Long-Acting Injectable (LAI) Dosing Chart
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aripiprazole As an Adjunct to Anti-Depressants for Major Depressive Disorder: Clinical Effectiveness, Cost-Effectiveness, and Guidelines
TITLE: Aripiprazole as an Adjunct to Anti-Depressants for Major Depressive Disorder: Clinical Effectiveness, Cost-Effectiveness, and Guidelines DATE: 04 May 2016 RESEARCH QUESTIONS 1. What is the clinical efficacy of aripiprazole as an adjunct to antidepressants for the treatment of patients with major depressive disorder who have had an inadequate response to prior antidepressant treatments? 2. What is the cost-effectiveness of aripiprazole as an adjunct to antidepressants for the treatment of patients with major depressive disorder who have had an inadequate response to prior antidepressant treatments? 3. What are the evidence-based guidelines for the use of aripiprazole for the treatment of patients with major depressive disorder who have had an inadequate response to prior antidepressant treatments? KEY FINDINGS Three systematic reviews with meta-analyses, two randomized controlled trials, and two evidence-based guidelines were identified regarding the use of aripiprazole as an adjunct to antidepressants for the treatment of patients with major depressive disorder who have had an inadequate response to prior antidepressant treatments. METHODS A limited literature search was conducted on key resources including PubMed, Ovid PsychINFO, Ovid Embase, The Cochrane Library, University of York Centre for Reviews and Dissemination (CRD) databases, Canadian and major international health technology agencies, as well as a focused Internet search. No methodological filters were used to limit retrieval by study type. Where possible, retrieval was limited to the human population. The search was also limited to English language documents published between January 1, 2014 and April 29, 2016. Disclaimer: The Rapid Response Service is an information service for those involved in planning and providing health care in Canada. -

HALDOL Brand of Haloperidol Injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia
HALDOL® brand of haloperidol injection (For Immediate Release) WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. HALDOL Injection is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS). DESCRIPTION Haloperidol is the first of the butyrophenone series of major antipsychotics. The chemical designation is 4-[4-(p-chlorophenyl)-4-hydroxypiperidino] 4’-fluorobutyrophenone and it has the following structural formula: HALDOL (haloperidol) is available as a sterile parenteral form for intramuscular injection. The injection provides 5 mg haloperidol (as the lactate) and lactic acid for pH adjustment between 3.0 – 3.6. -

Download Executive Summary
Comparative Effectiveness Review Number 43 Effective Health Care Program Off-Label Use of Atypical Antipsychotics: An Update Executive Summary Background Effective Health Care Program Antipsychotics medications are approved The Effective Health Care Program by the U.S. Food and Drug Administration was initiated in 2005 to provide valid (FDA) for treatment of schizophrenia and evidence about the comparative bipolar disorder. These medications are effectiveness of different medical commonly divided into two classes, interventions. The object is to help reflecting two waves of historical consumers, health care providers, and development: the conventional others in making informed choices antipsychotics and the atypical. The among treatment alternatives. Through conventional antipsychotics served as the its Comparative Effectiveness Reviews, first successful pharmacologic treatment the program supports systematic for primary psychotic disorders such as appraisals of existing scientific schizophrenia. Having been widely used evidence regarding treatments for for decades, the conventional high-priority health conditions. It also antipsychotics also produced various side promotes and generates new scientific effects requiring additional medications, evidence by identifying gaps in which spurred the development of the existing scientific evidence and atypical antipsychotics. supporting new research. The program Currently, nine atypical antipsychotic drugs puts special emphasis on translating have been approved by FDA: aripiprazole, findings into a variety of useful asenapine, clozapine, iloperidone, formats for different stakeholders, olanzapine, paliperidone, quetiapine, including consumers. risperidone, and ziprasidone. These drugs The full report and this summary are have been used off-label (i.e., for available at www.effectivehealthcare. indications not approved by FDA) for the ahrq.gov/reports/final.cfm. treatment of various psychiatric conditions. -
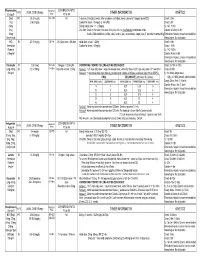
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Appendix 18: References to Studies from the Previous Guideline
Appendix 18: References to studies from the previous guideline This appendix contains references to the studies from the previous guideline, as they appeared in that guideline. References to studies added to the guideline update are in Appendix 17a-d. Contents Service references…………………………………………………………………..1 Psychology references……………………………………………………………..15 Pharmacology references………………………………………………………….28 Service references Araya2003 {published data only} Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, Simon G, Peters TJ. Treating depression in primary care in low-income women in Santiago, Chile: A randomised controlled trial. Lancet 2003;361(9362):995-1000. Arthur2002 {published data only} Arthur AJ, Jagger C, Lindesay J, Matthews RJ. Evaluating a mental health assessment for older people with depressive symptoms in general practice: a randomised controlled trial. British Journal of General Practice 2002;52(476):202-207. Austin-Los Angeles Austin NK, Liberman RP, King LW, DeRisi WJ. A comparative evaluation of two day hospitals. Goal attainment scaling of behaviour therapy vs. milieu therapy. Journal of Nervous and Mental Disease 1976;163:253-62. Azim-Alberta Azim HF, Weiden TD, Ratcliffe WD, Nutter RW, Dyck RJ, Howarth BG. Current utilization of day hospitalization. Canadian Psychiatric Association Journal 1978;23:557-66 Baker2001 {published data only} Baker R, Reddish S, Robertson N, Hearnshaw H, Jones B. Randomised controlled trial of tailored strategies to implement guidelines for the management of patients with depression in general practice. British Journal of General Practice 2001;51:737-741. Barkley-Ontario Barkley AL, Fagen K, Lawson JS. Day care: can it prevent readmission to a psychiatric hospital? Psychiatric Journal of the University of Ottawa 1989;14:536-41. -

