Physician-Assisted Suicide: Why Physicians Should Oppose It
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Right to End-Of-Life Palliative Care and a Dignified Death 1
THE RIGHT TO END-OF-LIFE PALLIATIVE CARE AND A DIGNIFIED DEATH 1 CONTRIBUTION FROM UN-ECLAC FOR THE EXPERT GROUP MEETING ON “CARE AND OLDER PERSONS: LINKS TO DECENT WORK, MIGRATION AND GENDER” 5-7 December 2017 United Nations Headquarters, New York – Secretariat Building, Conference Room S -2725 1. The right to life and dignity in old age The approach of death involves a number of activities, as different practicalities pertaining to the end of life have to be organized. It is essential for these activities —which are carried out by family members, caregivers and medical personnel, among others— to meet standards that ensure appropriate living conditions until such time as clinical and biological death supervenes. Older persons are among the most vulnerable to death. Their position in the age structure of society becomes almost by default a predictor of their demise. This social construction of old age prompts a particular way of treating the elderly: “The social structures in which [older persons] are involved are oriented to the fact of their forthcoming death; their families have become increasingly independent of them; the scope of references to the ‘future’ has progressively narrowed; ‘dying’ is of considerably less consequence for others, e.g., it is not felt to be a matter which requires drastic revision of others’ life plans, as does the ‘fact’ that a young adult is dying” (Sudnow, 1967).2 Older persons are sometimes treated like cadavers even when they are, clinically and biologically, still alive. This occurs especially in cases where they are dying or suffering from terminal illnesses, although they do not necessarily have to be in this predicament to receive degrading treatment. -

Physician-Assisted Suicide and Voluntary Euthanasia: Some Relevant Differences John Deigh
Journal of Criminal Law and Criminology Volume 88 Article 14 Issue 3 Spring Spring 1998 Physician-Assisted Suicide and Voluntary Euthanasia: Some Relevant Differences John Deigh Follow this and additional works at: https://scholarlycommons.law.northwestern.edu/jclc Part of the Criminal Law Commons, Criminology Commons, and the Criminology and Criminal Justice Commons Recommended Citation John Deigh, Physician-Assisted Suicide and Voluntary Euthanasia: Some Relevant Differences, 88 J. Crim. L. & Criminology 1155 (Spring 1998) This Criminal Law is brought to you for free and open access by Northwestern University School of Law Scholarly Commons. It has been accepted for inclusion in Journal of Criminal Law and Criminology by an authorized editor of Northwestern University School of Law Scholarly Commons. 0091-4169/98/8803-1155 THE JOURNAL OF CRIMINAL LAW& CRIMINOLOGY Vol. 88, No. 3 Copyright 0 1998 by Northwestern University, School of Law Prinfd in U.SA. PHYSICIAN-ASSISTED SUICIDE AND VOLUNTARY EUTHANASIA: SOME RELEVANT DIFFERENCES JOHN DEIGH" Yale Kamisar, in a series of influential articles on physician- assisted suicide and voluntary active euthanasia, has written elo- quently in opposition to legalizing these practices.1 Today he revisits the first of these articles, his seminal 1958 article, Some Non-Religious Views Against Proposed "Mercy-Killing"Legislation. 2 In that paper Professor Kamisar used the distinction between the law on the books and the law in action to quiet concerns about the harsh consequences of a blanket prohibition on mercy kill- ing. A blanket prohibition, after all, if strictly applied, would impose criminal punishment on physicians and relatives whose complicity in bringing about the death of a patient, or loved one was justified by the dying person's desperate condition and lucid wish to die. -

The Necessary Right of Choice for Physician-Assisted Suicide
Student Publications Student Scholarship Fall 2017 The ecesN sary Right of Choice for Physician- Assisted Suicide Kerry E. Ullman Gettysburg College Follow this and additional works at: https://cupola.gettysburg.edu/student_scholarship Part of the Applied Ethics Commons, and the Ethics in Religion Commons Share feedback about the accessibility of this item. Ullman, Kerry E., "The eN cessary Right of Choice for Physician-Assisted Suicide" (2017). Student Publications. 574. https://cupola.gettysburg.edu/student_scholarship/574 This open access student research paper is brought to you by The uC pola: Scholarship at Gettysburg College. It has been accepted for inclusion by an authorized administrator of The uC pola. For more information, please contact [email protected]. The ecesN sary Right of Choice for Physician-Assisted Suicide Abstract Research-based paper on the importance of the right for terminally ill patients facing a painful death to be able to choose how they end their life Keywords Assisted-Suicide, Maynard, Kevorkian, Terminally-ill Disciplines Applied Ethics | Ethics in Religion Comments Written for FYS 150: Death and the Meaning of Life. Creative Commons License Creative ThiCommons works is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This student research paper is available at The uC pola: Scholarship at Gettysburg College: https://cupola.gettysburg.edu/ student_scholarship/574 Ullman 1 Kerry Ullman Professor Myers, Ph.D. Death and the Meaning of Life - FYS 30 November 2017 Assisted Suicide The Necessary Right of Choice for Physician-Assisted Suicide Imagine being told you have less than six months left to live. On top of that horrific news, you experience excruciating pain every single day that is far more atrocious than anything you could have possibly imagined. -

