Package Leaflet: Information for the User EVRA 203 Micrograms/24
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Formulation and Evaluation of Transdermal Patch and Gel of Nateglinide
Human Journals Research Article September 2015 Vol.:4, Issue:2 © All rights are reserved by C. Aparna et al. Formulation and Evaluation of Transdermal Patch and Gel of Nateglinide Keywords: Nateglinide, transdermal patch and gel, HPMC, ethyl cellulose, carbopol, PVA, PVP ABSTRACT Anusha Gundeti, C. Aparna*, Dr. Prathima Srinivas The objective of the present work was to formulate Transdermal Drug Delivery systems of Nateglinide, an Department of Pharmaceutics, Sri Venkateshwara antidiabetic drug belonging to meglitinide class with a half life of 1.5 hrs. Transdermal patches containing nateglinide were College of Pharmacy, prepared by solvent casting method using the combinations Affiliated to Osmania University, of HPMC:EC, PVA:PVP, HPMC:Eudragit RS 100, Eudragit RL100:RS100 in different proportions and by incorporating Madhapur, Hyderabad, Telangana -500081, India. different permeation enhancers (polyethylene glycol 400, Su bmission: 7 September 2015 DMSO). The transdermal patches were evaluated for their physicochemical properties like thickness, weight variation, Accepted: 11 September 2015 folding endurance, percentage moisture absorption, percentage Published: 25 September 2015 moisture loss, in-vitro diffusion studies & ex-vivo permeation studies. Transdermal Gel was formulated using HPMC, carbopol 934, carbopol 940 and methyl cellulose. Gels were evaluated for homogeneity, pH, viscosity, drug content, in-vitro diffusion studies & ex-vivo permeation studies. By comparing the drug release F5 (HPMC:EC) formulation was selected as optimized formulation as it could sustain the drug release for 12 hrs i.e. 99.2% when compared to gel. Stability studies were www.ijppr.humanjournals.com carried out according to ICH guidelines and the patches maintained integrity and good physicochemical properties during the study period. -
Preven Emergency Contraceptive
9/1/1998 1 Rx Only PREVENÔ Emergency Contraceptive Kit consisting of Emergency Contraceptive Pills and Pregnancy Test Emergency Contraceptive Pills (Levonorgestrel and Ethinyl Estradiol Tablets, USP) and Pregnancy Test The PREVENÔ Emergency Contraceptive Kit is intended to prevent pregnancy after known or suspected contraceptive failure or unprotected intercourse. Emergency contraceptive pills (like all oral contraceptives) do not protect against infection with HIV (the virus that causes AIDS) and other sexually transmitted diseases. DESCRIPTION The PREVENÔ Emergency Contraceptive Kit consists of a patient information book, a urine pregnancy test and four (4) emergency contraceptive pills (ECPs). The pills in the PREVENÔ Emergency Contraceptive Kit are combination oral contraceptives (COCs) which are used to provide postcoital emergency contraception. Each blue film-coated pill contains 0.25 mg levonorgestrel (18,19-Dinorpregn-4-en-20- yn-3-one, 13-Ethyl-17-hydroxy-, (17a)-(-), a totally synthetic progestogen, and 0.05 mg ethinyl estradiol (19-Nor-17a-pregna-1,3,5, (10)-trien-20-yne-3,17-diol). The inactive ingredients present are polacrilin potassium, lactose, magnesium stearate, hydroxypropyl methylcellulose, titanium dioxide, polyethylene glycol, polysorbate 80 and FD&C Blue No.2 Aluminum Lake. MOLECULES TO BE ADDED The Pregnancy Test uses monoclonal antibodies to detect the presence of hCG (Human Chorionic Gonadotropin) in the urine. It is sensitive to 20 – 25 mIU / mL 9/1/1998 2 CLINICAL PHARMACOLOGY ECPs are not effective if the woman is pregnant; they act primarily by inhibiting ovulation. They may also act by altering tubal transport of sperm and/or ova (thereby inhibiting fertilization), and/or possibly altering the endometrium (thereby inhibiting implantation). -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009. -

Mycophenolate: OB-GYN Contraception Counseling Referral