Paliperidone Long Acting Injection Patient Information
Paliperidone (pala-pera-done) long acting injection Patient Information - Hillmorton Hospital Pharmacy www.healthinfo.org.nz Why have I been prescribed paliperidone? Paliperidone is used to treat schizophrenia, psychosis and similar conditions. It can also be used to treat mania. A person diagnosed with schizophrenia may hear voices talking to them or about them. They may also become suspicious or paranoid. Some people also have problems with their thinking and feel that other people can read their thoughts. These are called “positive Paliperidone Injection Long Acting symptoms”. Paliperidone can help to relieve these symptoms. Many people with schizophrenia also experience “negative symptoms”. They feel tired and lacking in energy and may become quite inactive and withdrawn. Paliperidone may help relieve these symptoms as well. Paliperidone may also be prescribed for people who have had side effects such as strange movements and shaking, with older types of antipsychotics. Paliperidone is a close relative of the antipsychotic risperidone. It’s side effect profile is similar but has the advantage of being able to be given as a once a month injection. What exactly is paliperidone? Is paliperidone safe for me? It is usually safe to take paliperidone Paliperidone is one of a group of regularly as prescribed by your doctor, but medicines used to treat schizophrenia it doesn’t suit everyone. Let your doctor and similar disorders. These illnesses are know if any of the following apply to you, sometimes referred to as psychoses, as extra care may be needed: hence the name given to this group of medicines, which is the “antipsychotics”. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -
Second-Generation Long-Acting Injectable Antipsychotics: a PRACTICAL GUIDE Understanding Each of These Medications’ Unique Properties Can Optimize Patient Care
Second-generation long-acting injectable antipsychotics: A PRACTICAL GUIDE Understanding each of these medications’ unique properties can optimize patient care Brittany L. Parmentier, PharmD, MPH, here are currently 7 FDA-approved second-generation long-acting BCPS, BCPP 1-7 Clinical Assistant Professor injectable antipsychotics (LAIAs). These LAIAs provide a Department of Pharmacy Practice Tunique dosage form that allows patients to receive an antipsy- The University of Texas at Tyler Fisch College of Pharmacy chotic without taking oral medications every day, or multiple times per Tyler, Texas day. This may be an appealing option for patients and clinicians, but Disclosure The author reports no financial relationships with any because there are several types of LAIAs available, it may be difficult to companies whose products are mentioned in this article, or with determine which LAIA characteristics are best for a given patient. manufacturers of competing products. Since the FDA approved the first second-generation LAIA, risperidone long-acting injectable (LAI),1 in 2003, 6 additional second-generation LAIAs have been approved: • aripiprazole LAI • aripiprazole lauroxil LAI • olanzapine pamoate LAI • paliperidone palmitate monthly injection • paliperidone palmitate 3-month LAI • risperidone LAI for subcutaneous (SQ) injection. When discussing medication options with patients, clinicians need to consider factors that are unique to each LAIA. In this article, I describe the similarities and differences among the second-generation LAIAs, and address common questions about these medications. A major potential benefit: Increased adherence One potential benefit of all LAIAs is increased medication adherence com- pared with oral antipsychotics. One meta-analysis of 21 randomized con- trolled trials (RCTs) that compared LAIAs with oral antipsychotics and Current Psychiatry GEORGE MATTEI/SCIENCE SOURCE GEORGE MATTEI/SCIENCE Vol. -