Caring for People with Multiple Disabilities : an Interdisciplinary Guide for Caregivers Pdf, Epub, Ebook
CARING FOR PEOPLE WITH MULTIPLE DISABILITIES : AN INTERDISCIPLINARY GUIDE FOR CAREGIVERS PDF, EPUB, EBOOK Cindy French | 145 pages | 29 Mar 1995 | Elsevier Health Sciences | 9780761647058 | English | San Antonio, United States Caring for People with Multiple Disabilities : An Interdisciplinary Guide for Caregivers PDF Book She earned her Ph. Companionship is key to a trusted relationship with our caregivers. Now we get to reconnect a few times a month. Depending on the covered benefits and reimbursement policies of State Medicaid programs, including those provided through waivers, other services may be available to some patients. She later joined the Office of the Center Director as a senior advisor leading and supporting various strategic initiatives such as Clinical Trials Innovation, Real World Evidence, and efforts to improve diversity and inclusion in medical product development. Caregivers in the focus groups consistently reported they did not have time to take care of their own health. We constructed a composite measure of self-care or mobility disability that reflects whether the older adult received help in the prior month with 1 or more self-care eg, eating, dressing, bathing, and toileting or mobility eg, getting outside, getting around inside, and getting out of bed activities. Parents and caregivers should aim to have children be as independent as possible. Care Services. Facilitator Feedback Facilitators agreed that the pilot program went smoothly overall. Training and Education in Professional Psychology , 1 2 , — doi Additionally, the program provides advocacy for residents transitioning from nursing homes back to the community through Money Follows the Person. Compensation for the extra effort involved in caring for patients with complex needs is clearly important. -
How We Die in North Carolina
How We Die in North Carolina ANNE DELLINGER n June 1998 the Wall Street Journal reported on seventy-year- old North Carolinian Claude Marion, who thought that he had prepared for death ten years ahead of time, but still did not re- Iceive the care he wanted.1 After he died, one of his daughters described the experience of acting as his advocate. Speaking of the divisions that emerged among patient, family, and physician, and eventually within the family, she said, [My father] just tried really hard to do the right thing. And he died in a very undignified way. I felt so help- less. My sister and I felt we had been to war. I don’t think there’s a good guy and a bad guy here. I think people were doing what they were taught.2 Following Mr. Marion’s emergency surgery at Wake Forest University Baptist Medical Center in Winston-Salem, he slipped in and out of conscious- ness, unable to make his wishes known. Although four successive complications repeatedly brought him close to death, the attending physician would not honor the living will, believing that Mr. Marion was not “terminal” (defined by the physician as having no chance for recovery).3 A hospital ethics council was convened, which agreed with Mr. Marion’s daughters that his condition was termi- nal. Rejecting the council’s opinion, the physician said he would continue to treat aggressively. A The Death of Socrates, painted by judge appointed Mr. Marion’s daughters his guardians. Meanwhile, Jacques Louis David in 1787, depicts though, some of their aunts and uncles took the physician’s side, the Greek philosopher about to drink and the family began arguing. -

