Self-Deliverance and Bridge Traffic “Let's Talk
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
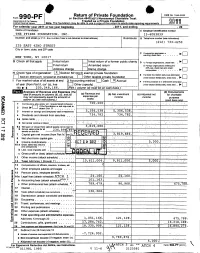
Return of Private Foundation CT' 10 201Z '
Return of Private Foundation OMB No 1545-0052 Form 990 -PF or Section 4947(a)(1) Nonexempt Charitable Trust Department of the Treasury Treated as a Private Foundation Internal Revenue Service Note. The foundation may be able to use a copy of this return to satisfy state reporting requirem M11 For calendar year 20 11 or tax year beainnina . 2011. and ending . 20 Name of foundation A Employer Identification number THE PFIZER FOUNDATION, INC. 13-6083839 Number and street (or P 0 box number If mail is not delivered to street address ) Room/suite B Telephone number (see instructions) (212) 733-4250 235 EAST 42ND STREET City or town, state, and ZIP code q C If exemption application is ► pending, check here • • • • • . NEW YORK, NY 10017 G Check all that apply Initial return Initial return of a former public charity D q 1 . Foreign organizations , check here . ► Final return Amended return 2. Foreign organizations meeting the 85% test, check here and attach Address chang e Name change computation . 10. H Check type of organization' X Section 501( exempt private foundation E If private foundation status was terminated Section 4947 ( a)( 1 ) nonexem pt charitable trust Other taxable p rivate foundation q 19 under section 507(b )( 1)(A) , check here . ► Fair market value of all assets at end J Accounting method Cash X Accrual F If the foundation is in a60-month termination of year (from Part Il, col (c), line Other ( specify ) ---- -- ------ ---------- under section 507(b)(1)(B),check here , q 205, 8, 166. 16) ► $ 04 (Part 1, column (d) must be on cash basis) Analysis of Revenue and Expenses (The (d) Disbursements total of amounts in columns (b), (c), and (d) (a) Revenue and (b) Net investment (c) Adjusted net for charitable may not necessanly equal the amounts in expenses per income income Y books purposes C^7 column (a) (see instructions) .) (cash basis only) I Contribution s odt s, grants etc. -
FENA Conversation with Fran
FINAL EXIT NETWORK VOL 18 • NO 1 WINTER, JAN/FEB 2019 CONTENTS TTHEHE TIME TO IMPROVE OREGON-STYLE LAWS? .........3 GOODGOOD DEMENTIA ADVANCE DEATHDEATH DIRECTIVES ...........................5 FISCAL YEAR REPORT ............9 SOCIETYSOCIETY AMERICANS ACCEPT FEN EUTHANASIA ..................... 11 A Conversation With Fran By Michael James, FEN Life Member enior Guide Fran Schindler’s voice was raspy after five days of protesting in Washington, DC, but this remarkable 79- Q: year-old’sS enthusiasm for FEN and life in general was loud and clear. “The privilege of someone being What’s going to willing to have me with them when they die, when I happen to you? only just sit with them, is the most meaningful thing I have ever done.” In the late 1980s, Fran faced a series of daunt- ing issues: a brain tumor, divorce, and mysterious A. symptoms which mimicked ALS. She acknowledg- es she became obsessed with finding ways to kill I will get dead. herself during those dark days. Eventually she heard Faye Girsh lecture about FEN. She quickly signed up for training and got her FEN membership card in November 2006. Twelve years later she estimates FRAN continued on page 2 Renew your membership online: www.finalexitnetwork.org FRAN continued from page 1 she’s been present for over 70 individuals who have taken their lives using FEN protocol. “At the FEN training class I discovered a major benefit of being a “Start doing FEN member. I looked at the trainers and my fellow classmates—people who didn’t know me—and real- what you want ized that if I needed them they would be there for me. -

