Review of Pharmacokinetics and Pharmacogenetics in Atypical Long-Acting Injectable Antipsychotics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1: Clinical Pharmacokinetics 1
1: CLINICAL PHARMACOKINETICS 1 General overview: clinical pharmacokinetics, 2 Pharmacokinetics, 4 Drug clearance (CL), 6 Volume of distribution (Vd), 8 The half-life (t½), 10 Oral availability (F), 12 Protein binding (PB), 14 pH and pharmacokinetics, 16 1 Clinical pharmacokinetics General overview General overview: clinical pharmacokinetics 1 The ultimate aim of drug therapy is to achieve effi cacy without toxicity. This involves achieving a plasma concentration (Cp) within the ‘therapeutic window’, i.e. above the min- imal effective concentration (MEC), but below the minimal toxic concentration (MTC). Clinical pharmacokinetics is about all the factors that determine variability in the Cp and its time-course. The various factors are dealt with in subsequent chapters. Ideal therapeutics: effi cacy without toxicity Minimum Toxic Concentration (MTC) Ideal dosing Minimum Effective Concentration (MEC) Drug concentration Time The graph shows a continuous IV infusion at steady state, where the dose-rate is exactly appropriate for the patient’s clearance (CL). Inappropriate dosing Dosing too high in relation to the patient’s CL – toxicity likely Minimum Toxic Concentration (MTC) Minimum Effective Concentration (MEC) Dosing too low in relation to the Drug concentration patient’s CL – drug may be ineffective Time Some reasons for variation in CL Low CL High CL Normal variation Normal variation Renal impairment Increased renal blood fl ow Genetic poor metabolism Genetic hypermetabolism Liver impairment Enzyme induction Enzyme inhibition Old age/neonate 2 General overview Clinical Pharmacokinetics Pharmacokinetic factors determining ideal therapeutics If immediate effect is needed, a loading dose (LD) must be given to achieve a desired 1 concentration. The LD is determined by the volume of distribution (Vd). -
Prediction of Clinical Transporter‐Mediated Drug–Drug Interactions
Citation: CPT Pharmacometrics Syst. Pharmacol. (2020) 9, 211–221; doi:10.1002/psp4.12505 ARTICLE Prediction of Clinical Transporter-Mediated Drug–Drug Interactions via Comeasurement of Pitavastatin and Eltrombopag in Human Hepatocyte Models Simon J. Carter1, Bhavik Chouhan2, Pradeep Sharma3 and Michael J. Chappell1,* A structurally identifiable micro-rate constant mechanistic model was used to describe the interaction between pitavastatin and eltrombopag, with improved goodness-of-fit values through comeasurement of pitavastatin and eltrombopag. Transporter association and dissociation rate constants and passive rates out of the cell were similar between pitavastatin and eltrom- bopag. Translocation into the cell through transporter-mediated uptake was six times greater for pitavastatin, leading to pronounced inhibition of pitavastatin uptake by eltrombopag. The passive rate into the cell was 91 times smaller for pitavas- tatin compared with eltrombopag. A semimechanistic physiologically-based pharmacokinetic (PBPK) model was developed to evaluate the potential for clinical drug–drug interactions (DDIs). The PBPK model predicted a twofold increase in the pita- vastatin peak blood concentration and area under the concentration-time curve in the presence of eltrombopag in simulated healthy volunteers. The use of structural identifiability supporting experimental design combined with robust micro-rate con- stant parameter estimates and a semimechanistic PBPK model gave more informed predictions of transporter-mediated DDIs. Study Highlights WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC? model fits through micro-rate constants compared with ✔ Currently, most in vitro models are not guided by macro-rate constants in human hepatocytes, with addi- structural identifiability analysis, relying on substrate-only tional information provided regarding transporter binding. -