Current as of 6/1/2013. This document may not be part of the latest approved REMS. OB/GYN CONTRACEPTION COUNSELING LETTER Reference ID: 3194413 Current as of 6/1/2013. This document may not be part of the latest approved REMS. Letter to Ob/Gyn Contraception Counseling ((Date)) ((Recipient’s Name)) ((Recipient’s Address 1)) ((Recipient’s Address 2)) ((City, State, ZIP)) In reference to: My patient ((Patient’s Name)) Reason for the referral: Contraception counseling Dear Dr ((Recipient’s Last Name)): I am writing to you in reference to the above-named patient who is under my care for ((diagnosis)) and ((insert drug information such as drug name, when patient will begin taking the drug, if treatment has already begun, etc)). This medication contains mycophenolate, which is associated with an increased risk of first trimester pregnancy loss and congenital malformations. It is important that this patient receive contraception counseling about methods that are acceptable for use while taking mycophenolate. Prescribers of mycophenolate participate in the FDA-mandated Mycophenolate REMS (Risk Evaluation and Mitigation Strategy) to ensure that the benefits of mycophenolate outweigh the risks. The following table lists the forms of contraception that are acceptable for use during treatment with mycophenolate. Acceptable Contraception Methods for Females of Reproductive Potential Guide your patients to choose from the following birth control options: Option 1 Intrauterine devices (IUDs) Tubal sterilization Methods to Use Patient’s partner had -

Delaying Menstruation During Holidays. Norethisterone 5Mg Tds
Delaying menstruation during holidays. Norethisterone 5mg tds, started 3 days before the expected menses can be used for the postponement of menstruation and is often prescribed prior to a holiday. The effectiveness of the delay varies between individuals. So what is the problem? A review article in the Journal of Family Planning and Reproductive healthcare ( Mansour 2012) highlighted that owing to the specific structure of norethisterone, it is partly metabolised to ethinyl oestradiol. Chu et al 2007 suggested that a daily dose of norethisterone 5mg tds might be equivalent to taking 20-30mcg combined oral contraceptive pill. Therefore, prescribing therapeutic doses of norethisterone for women with significant risk factors for venous thromboembolism ( VTE) may therefore be inappropriate. Who shouldn’t be given norethisterone? Obese Personal h/o VTE Strong FH of VTE Immobile/wheelchair bound Carriers of thrombophilia Any other condition predisposing to VTE If my patient can’t take norethisterone, what are the alternatives? The metabolism to ethinyl oestradiol occurs with doses of norethisterone 5mg and over and therefore, the concern does not apply to or other progestogens or contraceptive pills containing norethisterone. Mansour suggested Medroxyprogesterone ( MPA ) 10mg three times a day to reduce heavy menstrual bleeding. Dr Sarah Grey (personal communication) recommends 20mg medroxyprogesterone to be taken daily, starting 3 days before the expected onset of menses. However, (MPA) is not licensed for this use and the prescriber should follow the rules of off label prescribing. References Safer prescribing of therapeutic norethisterone for women at risk of venous thromboembolism. Mansour JFPRHC July 2012 Formation of ethinyl oestradiol in women during treatment with norethisterone acetate. -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -
Recommendations for Contraceptive Use, 2013 Adapted from the World Health Organization Selected Practice Recommendations for Contraceptive Use, 2Nd Edition
Morbidity and Mortality Weekly Report Early Release / Vol. 62 June 14, 2013 U.S. Selected Practice Recommendations for Contraceptive Use, 2013 Adapted from the World Health Organization Selected Practice Recommendations for Contraceptive Use, 2nd Edition Continuing Education Examination available at http://www.cdc.gov/mmwr/cme/conted.html. U.S. Department of Health and Human Services Centers for Disease Control and Prevention Early Release CONTENTS CONTENTS (Continued) Introduction ............................................................................................................1 Appendix A: Summary Chart of U.S. Medical Eligibility Criteria for Methods ....................................................................................................................2 Contraceptive Use, 2010 .................................................................................. 47 How To Use This Document ...............................................................................3 Appendix B: When To Start Using Specific Contraceptive Summary of Changes from WHO SPR ............................................................4 Methods .............................................................................................................. 55 Contraceptive Method Choice .........................................................................4 Appendix C: Examinations and Tests Needed Before Initiation of Maintaining Updated Guidance ......................................................................4 Contraceptive Methods -