NOW Is Time to Address Dementia
The Human Right To A Death With Dignity Special Edition FEN responds in hour of crises VOL 19 • NO 2 SPRING 2020 NOW is time to address dementia Final Exit Network has created surrounding the explosion in a new Advance Directive designed Alzheimer’s and other forms of to prevent dying people from being dementia, because no state that offers force fed against their wishes – Medical Aid in Dying accommodates even if suffering from dementia. patients who are not “of sound mind” What’s more, FEN will go to court when it is time to receive assistance. in an effort to set a legal precedent Now there is a second, more ensuring that VSED (Voluntarily pressing crisis: COVID-19. The Stopping Eating and Drinking) is specter of a ventilator is now reality always available to those who sign for many of us who were already the Supplemental Advance Directive concerned about how we would die. for Dementia Care. FEN is stepping up in this time This document, and the drive to of dual crises, and this edition of the make it legally binding, has been magazine is keenly focused on on our agenda for some time. We what we all need to know. recognized the growing crisis – Brian Ruder, FEN President Life (and death) in the time of COVID-19 By Lowrey Brown words apply equally well when applied to laws FEN Client Services Director and social customs that would rob so many of The title is hardly original wordplay at the right to shape how their life stories end. -

State Court Rewriting of Overbroad Statutes
University of Pennsylvania Carey Law School Penn Law: Legal Scholarship Repository Prize Winning Papers Student Papers 2017 State Court Rewriting of Overbroad Statutes David Schneyer Follow this and additional works at: https://scholarship.law.upenn.edu/prize_papers Repository Citation Schneyer, David, "State Court Rewriting of Overbroad Statutes" (2017). Prize Winning Papers. 11. https://scholarship.law.upenn.edu/prize_papers/11 This Prize Paper is brought to you for free and open access by the Student Papers at Penn Law: Legal Scholarship Repository. It has been accepted for inclusion in Prize Winning Papers by an authorized administrator of Penn Law: Legal Scholarship Repository. For more information, please contact [email protected]. David Schneyer First Amendment Seminar Professor Seth Kreimer State Court Rewriting of Overbroad Statutes I. Introduction: Overbreadth and the Problem of Federalism ............................................. 2 II. State Court Narrowing of Overbroad Statutes: a 50-State Survey .............................. 7 A. States that Rewrite Overbroad Statutes .......................................................................... 10 1. California ........................................................................................................................ 11 2. Massachusetts ................................................................................................................. 16 3. Other States that Rewrite Overbroad Statutes. .............................................................. -

QUIZ: Are You Ready to Die?
QUIZ: Are you ready to die? 1. Do you have an irreversible physical illness or condition -- one that will not get better? __Yes __No 2. Do you suffer unbearably most of the time? __Yes __No 3. Will you lose any semblance of who you are as a person as your illness progresses? __Yes __No 4. If you didn’t have this illness, would you want to live? __Yes __No 5. Have you explored all alternatives to ending your life, for example, further treatment, comfort care? __Yes __No 6. Have you discussed your thoughts about dying with those closest to you? __Yes __No 7. Are people you love and respect sympathetic with your wishes? __Yes __No 8. Are your ideas about dying now consistent with your religious and ethical values? __Yes __No 9. Do you have a plan that follows authoritative information from respected sources to accomplish a peaceful and dignified death? __Yes __No 10. Do you have a plan that will not jeopardize or traumatize anyone else? __Yes __No 11. Have you discussed with an authoritative source what other choices you have to end your life besides the plan you have? __Yes __No 12. Will someone be with you so you do not die alone? __Yes __No 13. Have you explored the Final Exit Network program? __Yes __No __________________ If you have answered Yes to all 13 questions you might be a candidate for an assisted, hastened death. If you have answered No to any of these questions, you should not act to hasten your death until you have explored the possibilities further. -