Pharmacokinetics, Biodistribution, and Pharmacodynamics of Drug Delivery Systems
JPET Fast Forward. Published on March 5, 2019 as DOI: 10.1124/jpet.119.257113 This article has not been copyedited and formatted. The final version may differ from this version. JPET # 257113 Title: Pharmacokinetic and Pharmacodynamic Properties of Drug Delivery Systems Authors: Patrick M. Glassman, Vladimir R. Muzykantov Affiliation: Department of Systems Pharmacology and Translational Therapeutics, Perelman School of Medicine, University of Pennsylvania Address: 3400 Civic Center Boulevard, Bldg 421, Philadelphia, Pennsylvania 19104-5158, United States Downloaded from jpet.aspetjournals.org at ASPET Journals on September 24, 2021 1 JPET Fast Forward. Published on March 5, 2019 as DOI: 10.1124/jpet.119.257113 This article has not been copyedited and formatted. The final version may differ from this version. JPET # 257113 Running Title: PK/PD Properties of Drug Delivery Systems Corresponding Authors: Vladimir R. Muzykantov ([email protected], (215) 898-9823) and Patrick M. Glassman ([email protected]) # of Text Pages: 22 # of Tables: 2 # of Figures: 4 Word Count – Abstract: 144 Word Count – Introduction: 350 Word Count – Discussion: N/A Downloaded from Non-Standard Abbreviations: Absorption, Distribution, Metabolism, and Elimination (ADME) Biodistribution (BD) Drug Delivery Systems (DDSs) Enhanced Permeability & Retention (EPR) jpet.aspetjournals.org Gastrointestinal (GI) Intravenously (IV) Neonatal Fc Receptor (FcRn) Monoclonal Antibody (mAb) Reticuloendothelial System (RES) at ASPET Journals on September 24, 2021 Pharmacodynamics (PD) Pharmacokinetics (PK) Physiologically-Based Pharmacokinetic (PBPK) Subcutaneously (SC) Target-Mediated Drug Disposition (TMDD) Recommended Section: Drug Discovery and Translational Medicine 2 JPET Fast Forward. Published on March 5, 2019 as DOI: 10.1124/jpet.119.257113 This article has not been copyedited and formatted. -

Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development
Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development Gerlie Gieser, Ph.D. Office of Clinical Pharmacology, Div. IV Objectives • Outline the Phase 1 studies conducted to characterize the Clinical Pharmacology of a drug; describe important design elements of and the information gained from these studies. • List the Clinical Pharmacology characteristics of an Ideal Drug • Describe how the Clinical Pharmacology information from Phase 1 can help design Phase 2/3 trials • Discuss the timing of Clinical Pharmacology studies during drug development, and provide examples of how the information generated could impact the overall clinical development plan and product labeling. Phase 1 of Drug Development CLINICAL DEVELOPMENT RESEARCH PRE POST AND CLINICAL APPROVAL 1 DISCOVERY DEVELOPMENT 2 3 PHASE e e e s s s a a a h h h P P P Clinical Pharmacology Studies Initial IND (first in human) NDA/BLA SUBMISSION Phase 1 – studies designed mainly to investigate the safety/tolerability (if possible, identify MTD), pharmacokinetics and pharmacodynamics of an investigational drug in humans Clinical Pharmacology • Study of the Pharmacokinetics (PK) and Pharmacodynamics (PD) of the drug in humans – PK: what the body does to the drug (Absorption, Distribution, Metabolism, Excretion) – PD: what the drug does to the body • PK and PD profiles of the drug are influenced by physicochemical properties of the drug, product/formulation, administration route, patient’s intrinsic and extrinsic factors (e.g., organ dysfunction, diseases, concomitant medications, -

624.Full.Pdf
1521-009X/44/5/624–633$25.00 http://dx.doi.org/10.1124/dmd.115.068932 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:624–633, May 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Development of a Rat Plasma and Brain Extracellular Fluid Pharmacokinetic Model for Bupropion and Hydroxybupropion Based on Microdialysis Sampling, and Application to Predict Human Brain Concentrations Thomas I.F.H. Cremers, Gunnar Flik, Joost H.A. Folgering, Hans Rollema, and Robert E. Stratford, Jr. Brains On-Line BV, Groningen, The Netherlands (T.I.F.H.C., G.F. J.H.A.F.); Rollema Biomedical Consulting, Mystic, Connecticut (H.R.); and Division of Pharmaceutical Sciences, Mylan School of Pharmacy, Duquesne University, Pittsburgh, Pennsylvania (R.E.S.) Received December 11, 2015; accepted February 24, 2016 Downloaded from ABSTRACT Administration of bupropion [(6)-2-(tert-butylamino)-1-(3-chlorophenyl) concentration ratio at early time points was observed with propan-1-one] and its preformed active metabolite, hydroxybupropion bupropion; this was modeled as a time-dependent uptake clear- [(6)-1-(3-chlorophenyl)-2-[(1-hydroxy-2-methyl-2-propanyl)amino]- ance of the drug across the blood–brain barrier. Translation of the 1-propanone], to rats with measurement of unbound concentrations model was used to predict bupropion and hydroxybupropion dmd.aspetjournals.org by quantitative microdialysis sampling of plasma and brain extra- exposure in human brain extracellular fluid after twice-daily cellular fluid was used to develop a compartmental pharmacoki- administration of 150 mg bupropion. Predicted concentrations netics model to describe the blood–brain barrier transport of both indicate that preferential inhibition of the dopamine and norepi- substances. -