An Archetype Swing in Transdermal Drug Delivery
Indo American Journal of Pharmaceutical Research, 2017 ISSN NO: 2231-6876 A COMPREHENSIVE REVIEW ON MICRONEEDLES - AN ARCHETYPE SWING IN TRANSDERMAL DRUG DELIVERY G. Ravi*, N. Vishal Gupta, M. P. Gowrav Department of Pharmaceutics, JSS College of Pharmacy, JSS University, Shri Shivarathreeshwara Nagara, Mysuru, Karnataka, India. ARTICLE INFO ABSTRACT Article history Transdermal drug delivery is the non-invasive delivery of medications through the skin Received 23/12/2016 surface into the systemic circulation. The advantage of transdermal drug delivery system is Available online that it is painless technique of administration of drugs. The advantage of transdermal drug 31/01/2017 delivery system is that it is painless technique of administration of drugs. Transdermal drug delivery system can improve the therapeutic efficacy and safety of the drugs because drug Keywords delivered through the skin at a predetermined and controlled rate. Due to the various Microneedles, biomedical benefits, it has attracted many researches. The barrier nature of stratumcorneum Hypodermic Needles, poses a danger to the drug delivery. By using microneedles, a pathway into the human body Transdermal, can be recognized which allow transportation of macromolecular drugs such as insulin or Stratumcorneum, vaccine. These microneedles only penetrate outer layers of the skin, exterior sufficient not to Patch. reach the nerve receptors of the deeper skin. Thus the microneedles supplement is supposed painless and reduces the infection and injuries. Researches from the past few years showed that microneedles have emerged as a novel carrier and considered to be effective for safe and improved delivery of the different drugs. Microneedles development is created a new pathway in the drug delivery field. -

Transdermal Nicotine Maintenance Attenuates the Subjective And
Neuropsychopharmacology (2004) 29, 991–1003 & 2004 Nature Publishing Group All rights reserved 0893-133X/04 $25.00 www.neuropsychopharmacology.org Transdermal Nicotine Maintenance Attenuates the Subjective and Reinforcing Effects of Intravenous Nicotine, but not Cocaine or Caffeine, in Cigarette-Smoking Stimulant Abusers 1 1 ,1,2 Bai-Fang X Sobel , Stacey C Sigmon and Roland R Griffiths* 1Department of Psychiatry and Behavioral Science, Johns Hopkins University School of Medicine, Baltimore, MD, USA; 2Department of Neuroscience, Johns Hopkins University School of Medicine, Baltimore, MD, USA The effects of transdermal nicotine maintenance on the subjective, reinforcing, and cardiovascular effects of intravenously administered cocaine, caffeine, and nicotine were examined using double-blind procedures in nine volunteers with histories of using tobacco, caffeine, and cocaine. Each participant was exposed to two chronic drug maintenance phases (21 mg/day nicotine transdermal patch and placebo transdermal patch). Within each drug phase, the participant received intravenous injections of placebo, cocaine (15 and 30 mg/70 kg), caffeine (200 and 400 mg/70 kg), and nicotine (1.0 and 2.0 mg/70 kg) in mixed order across days. Subjective and cardiovascular data were collected before and repeatedly after drug or placebo injection. Reinforcing effects were also assessed after each injection with a Drug vs Money Multiple-Choice Form. Intravenous cocaine produced robust dose-related increases in subjective and reinforcing effects; these effects were not altered by nicotine maintenance. Intravenous caffeine produced elevations on several subjective ratings; nicotine maintenance did not affect these ratings. Under the placebo maintenance condition, intravenous nicotine produced robust dose-related subjective effects, with maximal increases similar to the high dose of cocaine; nicotine maintenance significantly decreased the subjective and reinforcing effects of intravenous nicotine. -
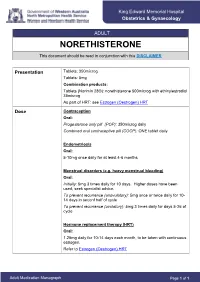
NORETHISTERONE This Document Should Be Read in Conjunction with This DISCLAIMER
