A Small Road to Misery in Necrotizing External Otitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Download
1 Contribution of dental private practitioners to 2 publications on anatomical variations using 3 cone beam computed tomography. 4 5 Authors: 6 Hebda A1,*MS, 7 Theys S2 DDS, 8 De Roissart J3 MD, 9 Perez E4 DDS, 10 Olszewski R1,3 DDS,MD,PhD,DrSc 11 Affiliations: 12 1 Oral and maxillofacial surgery research Lab, NMSK, IREC, SSS, UCLouvain, 13 Brussels, Belgium 14 2 Department of pediatric dentistry and special care, Cliniques universitaires saint 15 Luc, UCLouvain, Brussels, Belgium 16 3 Department of oral and maxillofacial surgery, Cliniques universitaires saint Luc, 17 UCLouvain, Brussels, Belgium 18 4 Department of orthodontics, Cliniques universitaires saint Luc, UCLouvain, 19 Brussels, Belgium 20 *Corresponding author: Hebda A, Oral and maxillofacial surgery research Lab, 21 NMSK, IREC, SSS, UCLouvain, Brussels, Belgium, ORCID Id 0000-0001-5111- 22 0021 1 2 [Nemesis] Titre de l’article (PUL - En- tête paire) 23 Disclaimer: the views expressed in the submitted article are our own and not an 24 official position of the institution or funder. 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 [Nemesis] Titre de l’article (PUL - En- tête impaire) 3 61 Abstract 62 Objective: To investigate the participation of citizens-dental private practitioner in 63 scientific articles about anatomical variations on dentomaxillofacial CBCT. Our null 64 hypothesis was that private practice practitioners are not involved in publications on 65 anatomical variations using cone beam computed tomography. -

A Small Road to Misery in Necrotizing External Otitis
Published August 8, 2019 as 10.3174/ajnr.A6161 ORIGINAL RESEARCH HEAD & NECK A Persistent Foramen of Huschke: A Small Road to Misery in Necrotizing External Otitis X W.L. van der Meer, X M. van Tilburg, X C. Mitea, and X A.A. Postma ABSTRACT BACKGROUND AND PURPOSE: Necrotizing external otitis is a serious complication of external otitis with different spreading patterns. A persistent foramen of Huschke is a dehiscence located antero-inferior in the osseous external ear canal and posterior-medial to the temporomandibular joint. This dehiscence can facilitate extension of infection in an anterior pattern next to classic spread along the fissures of Santorini. The aim of this study was to define the prevalence and size of a persistent foramen of Huschke in patients with necrotizing external otitis. MATERIALS AND METHODS: We retrospectively examined 78 CT temporal bone studies (39 patients with necrotizing external otitis, 39 control subjects). The side and presence of the foramen were noted, and its prevalence was calculated. The maximal width of the foramen of Huschke was measured in the axial plane and classified as subtle, mild, moderate, or extensive. RESULTS: A persistent foramen of Huschke was present in 21 patients (26 ears) and 7 control subjects (9 ears). Prevalence was 50% (20/40) and 11.5% (9/78) in affected ears of patients with necrotizing external otitis and control subjects, respectively. Almost all affected ears showed an anterior distribution pattern of necrotizing external otitis. The extensive dehiscence was most common in affected ears. CONCLUSIONS: An anterior necrotizing external otitis spreading pattern is associated with the presence and increased size of a persis- tent foramen of Huschke. -

East and Central Africa Journal of Otolaryngology, Head and Neck Surgery July, 2020 ISSN 2664-0376 Volume 4, No
East and Central Africa Journal of Otolaryngology, Head and Neck Surgery July, 2020 ISSN 2664-0376 Volume 4, No. 2 Contents Overview of articles in this issue Editorial: Challenges of otolarygology practice in the Covid-19 era Gikonyo M .....................................................................................................................................................................Contents 1 Editorial Editor's note: Making a life Gitonga S .................................................................................................................................................................... 2 Epstein barr-virus and human papillomavirus co-infection in nasopharyngeal Fromcarcinoma the edito patientsr’s desk at Kenyatta National Hospital, Kenya GitongaAswani S ........................................................................................................................ JM, Anzala O, Mwang’ombe JN ................................................................................................................................................................... 3 2 AuditEffect of patternof the starkey of E.N. hearingT. diseases foundation in phasea specialist 4 intervention clinic onin speech,a rural hospital in Kenyalanguage and audition on pupils living with hearing impairment in Kochi; Machariaa quasi IM, G controlledakuo KC ............................................................................................................................. trial ................................ 3 Lawal L, Buttars -

