Invega (Paliperidone)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Paliperidone Long Acting Injection Patient Information
Paliperidone (pala-pera-done) long acting injection Patient Information - Hillmorton Hospital Pharmacy www.healthinfo.org.nz Why have I been prescribed paliperidone? Paliperidone is used to treat schizophrenia, psychosis and similar conditions. It can also be used to treat mania. A person diagnosed with schizophrenia may hear voices talking to them or about them. They may also become suspicious or paranoid. Some people also have problems with their thinking and feel that other people can read their thoughts. These are called “positive Paliperidone Injection Long Acting symptoms”. Paliperidone can help to relieve these symptoms. Many people with schizophrenia also experience “negative symptoms”. They feel tired and lacking in energy and may become quite inactive and withdrawn. Paliperidone may help relieve these symptoms as well. Paliperidone may also be prescribed for people who have had side effects such as strange movements and shaking, with older types of antipsychotics. Paliperidone is a close relative of the antipsychotic risperidone. It’s side effect profile is similar but has the advantage of being able to be given as a once a month injection. What exactly is paliperidone? Is paliperidone safe for me? It is usually safe to take paliperidone Paliperidone is one of a group of regularly as prescribed by your doctor, but medicines used to treat schizophrenia it doesn’t suit everyone. Let your doctor and similar disorders. These illnesses are know if any of the following apply to you, sometimes referred to as psychoses, as extra care may be needed: hence the name given to this group of medicines, which is the “antipsychotics”. -
Second-Generation Long-Acting Injectable Antipsychotics: a PRACTICAL GUIDE Understanding Each of These Medications’ Unique Properties Can Optimize Patient Care
Second-generation long-acting injectable antipsychotics: A PRACTICAL GUIDE Understanding each of these medications’ unique properties can optimize patient care Brittany L. Parmentier, PharmD, MPH, here are currently 7 FDA-approved second-generation long-acting BCPS, BCPP 1-7 Clinical Assistant Professor injectable antipsychotics (LAIAs). These LAIAs provide a Department of Pharmacy Practice Tunique dosage form that allows patients to receive an antipsy- The University of Texas at Tyler Fisch College of Pharmacy chotic without taking oral medications every day, or multiple times per Tyler, Texas day. This may be an appealing option for patients and clinicians, but Disclosure The author reports no financial relationships with any because there are several types of LAIAs available, it may be difficult to companies whose products are mentioned in this article, or with determine which LAIA characteristics are best for a given patient. manufacturers of competing products. Since the FDA approved the first second-generation LAIA, risperidone long-acting injectable (LAI),1 in 2003, 6 additional second-generation LAIAs have been approved: • aripiprazole LAI • aripiprazole lauroxil LAI • olanzapine pamoate LAI • paliperidone palmitate monthly injection • paliperidone palmitate 3-month LAI • risperidone LAI for subcutaneous (SQ) injection. When discussing medication options with patients, clinicians need to consider factors that are unique to each LAIA. In this article, I describe the similarities and differences among the second-generation LAIAs, and address common questions about these medications. A major potential benefit: Increased adherence One potential benefit of all LAIAs is increased medication adherence com- pared with oral antipsychotics. One meta-analysis of 21 randomized con- trolled trials (RCTs) that compared LAIAs with oral antipsychotics and Current Psychiatry GEORGE MATTEI/SCIENCE SOURCE GEORGE MATTEI/SCIENCE Vol. -

INVEGA SUSTENNA® (Paliperidone Palmitate)
INVEGA SUSTENNA® INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable suspension, for intramuscular use (paliperidone palmitate) extended-release injectable suspension, for intramuscular use --------------------------- DOSAGE FORMS AND STRENGTHS --------------------------- HIGHLIGHTS OF PRESCRIBING INFORMATION Extended-release injectable suspension: 39 mg/0.25 mL, 78 mg/0.5 mL, 117 mg/0.75 mL, These highlights do not include all the information needed to use 156 mg/mL, or 234 mg/1.5 mL (3) INVEGA SUSTENNA® safely and effectively. See full prescribing information for INVEGA SUSTENNA®. ----------------------------------- CONTRAINDICATIONS ----------------------------------- INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable Known hypersensitivity to paliperidone, risperidone, or to any excipients in suspension, for intramuscular use INVEGA SUSTENNA®. (4) Initial U.S. Approval: 2006 -----------------------------WARNINGS AND PRECAUTIONS ----------------------------- WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS • Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with WITH DEMENTIA-RELATED PSYCHOSIS Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse See full prescribing information for complete boxed warning. reactions (e.g. stroke, transient ischemic attack). (5.2) • Neuroleptic Malignant Syndrome: Manage with immediate discontinuation of Elderly patients with dementia-related psychosis treated with antipsychotic drug and close monitoring. (5.3) drugs are -

CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (Also Belong to Psychiatric Medication Category) • Codeine (In 222® Tablets, Tylenol® No
CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (also belong to psychiatric medication category) • codeine (in 222® Tablets, Tylenol® No. 1/2/3/4, Fiorinal® C, Benzodiazepines Codeine Contin, etc.) • heroin • alprazolam (Xanax®) • hydrocodone (Hycodan®, etc.) • chlordiazepoxide (Librium®) • hydromorphone (Dilaudid®) • clonazepam (Rivotril®) • methadone • diazepam (Valium®) • morphine (MS Contin®, M-Eslon®, Kadian®, Statex®, etc.) • flurazepam (Dalmane®) • oxycodone (in Oxycocet®, Percocet®, Percodan®, OxyContin®, etc.) • lorazepam (Ativan®) • pentazocine (Talwin®) • nitrazepam (Mogadon®) • oxazepam ( Serax®) Alcohol • temazepam (Restoril®) Inhalants Barbiturates • gases (e.g. nitrous oxide, “laughing gas”, chloroform, halothane, • butalbital (in Fiorinal®) ether) • secobarbital (Seconal®) • volatile solvents (benzene, toluene, xylene, acetone, naptha and hexane) Buspirone (Buspar®) • nitrites (amyl nitrite, butyl nitrite and cyclohexyl nitrite – also known as “poppers”) Non-Benzodiazepine Hypnotics (also belong to psychiatric medication category) • chloral hydrate • zopiclone (Imovane®) Other • GHB (gamma-hydroxybutyrate) • Rohypnol (flunitrazepam) CENTRAL NERVOUS SYSTEM STIMULANTS Amphetamines Caffeine • dextroamphetamine (Dexadrine®) Methelynedioxyamphetamine (MDA) • methamphetamine (“Crystal meth”) (also has hallucinogenic actions) • methylphenidate (Biphentin®, Concerta®, Ritalin®) • mixed amphetamine salts (Adderall XR®) 3,4-Methelynedioxymethamphetamine (MDMA, Ecstasy) (also has hallucinogenic actions) Cocaine/Crack -

Review of Pharmacokinetics and Pharmacogenetics in Atypical Long-Acting Injectable Antipsychotics
pharmaceutics Review Review of Pharmacokinetics and Pharmacogenetics in Atypical Long-Acting Injectable Antipsychotics Francisco José Toja-Camba 1,2,† , Nerea Gesto-Antelo 3,†, Olalla Maroñas 3,†, Eduardo Echarri Arrieta 4, Irene Zarra-Ferro 2,4, Miguel González-Barcia 2,4 , Enrique Bandín-Vilar 2,4 , Victor Mangas Sanjuan 2,5,6 , Fernando Facal 7,8 , Manuel Arrojo Romero 7, Angel Carracedo 3,9,10,* , Cristina Mondelo-García 2,4,* and Anxo Fernández-Ferreiro 2,4,* 1 Pharmacy Department, University Clinical Hospital of Ourense (SERGAS), Ramón Puga 52, 32005 Ourense, Spain; [email protected] 2 Clinical Pharmacology Group, Institute of Health Research (IDIS), Travesía da Choupana s/n, 15706 Santiago de Compostela, Spain; [email protected] (I.Z.-F.); [email protected] (M.G.-B.); [email protected] (E.B.-V.); [email protected] (V.M.S.) 3 Genomic Medicine Group, CIMUS, University of Santiago de Compostela, 15782 Santiago de Compostela, Spain; [email protected] (N.G.-A.); [email protected] (O.M.) 4 Pharmacy Department, University Clinical Hospital of Santiago de Compostela (SERGAS), Citation: Toja-Camba, F.J.; 15706 Santiago de Compostela, Spain; [email protected] Gesto-Antelo, N.; Maroñas, O.; 5 Department of Pharmacy and Pharmaceutical Technology and Parasitology, University of Valencia, Echarri Arrieta, E.; Zarra-Ferro, I.; 46100 Valencia, Spain González-Barcia, M.; Bandín-Vilar, E.; 6 Interuniversity Research Institute for Molecular Recognition and Technological Development, -