American Atheists 2019 National Convention
AMERICAN ATHEISTS 2019 NATIONAL CONVENTION APRIL 19–21, 2019 Hilton Netherland Plaza Hotel Cincinnati, OH EVERYDAY ATHEISM EXTRAORDINARY ACTIVISM FROM EVERYDAY PEOPLE CONFERENCE AGENDA YOUR NAME Table of Contents Convention Site Layout ......................................................2 Exhibitors and Guests ..........................................................3 Service Project ..........................................................................4 Recording Policy ......................................................................4 Meet Your Emcee ...................................................................5 Convention Schedule Thursday ..............................................................................5 Friday ......................................................................................6 Saturday ...............................................................................8 Sunday ..................................................................................10 Convention Speakers ...........................................................11 God Awful Movies LIVE! .....................................................17 Saturday Main Stage ............................................................18 Saturday Workshops ............................................................19 Full Code of Conduct ...........................................................23 Join the Conversation American Atheists @AmericanAtheist #AACon2019 Convention Layout Fourth Floor Freight Rosewood Elevator Rosewood -

In Canada Market Research Done? Medical Problems
ISSN #1481-7314 Vol. 8, No. 3 Jul. - Sep. 2006 A QUARTERLY NEWSLETTER BY AND FOR THE MEMBERS OF: Choice in Dying - Ottawa Dying With Dignity Canada Right to Die Society of Canada Sharma is free on $50,000 bail and is no husband John visited her every day; NEWS longer working as a doctor in the area. hospital staff members noticed that they were very devoted to each other. Unfortunately, John also was having in Canada Market Research Done? medical problems. He had suffered a series An August 5 Vancouver Sun story of small strokes, and since then had been Vernon Is Not Lugano or Zurich reported the theft of some drugs from a having memory difficulties. veterinarian’s car. The thief discarded At some point Lorna and John were told As was mentioned in the first 2006 much of the loot but kept 11 vials contain- that Lorna would not be able to live at home issue of Free To Go, nursing homes in ing “a number of different drugs used for any more. When she was well enough to the Swiss cities of Lugano and Zurich have euthanizing or operating on animals”. leave the hospital, she was to be transferred been allowing residents to receive suicide These drugs likely included pento- to a nursing home. assistance (from the group called Exit) for barbital and thiopental. For aid in dying, Both partners probably accepted this, at several years now. pentobarbital (a veterinary euthanatic) is first; John spoke with the manager of his But things are not at that stage in the drug most frequently used when the apartment building about having to move, Vernon BC. -

Marilyn Golden, DRLIB Presentation
Assisted Suicide Laws Marilyn Golden Senior Policy Analyst Disability Rights Education & Defense Fund (DREDF) April 25, 2014 At the Disability Rights Leadership Institute on Bioethics Arlington, Virginia Introduction Thanks much, Diane. Like Diane, I’d like to speak for a while and then open it up for Q&A; please hold your questions until then. If you have questions before then, do write them down! SLIDES 1, 2, 3 Here at DRLIB, we are looking at many issues where our perspective is at serious risk of being lost in the tumult of other views and interests in society. The legalization of assisted suicide may be one of the biggest ones that come up as proposals for major public policy change, regularly and often. By which I mean, there are bills, initiatives, and lawsuits to legalize assisted suicide in at least a few states, sometimes more, every year. Almost all are defeated. Some come close to becoming law, and rarely, but sometimes, one does, in fact, become law, I hate to say. So, did you figure out yet which side we’re on? [laughter] While many people know that Oregon, Washington State, and Vermont have legalized assisted suicide, it is less well known that approximately half the states in the U.S. have either defeated bills to legalize it, or have passed laws explicitly banning it. What they’ve banned—what assisted suicide, when legalized, is—and it’s not easy to say simply—is making it legal for a doctor (generally speaking, a doctor), to prescribe lethal drugs (often thought of as an easy-to-swallow single pill, but actually not so, at all—it’s an onerous to do), to someone who, theoretically, is terminally ill and requests it. -