Incidence of the Tympanic Foramen in the Population of Northeast Brazil
IJAE Vol. 123, n. 3: 241-247, 2018 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research Article - Basic and Applied Anatomy Incidence of the tympanic foramen in the population of Northeast Brazil Jalles Dantas de Lucena1, Clarice Sampaio Torres2, Patricia Karline Rojas2, Mateus Francelino Silva2, Beatriz Soares Brito2, Ana Luíza Viana Pequeno2, Paula Emanuele de Lima Bessa2, Michelle Guimarães de Lima3, Maria Clara Motta Barbosa Valente4, Geovani Garcia de Souza5, Gilberto Santos Cerqueira6,* 1 Department of Morphology, Morfofuntional Science Post-Graduation Program, Federal University of Ceara (UFC) - Brazil 2 Department of Morphology, Medical School - UFC - Brazil 3 Department of Morphology, Medical School - Federal University of Alagoas (UFAL) - Brazil 4 Department of Morphology, Medical School - State University of Health Sciences of Alagoas (UNCISAL) - Brazil 5 Integrated Colleges of Patos (FIP) – Brazil 6 Department of Morphology, Medical School, Morfofuntional Science Post-Graduation Program - UFC - Brazil Abstract The persistence of the tympanic foramen (or of Huschke) in individuals after second childhood constitutes a failure in the embryological development of the tympanic cavity. When present, it is on the anterior wall of the external acoustic meatus and is associated with important oto- logical complications of the temporomandibular joint and external acoustic meatus. To report on the incidence of tympanic foramen in adult dry skulls, belonging to the population of the Northeast of Brazil, 87 adult skulls obtained from the Human Anatomy Laboratory of 4 univer- sities of the Northeast of Brazil, without knowledge of gender, race and age were analyzed. The 174 temporal bones were examined for presence, morphology and measurements of the longi- tudinal and transverse diameter of the tympanic foramen. -
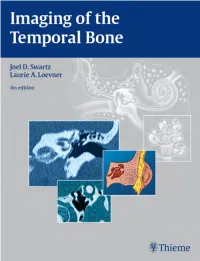
Thieme: Imaging of the Temporal Bone
fm 1/7/09 12:23 PM Page i Imaging of the Temporal Bone Fourth Edition fm 1/7/09 12:23 PM Page ii fm 1/7/09 12:23 PM Page iii Imaging of the Temporal Bone Fourth Edition Joel D. Swartz, MD President Germantown Imaging Associates Gladwyne, Pennsylvania Laurie A. Loevner, MD Professor of Radiology and Otorhinolaryngology—Head and Neck Surgery Department of Radiology Neuroradiology Section University of Pennsylvania School of Medicine and Health System Philadelphia, Pennsylvania Thieme New York • Stuttgart fm 1/7/09 12:23 PM Page iv Thieme Medical Publishers, Inc. 333 Seventh Ave. New York, NY 10001 Executive Editor: Timothy Hiscock Editorial Assistant: David Price Vice President, Production and Electronic Publishing: Anne T. Vinnicombe Production Editor: Heidi Pongratz, Maryland Composition Vice President, International Marketing and Sales: Cornelia Schulze Chief Financial Officer: Peter van Woerden President: Brian D. Scanlan Compositor: Thomson Digital Printer: The Maple-Vail Book Manufacturing Group Library of Congress Cataloging-in-Publication Data Imaging of the temporal bone / [edited by] Joel D. Swartz, Laurie A. Loevner.– 4th ed. p. ; cm. Rev. ed. of: Imaging of the temporal bone / Joel D. Swartz, H. Ric Harnsberger. 3rd ed. 1998. Includes bibliographical references and index. ISBN 978-1-58890-345-7 1. Temporal bone—Imaging. 2. Temporal bone—Diseases—Diagnosis. I. Swartz, Joel D. II. Loevner, Laurie A. [DNLM: 1. Temporal Bone—radiography. 2. Magnetic Resonance Imaging. 3. Temporal Bone—pathology. 4. Tomography, X-Ray Computed. WE 705 I31 2008] RF235.S93 2008 617'.514–dc22 2008026874 Copyright © 2009 by Thieme Medical Publishers, Inc. -