King Edward Memorial Hospital Obstetrics & Gynaecology ADULT NORETHISTERONE This document should be read in conjunction with this DISCLAIMER Presentation Tablets: 350microg Tablets: 5mg Combination products: Tablets (Norimin 28®): norethisterone 500microg with ethinylestradiol 35microg As part of HRT: see Estrogen (Oestrogen) HRT Dose Contraception Oral: Progesterone only pill (POP): 350microg daily Combined oral contraceptive pill (COCP): ONE tablet daily Endometriosis Oral: 5-10mg once daily for at least 4-6 months Menstrual disorders (e.g. heavy menstrual bleeding) Oral: Initially: 5mg 3 times daily for 10 days. Higher doses have been used; seek specialist advice. To prevent recurrence (anovulatory): 5mg once or twice daily for 10- 14 days in seconf half of cycle To prevent recurrence (ovulatory): 5mg 3 times daily for days 5-26 of cycle Hormone replacement therapy (HRT) Oral: 1.25mg daily for 10-14 days each month, to be taken with continuous estrogen. Refer to Estrogen (Oestrogen) HRT Adult Medication Monograph Page 1 of 1 Norethisterone – Adult Administration Oral To be taken at the same time each day (or within 3 hours of the usual dose time). For Contraception: Start 4 weeks after the birth of baby (increased risk of abnormal vaginal bleeding if started earlier) Pregnancy 1st Trimester: Contraindicated 2nd Trimester: Contraindicated 3rd Trimester: Contraindicated Breastfeeding Considered safe to use. Progestogens are the preferred hormonal contraceptives as they do not inhibit lactation. Clinical Guidelines Estrogen (Oestrogen) HRT and Policies Progesterone Only Pill Contraception: Post Partum Gynaecology (Non-Oncological) Australian Medicines Handbook. Norethisterone. In: Australian References Medicines Handbook [Internet]. Adelaide (South Australia): Australian Medicines Handbook; 2017 [cited 2017 Apr 12]. -

A Brief Review on Transdermal Patches
Organic and Medicinal Chemistry International Journal ISSN 2474-7610 Review Article Organic & Medicinal Chem IJ Volume 7 Issue 2 - June 2018 Copyright © All rights are reserved by Nidhi Sharma DOI: 10.19080/OMCIJ.2018.07.555707 A Brief Review on Transdermal Patches Nidhi Sharma* HIMT College of Pharmacy, Greater Noida, India Submission: May 12, 2018; Published: June 05, 2018 *Corresponding author: Nidhi Sharma, HIMT College of Pharmacy, Greater Noida, India, Email: Abstract healingTransdermal to an injured drug area delivery of the system body. was An presentedadvantage toof overcome a transdermal the difficulties drug delivery of drug route delivery over especiallyother types oral of route. delivery A transdermal system such patch as oral, is a topical,medicated i.v., adhesive i.m., etc. ispatch that that the patchis placed provides on the askin controlled to deliver release a specific of the dose medication of medication into the through patient, the usually skin and through into the either bloodstream. a porous It membrane promotes covering a reservoir of medication or through body heat melting thin layers of medication embedded in the adhesive. The main disadvantage to transdermal delivery systems stems from the fact that the skin is a very effective barrier, as a result, only medications whose molecules are small can easily penetrate the skin, so it can be delivered by this method. This review article describes the overall introduction of transdermal patches including type of transdermal patches, method of preparation of transdermal -
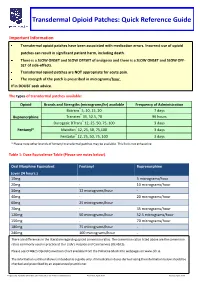
Transdermal Opioid Patches: Quick Reference Guide
Transdermal Opioid Patches: Quick Reference Guide Important Information Transdermal opioid patches have been associated with medication errors. Incorrect use of opioid patches can result in significant patient harm, including death. There is a SLOW ONSET and SLOW OFFSET of analgesia and there is a SLOW ONSET and SLOW OFF- SET of side-effects. Transdermal opioid patches are NOT appropriate for acute pain. The strength of the patch is prescribed in micrograms/hour. If in DOUBT seek advice. The types of transdermal patches available: Opioid Brands and Strengths (micrograms/hr) available Frequency of Administration Butrans® 5, 10, 15, 20 7 days Buprenorphine Transtec® 35, 52.5, 70 96 hours Durogesic DTrans® 12, 25, 50, 75, 100 3 days Fentanyl* Matrifen® 12, 25, 50, 75,100 3 days Fentadur® 12, 25, 50, 75, 100 3 days * Please note other brands of fentanyl transdermal patches may be available. This list is not exhaustive. Table 1: Dose Equivalence Table (Please see notes below). Oral Morphine Equivalent Fentanyl Buprenorphine (over 24 hours.) 10mg 5 micrograms/hour 20mg - 10 micrograms/hour 30mg 12 micrograms/hour - 40mg - 20 micrograms/hour 60mg 25 micrograms/hour 70mg - 35 micrograms/hour 120mg 50 micrograms/hour 52.5 micrograms/hour 150mg - 70 micrograms/hour 180mg 75 micrograms/hour - 240mg 100 micrograms/hour - There are differences in the literature regarding opioid conversion ratios. The conversion ratios listed above are the conversion ratios commonly used in practice at Our Lady’s Hospice and Care Service (OLH&CS). Please see OLH&CS Opioid Conversion Chart available from the Palliative Meds Info webpages on www.olh.ie.