April 2014 FFRF Complaints © a Better Life/Christopher Johnson Create Buzz
Complimentary Copy Join FFRF Now! Vo1. 31 No. 3 Published by the Freedom From Religion Foundation, Inc. April 2014 FFRF complaints Better Life/Christopher Johnson A © create buzz Rebecca Newberger Goldstein and Steven Pinker, photographed for Christopher Johnson’s A Better Life: 100 Atheists Speak Out on Joy & Meaning in a World Without God. March roared like a lion from begin- the board’s public censure. ning to end in winter-weary Wisconsin, Garnering at least of a week of me- and so did the Freedom From Religion dia attention in March was a letter from Pinker named FFRF’s Foundation, acting on many egregious Co-Presidents Dan Barker and Annie entanglements between religion and Laurie Gaylor to Green Bay Mayor Jim government. Schmitt, reprimanding him for invit- first honorary president FFRF’s complaints stirred up lots of ing the pope to visit the Wisconsin city regional and national news coverage, next year to make “a pilgrimage to the crank mail and crank callers, starting Shrine of Our Lady of Good Help.” with the March 3 announcement that Schmitt’s invitation on city let- religious incursions in science and gov- the Tennessee Board of Judicial Con- terhead was signed “Your servant in ernment, including testifying before duct agreed with FFRF that former Christ” and extolled in excited tones The Freedom From Religion Congress. He prevailed against a pro- magistrate Lu Ann Ballew violated “the events, apparitions and locutions” Foundation is delighted to announce posal at Harvard to require a course on codes of judicial conduct by ordering a in 1859 that “exhibit the substance that world-renowed scientist Steven “Reason and Faith,” saying, “[U]niver- boy’s named changed from Messiah to of supernatural character,” involving Pinker, already an honorary FFRF di- sities are about reason, pure and sim- Martin at an August hearing. -

