyxin B use Associated with Severe Hypotensive Episodes Mehta M1*, Baron JM1, Nelson BC1, Muir J1 and Pereira MR2 1NewYork-Presbyterian Hospital, USA 2Columbia University Medical Center, USA Abstract Polymyxin B was developed in the 1940s but was infrequently used because of renal toxicity. Since the rise of infections due to multidrug resistant gram-negative organisms, polymyxin B has re-emerged as an important agent. However, its toxicity is still not fully elucidated. In this report, we describe two cases of multiple hypotensive events occurring after polymyxin B administration. Management strategies, such as slowing the infusion rate and administering diphenhydramine, did not mitigate the hypotension. We also describe relatively high polymyxin levels correlated with this effect in one of these cases. Keywords: Polymyxin; Toxicity; Hypotension While hypotension is usually a complication of sepsis, details in this case suggest that the episodes of hypotension are more related Case 1 to polymyxin B administration than an uncontrolled infection. The A 35-year-old-woman was admitted to our hospital for management episodes of hypotension started to occur only after polymyxin B and of newly diagnosed acute promyelocytic leukemia. Twelve days after other antibiotics were initiated. There is good evidence, with negative initiation of chemotherapy, she developed a fever to 38.0°C. Cultures follow-up cultures, resolution of fever, and improving imaging, that of her urine and blood grew a carbapenem-resistant Escherichia coli the infection was controlled by the time that the hypotensive episodes susceptible to polymyxin B (minimum inhibitory concentration started. -

Remifentanil Hydrochloride)
NDA 20-630/S-005 Page 3 Ultiva® for Injection (remifentanil hydrochloride) For IV Use Only DESCRIPTION ULTIVA (remifentanil hydrochloride) for Injection is a µ-opioid agonist chemically designated as a 3- [4-methoxycarbonyl-4-[(1-oxopropyl)phenylamino]-1-piperidine]propanoic acid methyl ester, hydrochloride salt, C20H28N2O5·HCl, with a molecular weight of 412.91. It has the following chemical structure: ULTIVA is a sterile, nonpyrogenic, preservative-free, white to off-white lyophilized powder for intravenous (IV) administration after reconstitution and dilution. Each vial contains 1, 2, or 5 mg of remifentanil base; 15 mg glycine; and hydrochloric acid to buffer the solutions to a nominal pH of 3 after reconstitution. When reconstituted as directed, solutions of ULTIVA are clear and colorless and contain remifentanil hydrochloride (HCl) equivalent to 1 mg/mL of remifentanil base. The pH of reconstituted solutions of ULTIVA ranges from 2.5 to 3.5. Remifentanil HCl has a pKa of 7.07. Remifentanil HCl has an n-octanol:water partition coefficient of 17.9 at pH 7.3. CLINICAL PHARMACOLOGY ULTIVA is a µ-opioid agonist with rapid onset and peak effect, and short duration of action. The µ-opioid activity of ULTIVA is antagonized by opioid antagonists such as naloxone. Unlike other opioids, ULTIVA is rapidly metabolized by hydrolysis of the propanoic acid-methyl ester linkage by nonspecific blood and tissue esterases. ULTIVA is not a substrate for plasma cholinesterase (pseudocholinesterase) and, therefore, patients with atypical cholinesterase are expected to have a normal duration of action. Pharmacodynamics: The analgesic effects of ULTIVA are rapid in onset and offset. -

Tackling Pristinamycin IIB Problems: Synthetic Studies Toward Some Fluorinated Analogs †
Proceeding Paper Tackling Pristinamycin IIB Problems: Synthetic Studies toward Some Fluorinated Analogs † Assia Chebieb * and Chewki Ziani-Cherif Department of Chemistry, University Abou-Bekr Belkaid of Tlemcen/Laboratory of Catalysis and Synthesis in Organic Chemistry LCSCO, 13000 Tlemcen, Algeria; [email protected] * Correspondence: [email protected] † Presented at the 24th International Electronic Conference on Synthetic Organic Chemistry, 15 November–15 December 2020; Available online: https://ecsoc-24.sciforum.net/. Abstract: Streptogramins are potent antibiotics against numerous highly resistant pathogens and therefore are used in last-resort human therapy. These antibiotics are formed of both A- and B-group compounds named pristinamycins that differ in their basic primary structures. Although pristina- mycin IIB is among the most interesting antibiotics in this family, it presents numerous problems related to its chemical structure, such as instability at most pH levels, weak solubility in water, and resistance by bacteria. As a response to the need for developing new antimicrobial agents, we have designed a new analog of pristinamycin IIB, based most importantly on the introduction of fluorine atoms. We conjectured indeed that the introduced modifications may solve the above-mentioned problems exhibited by pristinamycin IIB. Our multistep synthetic approach relies on few key reac- tions, namely a Wittig reaction, a Grubbs reaction, and dihydroxy, -difluoro API (Advanced Phar- maceutical Intermediate) synthesis Keywords: streptogramins; pristinamycins IIB; fluorine Citation: Chebieb, A.; Ziani-Cherif, C. Tackling Pristinamycin IIB Problems: Synthetic Studies toward Some Fluorinated Analogs. Chem. The first antibiotic mixture of streptogramin antibiotics was isolated from the pro- Pro. 2021, 3, 107. https://doi.org/ ducer strain Streptomyces graminofaciens from a soil sample in Texas [1]. -

Swedres-Svarm 2019
2019 SWEDRES|SVARM Sales of antibiotics and occurrence of antibiotic resistance in Sweden 2 SWEDRES |SVARM 2019 A report on Swedish Antibiotic Sales and Resistance in Human Medicine (Swedres) and Swedish Veterinary Antibiotic Resistance Monitoring (Svarm) Published by: Public Health Agency of Sweden and National Veterinary Institute Editors: Olov Aspevall and Vendela Wiener, Public Health Agency of Sweden Oskar Nilsson and Märit Pringle, National Veterinary Institute Addresses: The Public Health Agency of Sweden Solna. SE-171 82 Solna, Sweden Östersund. Box 505, SE-831 26 Östersund, Sweden Phone: +46 (0) 10 205 20 00 Fax: +46 (0) 8 32 83 30 E-mail: [email protected] www.folkhalsomyndigheten.se National Veterinary Institute SE-751 89 Uppsala, Sweden Phone: +46 (0) 18 67 40 00 Fax: +46 (0) 18 30 91 62 E-mail: [email protected] www.sva.se Text, tables and figures may be cited and reprinted only with reference to this report. Images, photographs and illustrations are protected by copyright. Suggested citation: Swedres-Svarm 2019. Sales of antibiotics and occurrence of resistance in Sweden. Solna/Uppsala ISSN1650-6332 ISSN 1650-6332 Article no. 19088 This title and previous Swedres and Svarm reports are available for downloading at www.folkhalsomyndigheten.se/ Scan the QR code to open Swedres-Svarm 2019 as a pdf in publicerat-material/ or at www.sva.se/swedres-svarm/ your mobile device, for reading and sharing. Use the camera in you’re mobile device or download a free Layout: Dsign Grafisk Form, Helen Eriksson AB QR code reader such as i-nigma in the App Store for Apple Print: Taberg Media Group, Taberg 2020 devices or in Google Play.