Evaluation of Foramen Tympanicum Using Cone-Beam Computed
The Journal of Craniofacial Surgery & Volume 25, Number 2, March 2014 Brief Clinical Studies he foramen tympanicum or foramen of Huschke represents a Evaluation of Foramen Tdevelopmental defect or formation in the anteroinferior aspect of the external auditory canal (EAC), posteromedial to the temporo- Tympanicum Using Cone-Beam mandibular joint (TMJ), and is an unusual condition in human skulls.1,2 Foramen tympanicum occurs during embryological de- Computed Tomography in velopment of the viscerocranial bone and was described first by Emil Huschke.3Y5 In most children, the foramen tympanicum gra- Orthodontic Malocclusions dually becomes smaller and completely closes before the age of 5 years, but it occasionally persists. An anomaly of the tympanic Nihat Akbulut, DDS, PhD,* Sebnem Kursun, DDS, PhD,Þ ring during embryogenesis could lead to an abnormal ossification of Secil Aksoy, DDS, PhD,þ Hakan Kurt, DDS, PhD,Þ the tympanic bone and to a persistent foramen tympanicum.6 Also, Kaan Orhan, DDS, PhDÞþ genetic factors may lead to delays in ossification.7 It was stated that the tympanic bone dehiscence present at the precise point of fusion Abstract: The foramen tympanicum is a persistent anatomic for- of the 2 prominences should be considered an anatomic variant only mation of the temporal bone due to a defect in ossification normal after the age of 5 years.2,8 bone physiology in neonatal or postnatal period. This study deter- Foramen tympanicum may be associated with salivary discharge mined the occurrence and location of the foramen tympanicum in a into the EAC during joint movements, or it may be associated with a Y Y Turkish sample using cone-beam computed tomography. -

Foramen of Huschke” in Seven Adult Human Crania
eISSN 1308-4038 International Journal of Anatomical Variations (2013) 6: 120–123 Case Report Variant presentations of “Foramen of Huschke” in seven adult human crania Published online July 24th, 2013 © http://www.ijav.org Phalguni SRIMANI [1] Abstract Pranab MUKHERJEE [1] So far the development of tympanic plate is concerned; gaps or ‘foramen of Huschke’ may affect its [2] surface, which bear not only anatomical significance but also clinical correlation with etiogenesis Enakshi GHOSH of different diseases. Such records though available in literature in different ethnicity and groups, Hironmoy ROY [3] but till date not available in Bengali population of India. A meticulous observation in preserved adult human crania in the Museum of Anatomy Department at the Medical College of Kolkata, Department of Anatomy, RG Kar Medical College, Kolkata seven crania showed variant presentations, detailed in the report. [1], Department of Anatomy, Burdwan Medical College, © Int J Anat Var (IJAV). 2013; 6: 120–123. Burdwan [2], Department of Anatomy, North Bengal Medical College, Darjeeling [3], INDIA. Prof. Pranab Mukherjee Department of Anatomy RG Kar Medical College Kolkata, INDIA. +91 943 4568024 [email protected] Received March 6th, 2013; accepted April 21st, 2013 Key words [foramen of Huschke] [tympanic plate] Introduction of Huschke. Shapes of such foramina were confirmed by naked Professor Emil Huschke (1797-1858), a German anatomist first eye examination with the help of divider, pointers, ruled scale described the probability of deficiency in the development and flat cardboard. of tympanic plate of temporal bone, which was named as Amongst the 53 skull studied, seven of them found to have the “Foramen of Huschke” or foramen tympanicum, which usually deficiencies of tympanic plates in form of foramen of Huschke to get apposed in adulthood [1, 2]. -