A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
A synbiotic mixture augmented the efficacy of doxepin, venlafaxine, and fluvoxamine in mice model of depression Azadeh Mesripour1, Andiya Meshkati1, Valiolah Hajhashemi2 1Department of Pharmacology and Toxicology, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. 2‐ Isfahan Pharmaceutical Sciences Research Center, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. ABSTRACT Objective: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals, may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicineproof in order to augment the efficacy of therapeutic doses of antidepressant drugs seems to be very important. Therefore the effect of adding a synbiotic cocktail in drinking water was assessed in mice model of despair following administrating three antidepressant drugs belonging to different classes. Methods: The marble burring test (MBT), and forced swimming test (FST) were used as animal model of obsessive behavior and despair. The synbiotic cocktail was administered in mice drinking water (6.25×106 CFU) for 14 days and the tests were performed on the days 7 and 14 thirty minutes after injecting the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg). Results: After 7 days of the synbiotic ingestion immobility time decreased in FST for doxepin (92 sec ± 5.5) and venlafaxine (17.3 sec ± 2.5) compared to their control group (drinking water) but fluvoxamine could decrease immobility time after 14 days of ingesting the synbiotic (70 sec ± 7.5). -
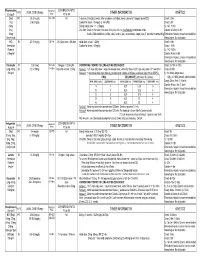
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

A Primer on Pharmacology
A primer on pharmacology Universidade do Algarve Faro 2017 by Ferdi Engels, Ph.D. 1 2 1 3 Utrecht university campus ‘de Uithof’ Dept. of Pharmaceutical Sciences Division of Pharmacology 4 2 Bachelor and master education Ferdi Engels, PhD ‐ Associate professor of pharmacology ‐ Director of Undergraduate School of Science PhD training Research expertise 5 for today 1. Understand the main concepts of pharmacokinetics Main concept 2. Be able to apply this new knowledge 6 3 Pharmacology is about drugs………. Drugs = chemicals that alter physiological processes in the body for treatment, prevention, or cure of diseases input output (administration of the drug) (biological response) ‐ dose ‐ no effect ‐ frequency of administration ‐ beneficial effects ‐ route of administration ‐ adverse / toxic effects onset, intensity, and duration of therapeutic effects 7 Pharmacology is about drugs………. Drugs = chemicals that alter physiological processes in the body for treatment, prevention, or cure of diseases What does the body do to the drug? pharmacokinetics What does the drug do to the body? pharmacodynamics 8 4 Thursday, June 15 Lecture on topic 1 Workshop on topic 1 Friday, June 16 Lecture on topic 2 Workshop on topic 2 Course Topic 1 Course Topic 2 9 Rosenbaum ‐ Basic pharmacokinetics and pharmacodynamics: an integrated textbook and computer simulations, 1st ed. (2011) input output (administration of the drug) (biological response) ‐ dose ‐ no effect ‐ frequency of administration ‐ beneficial effects ‐ route of administration ‐ adverse / toxic effects -

Selective Knockout of the Vesicular Monoamine Transporter 2 (Vmat2)
ORIGINAL RESEARCH published: 09 November 2020 doi: 10.3389/fnbeh.2020.578443 Selective Knockout of the Vesicular Monoamine Transporter 2 (Vmat2) Gene in Calbindin2/Calretinin-Positive Neurons Results in Profound Changes in Behavior and Response to Drugs of Abuse 1 1† 2 1 Edited by: Niclas König , Zisis Bimpisidis , Sylvie Dumas and Åsa Wallén-Mackenzie * Nuno Sousa, 1Unit of Comparative Physiology, Department of Organismal Biology, Uppsala University, Uppsala, Sweden, 2Oramacell, University of Minho, Portugal Paris, France Reviewed by: Ali Salahpour, University of Toronto, Canada The vesicular monoamine transporter 2 (VMAT2) has a range of functions in the Louis-Eric Trudeau, central nervous system, from sequestering toxins to providing conditions for the quantal Université de Montréal, Canada release of monoaminergic neurotransmitters. Monoamine signaling regulates diverse *Correspondence: functions from arousal to mood, movement, and motivation, and dysregulation of Åsa Wallén-Mackenzie [email protected] VMAT2 function is implicated in various neuropsychiatric diseases. While all monoamine- releasing neurons express the Vmat2 gene, only a subset is positive for the calcium- †Present address: Zisis Bimpisidis, binding protein Calbindin 2 (Calb2; aka Calretinin, 29 kDa Calbindin). We recently Department of Neuroscience and showed that about half of the dopamine neurons in the mouse midbrain are positive Brain Technologies, Istitito Italiano di Tecnologia, Genova, Italy for Calb2 and that Calb2 is an early developmental marker of -