INVEGA SUSTENNA® (Paliperidone Palmitate)
INVEGA SUSTENNA® INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable suspension, for intramuscular use (paliperidone palmitate) extended-release injectable suspension, for intramuscular use --------------------------- DOSAGE FORMS AND STRENGTHS --------------------------- HIGHLIGHTS OF PRESCRIBING INFORMATION Extended-release injectable suspension: 39 mg/0.25 mL, 78 mg/0.5 mL, 117 mg/0.75 mL, These highlights do not include all the information needed to use 156 mg/mL, or 234 mg/1.5 mL (3) INVEGA SUSTENNA® safely and effectively. See full prescribing information for INVEGA SUSTENNA®. ----------------------------------- CONTRAINDICATIONS ----------------------------------- INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable Known hypersensitivity to paliperidone, risperidone, or to any excipients in suspension, for intramuscular use INVEGA SUSTENNA®. (4) Initial U.S. Approval: 2006 -----------------------------WARNINGS AND PRECAUTIONS ----------------------------- WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS • Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with WITH DEMENTIA-RELATED PSYCHOSIS Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse See full prescribing information for complete boxed warning. reactions (e.g. stroke, transient ischemic attack). (5.2) • Neuroleptic Malignant Syndrome: Manage with immediate discontinuation of Elderly patients with dementia-related psychosis treated with antipsychotic drug and close monitoring. (5.3) drugs are -

HALDOL Decanoate 50 (Haloperidol)
HALDOL® Decanoate 50 (haloperidol) HALDOL® Decanoate 100 (haloperidol) For IM Injection Only WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. HALDOL Decanoate is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS). DESCRIPTION Haloperidol decanoate is the decanoate ester of the butyrophenone, HALDOL (haloperidol). It has a markedly extended duration of effect. It is available in sesame oil in sterile form for intramuscular (IM) injection. The structural formula of haloperidol decanoate, 4-(4-chlorophenyl)-1-[4-(4-fluorophenyl)-4-oxobutyl]-4 piperidinyl decanoate, is: Haloperidol decanoate is almost insoluble in water (0.01 mg/mL), but is soluble in most organic solvents. -

Schizophrenia Paper
The new england journal of medicine review article drug therapy Alastair J.J. Wood, M.D., Editor Schizophrenia Robert Freedman, M.D. From the Institute for Children’s Mental chizophrenia is a chronic, debilitating psychotic mental dis- Disorders, University of Colorado and the order that affects about 1 percent of people. A new generation of medications Veterans Affairs Medical Center, Denver. s Address reprint requests to Dr. Freedman and recent developments in neuropathology, brain imaging, and molecular ge- at the Department of Psychiatry, C-268-71, netics have led to a greater understanding of the pathophysiology of schizophrenia and University of Colorado Health Sciences to improved treatment. Nonetheless, it remains an enigmatic illness that places a sub- Center, Denver CO 80262, or at robert. [email protected]. stantial burden on patients, their families, and society. N Engl J Med 2003;349:1738-49. clinical characteristics Copyright © 2003 Massachusetts Medical Society. Schizophrenia has varied and ominous symptoms that generally begin in late adoles- cence or early adulthood and usually continue throughout life.1 Most patients have a history of behavioral dysfunction — primarily social and learning difficulties.2 Diagnos- tic features of schizophrenia include auditory hallucinations (generally voices that con- verse with or about the patient) and delusions (often the paranoid belief that external forces are conspiring against the patient). Patients may have some insight that the voices are internal thoughts and that the delusions cannot possibly be true, but these phenom- ena remain persistent and troubling. In addition to these overt psychotic, or “positive,” symptoms, various deficits, or “negative” symptoms, occur, including an inability to pay attention, the loss of a sense of pleasure, the loss of will or drive, disorganization or im- poverishment of thoughts and speech, flattening of affect, and social withdrawal (Ta- ble 1).