Invega Paliperidone
EMA/529190/2017 EMEA/H/C/000746 EPAR summary for the public Invega paliperidone This is a summary of the European public assessment report (EPAR) for Invega. It explains how the Agency assessed the medicine to recommend its authorisation in the EU and its conditions of use. It is not intended to provide practical advice on how to use Invega. For practical information about using Invega, patients should read the package leaflet or contact their doctor or pharmacist. What is Invega and what is it used for? Invega is an antipsychotic medicine used in adults and adolescents from 15 years of age to treat schizophrenia, a mental illness with symptoms such as disorganised thinking and speech, hallucinations (hearing or seeing things that are not there), suspiciousness and delusions (false beliefs). Invega is also used to treat adults with schizoaffective disorder. This is a condition in which the patient has episodes of elevated mood (mania) or low mood (depression) in addition to symptoms of schizophrenia. Invega contains the active substance paliperidone. How is Invega used? Invega can only be obtained with a prescription. It is available as prolonged-release tablets (3, 6, 9 and 12 mg). ‘Prolonged release’ means that paliperidone is released slowly from the tablet over a few hours. The recommended starting dose of Invega in adults is 6 mg once a day, taken in the morning; the starting dose in adolescents is 3 mg daily. Patients can take Invega either with food or between meals, but should not switch between taking it with food on one day and between meals on another. -

Guidance on the Treatment of Antipsychotic Induced Hyperprolactinaemia in Adults
Guidance on the Treatment of Antipsychotic Induced Hyperprolactinaemia in Adults Version 1 GUIDELINE NO RATIFYING COMMITTEE DRUGS AND THERAPEUTICS GROUP DATE RATIFIED April 2014 DATE AVAILABLE ON INTRANET NEXT REVIEW DATE April 2016 POLICY AUTHORS Nana Tomova, Clinical Pharmacist Dr Richard Whale, Consultant Psychiatrist In association with: Dr Gordon Caldwell, Consultant Physician, WSHT . If you require this document in an alternative format, ie easy read, large text, audio, Braille or a community language, please contact the Pharmacy Team on 01243 623349 (Text Relay calls welcome). Contents Section Title Page Number 1. Introduction 2 2. Causes of Hyperprolactinaemia 2 3. Antipsychotics Associated with 3 Hyperprolactinaemia 4. Effects of Hyperprolactinaemia 4 5. Long-term Complications of Hyperprolactinaemia 4 5.1 Sexual Development in Adolescents 4 5.2 Osteoporosis 4 5.3 Breast Cancer 5 6. Monitoring & Baseline Prolactin Levels 5 7. Management of Hyperprolactinaemia 6 8. Pharmacological Treatment of 7 Hyperprolactinaemia 8.1 Aripiprazole 7 8.2 Dopamine Agonists 8 8.3 Oestrogen and Testosterone 9 8.4 Herbal Remedies 9 9. References 10 1 1.0 Introduction Prolactin is a hormone which is secreted from the lactotroph cells in the anterior pituitary gland under the influence of dopamine, which exerts an inhibitory effect on prolactin secretion1. A reduction in dopaminergic input to the lactotroph cells results in a rapid increase in prolactin secretion. Such a reduction in dopamine can occur through the administration of antipsychotics which act on dopamine receptors (specifically D2) in the tuberoinfundibular pathway of the brain2. The administration of antipsychotic medication is responsible for the high prevalence of hyperprolactinaemia in people with severe mental illness1. -

Mental Health Medications
Mental Health Medications National Institute of Mental Health U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES UÊÊ >Ì>ÊÃÌÌÕÌiÃÊvÊi>Ì Contents Mental Health Medications ..............................................................1 What are psychiatric medications? .....................................................1 How are medications used to treat mental disorders? .......................................1 What medications are used to treat schizophrenia? ............................................2 What are the side effects? ............................................................2 How are antipsychotics taken and how do people respond to them? ...........................3 How do antipsychotics interact with other medications? ....................................3 What medications are used to treat depression? ..............................................4 What are the side effects? ............................................................4 How should antidepressants be taken? ..................................................5 Are herbal medicines used to treat depression? ...........................................5 FDA warning on antidepressants.......................................................6 What medications are used to treat bipolar disorder? . .7 Mood stabilizers ...................................................................7 Atypical antipsychotics ..............................................................7 Antidepressants ....................................................................7 What are the -