Paliperidone Long Acting Injection Patient Information
Paliperidone (pala-pera-done) long acting injection Patient Information - Hillmorton Hospital Pharmacy www.healthinfo.org.nz Why have I been prescribed paliperidone? Paliperidone is used to treat schizophrenia, psychosis and similar conditions. It can also be used to treat mania. A person diagnosed with schizophrenia may hear voices talking to them or about them. They may also become suspicious or paranoid. Some people also have problems with their thinking and feel that other people can read their thoughts. These are called “positive Paliperidone Injection Long Acting symptoms”. Paliperidone can help to relieve these symptoms. Many people with schizophrenia also experience “negative symptoms”. They feel tired and lacking in energy and may become quite inactive and withdrawn. Paliperidone may help relieve these symptoms as well. Paliperidone may also be prescribed for people who have had side effects such as strange movements and shaking, with older types of antipsychotics. Paliperidone is a close relative of the antipsychotic risperidone. It’s side effect profile is similar but has the advantage of being able to be given as a once a month injection. What exactly is paliperidone? Is paliperidone safe for me? It is usually safe to take paliperidone Paliperidone is one of a group of regularly as prescribed by your doctor, but medicines used to treat schizophrenia it doesn’t suit everyone. Let your doctor and similar disorders. These illnesses are know if any of the following apply to you, sometimes referred to as psychoses, as extra care may be needed: hence the name given to this group of medicines, which is the “antipsychotics”. -
A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
Turk J Pharm Sci 2020;17(3):293-298 DOI: 10.4274/tjps.galenos.2019.94210 ORIGINAL ARTICLE A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine, and Fluvoxamine in a Mouse Model of Depression Sinbiyotik Karışım, Fare Depresyon Modelinde Doksepin, Venlafaksin ve Fluvoksaminin Etkinliğini Artırdı Azadeh MESRIPOUR1*, Andiya MESHKATI1, Valiollah HAJHASHEMI2 1Isfahan University of Medical Sciences, School of Pharmacy and Pharmaceutical Sciences, Department of Pharmacology and Toxicology, Isfahan, Iran 2Isfahan University of Medical Sciences, School of Pharmacy and Pharmaceutical Sciences, Isfahan Pharmaceutical Sciences Research Center, Isfahan, Iran ABSTRACT Objectives: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicine in order to augment the efficacy of therapeutic doses of antidepressant drugs appears to be very important. Therefore, the effect of adding a synbiotic mixture to drinking water was assessed in a mouse model of depression following the administration of three antidepressant drugs belonging to different classes. Materials and Methods: The marble burying test (MBT) and forced swimming test (FST) were used as animal models of obsessive behavior and despair. The synbiotic mixture was administered to the mice’s drinking water (6.25x106 CFU) for 14 days and the tests were performed 30 min after the injection of the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg) on days 7 and 14. Results: After 7 days of ingestion of the synbiotic mixture, immobility time decreased in the FST for doxepin (92±5.5 s) and venlafaxine (17.3±2.5 s) compared to the control group (drinking water), but fluvoxamine decreased immobility time after 14 days of ingestion of the synbiotic mixture (70±7.5 s). -

Ecstasy and the Concomitant Use of Pharmaceuticals
J.Copeland, P. Dillon & M. Gascoigne Ecstasy and the Concomitant Use of Pharmaceuticals NDARC Technical Report No. 201 ECSTASY AND THE CONCOMITANT USE OF PHARMACEUTICALS Jan Copeland (PhD), Paul Dillon & Michael Gascoigne Technical Report Number 201 ISBN: 1 877027 92 8 ©National Drug and Alcohol Research Centre, University of New South Wales, Sydney, 2004 This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use or use within your organisation. All other rights are reserved. Requests and enquiries concerning reproduction and rights should be addressed to the information manager, National Drug and Alcohol Research Centre, University of New South Wales, Sydney, NSW 2052, Australia. 2 ACKNOWLEDGEMENT This study and report was funded by the Australian Government Department of Health and Ageing’s National Illicit Drug Strategy. It was conducted concurrently with a study of aspects of information seeking among ecstasy users and there is some replication of the data presented on demographic characteristics and perception of ecstasy related harms in this Technical Report and Technical Report Number 202. 3 TABLE OF CONTENTS ACKNOWLEDGEMENT 3 TABLE OF CONTENTS 4 TABLE OF TABLES 5 EXECUTIVE SUMMARY 6 INTRODUCTION 7 Anti-depressant medication 8 5-hydroxytryptophan 9 Attention Deficit Hyperactivity Disorder 11 Sildenafil Citrate 12 Benzodiazepines 13 Study Ains 14 METHOD 15 Participants 15 Procedure 15 Measures 15 RESULTS 17 Demographics