Anatomical Variants of the Temporal Bone As Depicted by Hrcts of Patients Evaluated in Two Radiology Centres in Nairobi
ANATOMICAL VARIANTS OF THE TEMPORAL BONE AS DEPICTED BY HRCTS OF PATIENTS EVALUATED IN TWO RADIOLOGY CENTRES IN NAIROBI DR. STEPHEN MUGAMBI ONYANGO H58/70092/2013 M. Med Otorhinolaryngology, Head and Neck Surgery Resident University of Nairobi A dissertation submitted in part fulfillment of the requirements for the degree of Master of Medicine in Otorhinolaryngology, Head and Neck Surgery, University of Nairobi. 2020 STUDENT’S DECLARATION I declare that this is my original work and it has not been presented for the award of any degree in any research institution or university. Dr Stephen Mugambi Onyango MBChB (UoN) Postgraduate Student- M.Med Otolaryngology, Head and Neck Surgery University of Nairobi Signature: …………………………………………..…… Date: …………………………… ii SUPERVISORS’ APPROVAL This dissertation has been submitted with our approval, in part fulfillment for the degree of master of Medicine in Otorhinolaryngology, Head and Neck Surgery, Dr Peter Mugwe MBChB (UoN), M.Med ENT, Head and Neck surgery (UoN) Consultant ENT- Head and neck surgeon and Senior Lecturer Department of Surgery (Otolaryngology, Head and Neck surgery) University of Nairobi Signature: …………………………………………..…… Date: …………………………… Dr Jane Thinwa MBChB (UoN), M.Med Diagnostic Radiology (UoN) Consultant Radiologist Kenyatta National Hospital Signature: …………………………………………..…… Date: …………………………… iii DECLARATION OF ORIGINALITY FORM (THE UNIVERSITY OF NAIROBI) Name of Student: Dr. Stephen Mugambi Onyango Registration Number: H58/70092/2013 College: Health Sciences Faculty/School: School of Medicine Department: Surgery, ENT thematic unit. Course Name: Otorhinolaryngology, Head and Neck Surgery Title of work: “ANATOMICAL VARIANTS OF THE TEMPORAL BONE AS DEPICTED BY HRCTS OF PATIENTS EVALUATED IN TWO RADIOLOGY CENTRES IN NAIROBI” Declaration 1. I understand what plagiarism is and I am aware of the University’s policy in this regard. -

Otolaryngology-Head and Neck Surgery Clinical
OTOLARYNGOLOGY HEAD &NECK SURGERY CLINICAL REFERENCE GUIDE Fifth Edition OTOLARYNGOLOGY HEAD &NECK SURGERY CLINICAL REFERENCE GUIDE Fifth Edition Raza Pasha, MD Justin S. Golub, MD, MS 5521 Ruffin Road San Diego, CA 92123 e-mail: [email protected] Website: www.pluralpublishing.com Copyright © 2018 by Plural Publishing, Inc. Typeset in 9/11 Adobe Garamond Pro by Flanagan’s Publishing Services, Inc. Printed in the United States of America by McNaughton & Gunn All rights, including that of translation, reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, recording, or otherwise, including photocopying, recording, taping, Web distribution, or information storage and retrieval systems without the prior written consent of the publisher. For permission to use material from this text, contact us by Telephone: (866) 758-7251 Fax: (888) 758-7255 e-mail: [email protected] Every attempt has been made to contact the copyright holders for material originally printed in another source. If any have been inadvertently overlooked, the publishers will gladly make the necessary arrangements at the first opportunity. NOTICE TO THE READER Care has been taken to confirm the accuracy of the indications, procedures, drug dosages, and diagnosis and remediation protocols presented in this book and to ensure that they conform to the practices of the general medical and health services communities. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. -