Drug Class Review Atypical Antipsychotic Drugs
Drug Class Review Atypical Antipsychotic Drugs Final Report Update 2 June 2008 Original Report Date: January 2005 Update 1 Report Date: April 2006 A literature scan of this topic is done periodically The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of or recommendation for any particular drug, use, or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Marian S. McDonagh, PharmD Kim Peterson, MS Susan Carson, MPH Benjamin Chan, MS Sujata Thakurta, MPA:HA Oregon Evidence-based Practice Center Oregon Health & Science University Mark Helfand, MD, MPH, Director Copyright © 2008 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 2 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION.............................................................................................................8 Scope and Key Questions ......................................................................................................15 METHODS .................................................................................................................... 18 Literature Search ....................................................................................................................18 Study Selection -
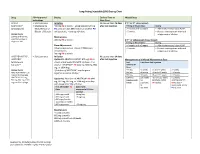
Long-Acting Injectable (LAI) Dosing Chart
Long-Acting Injectable (LAI) Dosing Chart Drug FDA-Approved Dosing Earliest Time to Missed Dose Indications Next Dose ABILIFY • Schizophrenia Initiation No sooner than 26 days If 2nd or 3rd dose missed: MAINTENA® • Maintenance 400 mg IM q month + aripiprazole 10-20 mg after last injection Timing of Missed Dose Dosing (aripiprazole)1 Monotherapy of PO daily x14 days OR if stable on another PO >4 weeks and <5 weeks • Administer missed dose ASAP. Bipolar 1 Disorder antipsychotic, + overlap x14 days >5 weeks • Restart next injection with oral Dosage Forms aripiprazole x 14 days. 300 mg and 400 mg Maintenance pre-filled syringe or 400 mg IM q month If 4th or subsequent doses missed: single-use vial Timing of Missed Dose Dosing Dose Adjustments >4 weeks and <6 weeks • Administer missed dose ASAP. Adverse reactions or known CYP2D6 poor >5 weeks • Restart next injection with oral metabolizers: aripiprazole x 14 days. 300 mg IM q month ARISTADA INITIO®, • Schizophrenia Initiation No sooner than 14 days ARISTADA® Option #1: ARISTADA INITIO® 675 mg IM x1 after last injection Management of a Missed Maintenance Dose (aripiprazole dose + aripiprazole 30 mg PO x1 dose + first Last Time Since Last Injection lauroxil)2,3 dose of *ARISTADA® IM (441 mg, 662 mg, 882 ARISTADA® mg, or 1064 mg) Dose Dosage Forms *first dose of ARISTADA® may be given 441 mg ≤6 weeks >6 and ≤7 weeks >7 weeks ARISTADA INITIO® 675 together or within 10 days* 662 mg ≤8 weeks >8 and ≤12 weeks >12 weeks mg pre-filled syringe 882 mg ≤8 weeks >8 and ≤12 weeks >12 weeks ARISTADA® 441 -

Psychopharmacologic Updates
Psychopharmacologic Updates Nimisha Gokaldas, MD Medical Director Multnomah County, Mental Health and Addiction Services Division This author has NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this presentation. History of Psychiatric drug development Mid-20th century showed saw the birth of modern psychopharmacology; the discovery of the first medicines that treated specific disorders. In 1949, lithium was tested on manic patients after John Cage noticed lithium urate salts sedating his guinea pigs. In 1950, chlorpromazine was initially used for its sedating properties, but the true benefit was really its ability to reduce hallucinations and delusions of patients with schizophrenia. In 1951, imipramine was initially developed for patients with schizophrenia, but was found to elevate mood, and became the prototype for antidepressant development. Fluoxetine was the first marketed SSRI in 1987 in the USA (Fluvoxamine was approved in 1983 in Switzerland and West Germany). History (con’t) The advent of drug discoveries in the 1950’s and 1960’s, motivated the research to understand the mechanism of actions that led to success of these medications Julius Axelrod won the Nobel Prize in 1970 for discovering neurotransmitter reuptake mechanisms. Arvid Carlsson won the Nobel Prize in 2000 for discovering that antipsychotic drugs work by blocking dopamine receptors. Antipsychotics “Golden era” of the 1950’s led to development of what we now refer to as the typical antipsychotics.