Physician-Assisted Suicide: Why Physicians Should Oppose It
Physician-Assisted Suicide: Why Physicians Should Oppose It Joseph E. Marine, MD, MBA Division of Cardiology Johns Hopkins University School of Medicine February 2, 2018 Disclosures • No relevant financial disclosures • I am a member of the American College of Physicians, the American Medical Association, and the Baltimore City Medical Society • All of these organizations oppose legalization of physician-assisted suicide and all other forms of euthanasia • There are no drugs or devices that have been approved by the US FDA for physician-assisted suicide or euthanasia Some Definitions • Physician-Assisted Suicide: A form of euthanasia (“good death) where a physician provides the means (such as a lethal drug prescription) for a patient to end his/her own life • Synonyms/ Euphemisms: • Physician/doctor-assisted death • Death with Dignity • End-of-Life Option • (Medical) Aid-in-Dying • includes euthanasia by lethal injection in Canada • Usual drugs used: 90-100 x 100 mg secobarbital tabs dissolved in liquid and swallowed quickly • Antiemetic premed usually given to prevent vomiting PAS/Euthanasia: Background • Mid-1800s – increasing medical use of morphine and chloroform anesthesia leads to proposals to use to hasten death for patients with advanced illnesses • 1906: Euthanasia law proposed in Ohio state legislature, voted down 79-23 • 1920s-1930s: Public support for euthanasia increases in USA, though not legally adopted • 1939-1945: WWII, Nuremberg trials Euthanasia in post-war era • 1945-1980: Little activity • 1980: Derek Humphry, a British journalist, founds Hemlock Society to promote euthanasia and assisted suicide for patients with advanced illness • 1992: Publication of Final Exit • 2003-4: Hemlock Society becomes Compassion and Choices Dr. -
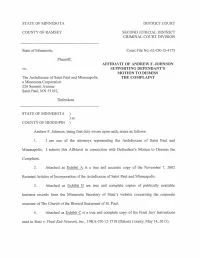
AFFIDAVIT of ANDREW F. JOHNSON SUPPORTING DEFENDANT's MOTION to DISMISS the COMPLAINT the Archdiocese of Saint Paul and Minneapo
STATE OF MINNESOTA DISTRICT COURT COUNTY OF RAMSEY SECOND JUDICIAL DISTRICT CRIMINAL COURT DIVISION State of Minnesota, Court File No: 62-CR-15-4175 Plaintiff, AFFIDAVIT OF ANDREW F. JOHNSON vs. SUPPORTING DEFENDANT'S MOTION TO DISMISS The Archdiocese of Saint Paul and Minneapolis, THE COMPLAINT a Minnesota Corporation 226 Summit Avenue Saint Paul, MN 55102, Defendant. STATE OF MINNESOTA ) ) ss. COUNTY OF HENNEPIN ) Andrew F. Johnson, being first duly sworn upon oath, states as follows: 1. I am one of the attorneys representing the Archdiocese of Saint Paul and Minneapolis. I submit this Affidavit in connection with Defendant's Motion to Dismiss the Complaint. 2. Attached as Exhibit A is a true and accurate copy of the November 7, 2002 Restated Articles of Incorporation of the Archdiocese of Saint Paul and Minneapolis. 3. Attached as Exhibit B are true and complete copies of publically available business records from the Minnesota Secretary of State's website concerning the corporate structure of The Church of the Blessed Sacrament of St. Paul. 4. Attached as Exhibit C is a true and complete copy of the Final Jury Instructions used in State v. Final Exit Network, Inc., 19HA-CR-12-1718 (Dakota County, May 14,2015). 5. Attached as Exhibit D are true and accurate copies of several cases cited in Defendant's Memorandum Supporting Its Motion to Dismiss the Criminal Complaint, including Subscribed and sworn to before me this 29th day of January"...-2,016. /1 " \1 (j IUJ\J)J~~ (]mVJ '/ . Notary Public - 2 - EXHIBIT A 1IIIIIIIIIIIIIIIillll~llllIllilllllllll~II~11111111 C \'--t - (000 \\j F)- f~() ) (2 l-\ 9057060002 CORPORATE RESOLUTION OF THE ARCHDIOCESE OF SAINT PAUL AND MINNEAPOLIS BE IT RESOLVED, That the Articles of Incorporation of the Archdiocese of Saint Paul and Minneapolis, a Minnesota corporation organized and existing under the laws of the State of Minnesota, being Section 315.16, are hereby restated to include therein all amendments made to the original Articles of Incorporation adopted on November 3rd, 1970: RESTATED ARTICLES OF INCORPORATION Article 1. -

2020-Winter.Pdf
FINAL EXIT NETWORK VOL 19 • NO 1 WINTER 2020 IN THIS ISSUE • A devoted husband’s murder-suicide farewell Page 2 • Mary Ewert: dementia and the growing RTD crisis 4 • How ‘Nora’ easily bequeathed a ‘thank you’ gift 5 • Volunteer Hall still leaves a distinguished mark 6 • Veterinarian has poetic take on peaceful deaths 12 • Grateful clients give voice to the essence of FEN 14 T R A I BULETN TO DELIVERANCE ‘My father shot my mother and then himself because her Alzheimer’s was too advanced for anyone to think she was competent to make a decision.’ By Jay Niver, FEN Editor criminal case,” Janet said. “They don’t cover suicides.” murder-suicide usually makes news. The details were unknown to all but the But when that tragedy involves an close friends and family to whom Bob wrote a elderly, devoted couple – and one or A letter, explaining their choice two days before both of them have debilitating dementia or a he pulled the trigger: first for his wife of more terminal disease – it grabs few headlines. than 60 years; then for himself. Authorities, family, friends, and courts The Shavers, too, had a long and storybook recognize that the victims planned and chose marriage. Alma was 80 and he was 79. It ended their exit because they didn’t have (or know) for them on a warm, Sunday afternoon last another way. June as they lay together on their canopy bed. Richard and Alma Shaver decided upon Some would say it ended such a death. But theirs made news across the for them much country after the Sunday New York Times ran a major feature last Dec.