Surgical Anatomy of the Temporal Bone Gülay Açar and Aynur Emine Çiçekcibaşı
Chapter Surgical Anatomy of the Temporal Bone Gülay Açar and Aynur Emine Çiçekcibaşı Abstract Numerous neurological lesions and tumors of the paranasal sinuses and oral cavity may spread into the middle and posterior cranial fossae through the ana- tomical apertures. For the appropriate management of these pathologies, many extensive surgical approaches with a comprehensive overview of the anatomical landmarks are required from the maxillofacial surgery’s point of view. The surgical significance lies in the fact that iatrogenic injury to the petrous segment of the tem- poral bone including the carotid artery, sigmoid sinus, and internal jugular vein, can lead to surgical morbidity and postoperative pseudoaneurysm, vasospasm, or carotid-cavernous fistula. To simplify understanding complex anatomy of the temporal bone, we aimed to review the surgical anatomy of the temporal bone focusing on the associations between the surface landmarks and inner structures. Also, breaking down an intricate bony structure into smaller parts by compart- mental approach could ease a deep concentration and navigation. To identify the anatomic architecture of the temporal bone by using reference points, lines and compartments can be used to supplement anatomy knowledge of maxillofacial surgeons and may improve confidence by surgical trainees. Especially, this system- atic method may provide an easier way to teach and learn surgical spatial structure of the petrous pyramid in clinical applications. Keywords: maxillofacial surgery, segmentation, surface landmarks, surgical anatomy, temporal bone 1. Introduction The temporal bone is a dense complex bone that constitutes the lower lateral aspect of the skull and has complex anatomy because of the three-dimensional relationships between neurovascular structures. -
Information to Users
INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand corner and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. Higher quality 6" x 9" black and white photographic prints are available for any photographs or illustrations appearing in this copy for an additional charge. Contact UMI directly to order. UMI University Microfilms International A Bell & Howell Information Company 300 Nortfi Zeeb Road. Ann Arbor. Ml 48106-1346 USA 313/761-4700 800/521-0600 Order Number 9238180 Late Prehistoric populations in the Ohio area: Biological affinities and stress indicators Giesen, Myra Jayne, Ph.D. The Ohio State University, 1992 UMI 300 N. -

Complete Issue (PDF)
SEPTEMBER 2019 AJNR VOLUME 40 PP 1437–1607 SEPTEMBER 2019 THE JOURNAL OF DIAGNOSTIC AND VOLUME 40 INTERVENTIONAL NEURORADIOLOGY NUMBER 9 WWW.AJNR.ORG Color-mapping of 4D-CT in AV shunts CTA analysis in symptomatic subjects with bilateral intraplaque hemorrhage Improved assessment of middle ear cholesteatomas Official Journal ASNR • ASFNR • ASHNR • ASPNR • ASSR AJNRAMERICAN JOURNAL OF NEURORADIOLOGY SEPTEMBER 2019 Publication Preview at www.ajnr.org features articles released in advance of print. VOLUME 40 Visit www.ajnrblog.org to comment on AJNR content and chat with colleagues NUMBER 9 and AJNR’s News Digest at http://ajnrdigest.org to read the stories behind the WWW.AJNR.ORG latest research in neuroimaging. 1437 PERSPECTIVES S.A. Messina GENERAL CONTENTS 1438 Altered Relationship between Working Memory and Brain ADULT BRAIN FUNCTIONAL Microstructure after Mild Traumatic Brain Injury S. Chung, et al. 1445 Utility of Percentage Signal Recovery and Baseline Signal in DSC-MRI ADULT BRAIN Optimized for Relative CBV Measurement for Differentiating FUNCTIONAL Glioblastoma, Lymphoma, Metastasis, and Meningioma M.D. Lee, et al. 1451 Dynamic Contrast-Enhanced MRI in Patients with Brain Metastases ADULT BRAIN Undergoing Laser Interstitial Thermal Therapy: A Pilot Study FUNCTIONAL J.I. Traylor, et al. 1458 Molecular Subtype Classification in Lower-Grade Glioma with ADULT BRAIN FUNCTIONAL Accelerated DTI E. Aliotta, et al. 1464 Widespread Increased Diffusivity Reveals Early Cortical Degeneration in ADULT BRAIN FUNCTIONAL Huntington Disease F. Sampedro, et al. 1469 Usefulness of the Delay Alternating with Nutation for Tailored ADULT BRAIN Excitation Pulse with T1-Weighted Sampling Perfection with Application-Optimized Contrasts Using Different Flip Angle Evolution in the Detection of Cerebral Metastases: Comparison with MPRAGE Imaging D.