The Constitutional Status of Morals Legislation
Kentucky Law Journal Volume 98 | Issue 1 Article 2 2009 The onsC titutional Status of Morals Legislation John Lawrence Hill Indiana University-Indianapolis Follow this and additional works at: https://uknowledge.uky.edu/klj Part of the Constitutional Law Commons, and the Law and Society Commons Right click to open a feedback form in a new tab to let us know how this document benefits you. Recommended Citation Hill, John Lawrence (2009) "The onC stitutional Status of Morals Legislation," Kentucky Law Journal: Vol. 98 : Iss. 1 , Article 2. Available at: https://uknowledge.uky.edu/klj/vol98/iss1/2 This Article is brought to you for free and open access by the Law Journals at UKnowledge. It has been accepted for inclusion in Kentucky Law Journal by an authorized editor of UKnowledge. For more information, please contact [email protected]. TKenf]iky Law Jornal VOLUME 98 2009-2010 NUMBER I ARTICLES The Constitutional Status of Morals Legislation John Lawrence Hiff TABLE OF CONTENTS INTRODUCTION I. MORALS LEGISLATION AND THE HARM PRINCIPLE A. Some Difficulties with the Concept of "MoralsLegislation" B. The Near Irrelevance of the PhilosophicDebate C. The Concept of "Harm" II. DEFINING THE SCOPE OF THE PRIVACY RIGHT IN THE CONTEXT OF MORALS LEGISLATION III. MORALS LEGISLATION AND THE PROBLEMS OF RATIONAL BASIS REVIEW A. The 'RationalRelation' Test in Context B. The Concept of a Legitimate State Interest IV. MORALITY AS A LEGITIMATE STATE INTEREST: FIVE TYPES OF MORAL PURPOSE A. The Secondary or IndirectPublic Effects of PrivateActivity B. Offensive Conduct C. Preventingthe Corruptionof Moral Character D. ProtectingEssential Values andSocial Institutions E. -
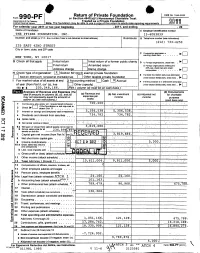
Return of Private Foundation CT' 10 201Z '
Return of Private Foundation OMB No 1545-0052 Form 990 -PF or Section 4947(a)(1) Nonexempt Charitable Trust Department of the Treasury Treated as a Private Foundation Internal Revenue Service Note. The foundation may be able to use a copy of this return to satisfy state reporting requirem M11 For calendar year 20 11 or tax year beainnina . 2011. and ending . 20 Name of foundation A Employer Identification number THE PFIZER FOUNDATION, INC. 13-6083839 Number and street (or P 0 box number If mail is not delivered to street address ) Room/suite B Telephone number (see instructions) (212) 733-4250 235 EAST 42ND STREET City or town, state, and ZIP code q C If exemption application is ► pending, check here • • • • • . NEW YORK, NY 10017 G Check all that apply Initial return Initial return of a former public charity D q 1 . Foreign organizations , check here . ► Final return Amended return 2. Foreign organizations meeting the 85% test, check here and attach Address chang e Name change computation . 10. H Check type of organization' X Section 501( exempt private foundation E If private foundation status was terminated Section 4947 ( a)( 1 ) nonexem pt charitable trust Other taxable p rivate foundation q 19 under section 507(b )( 1)(A) , check here . ► Fair market value of all assets at end J Accounting method Cash X Accrual F If the foundation is in a60-month termination of year (from Part Il, col (c), line Other ( specify ) ---- -- ------ ---------- under section 507(b)(1)(B),check here , q 205, 8, 166. 16) ► $ 04 (Part 1, column (d) must be on cash basis) Analysis of Revenue and Expenses (The (d) Disbursements total of amounts in columns (b), (c), and (d) (a) Revenue and (b) Net investment (c) Adjusted net for charitable may not necessanly equal the amounts in expenses per income income Y books purposes C^7 column (a) (see instructions) .) (cash basis only) I Contribution s odt s, grants etc. -
EUTHANASIA and RELIGION the Advance of Technologies to Prolong Life and Control Dying Can Raise Agonizing Moral Dilemmas
Article 32 EUTHANASIA AND RELIGION The advance of technologies to prolong life and control dying can raise agonizing moral dilemmas. What guidance is offered by the great world religions? Courtney S. Campbell In “The Parable of the Mustard Seed”, the Buddha choices, religious traditions and values can offer guid- teaches a lesson that is valid for all cultures: human be- ance and insight, if not solutions. ings receive no exemption from mortality. Deep in the Historically, religious communities have sought to ap- throes of grief after the death of her son, a woman seeks propriate death within the life cycle through rituals of re- wisdom from the Buddha, who says that he does indeed membrance, and religious teachings have emphasized have an answer to her queries. Before giving it, however, that death brings meaning to mortality. The process of he insists that she must first collect a grain of mustard dying is often portrayed as an invitation to spiritual in- seed from every house that has not been touched by sight and a key moment in the cultivation of spiritual death. She canvasses her entire community, but fails to identity. collect a single seed. Returning to the Buddha, she un- derstands that, like all other living beings, we are des- tined to die. Judaism, Christianity and Islam Death is a defining characteristic of human experience. Yet, while the event of death remains elusively beyond basically address ethical issues human control, the process of dying has increasingly concerning the end of life from a been brought into the domain of medicine and life- extending technologies. -

Attitude of Doctors Toward Euthanasia in Delhi, India
Published online: 2019-04-05 Original Article AAttitudettitude ooff ddoctorsoctors ttowardoward eeuthanasiauthanasia iinn DDelhi,elhi, IIndiandia ABSTRACT Introduction: Deliberation over euthanasia has been enduring for an extended period of time. On one end, there are populaces talking for the sacrosanctity of life and on the other end, there are those, who promote individual independence. All over the world professionals from different areas have already spent mammoth period over the subject. A large number of cases around the world have explored the boundaries of current legal distinctions, drawn between legitimate and nonlegitimate instances of ending the life. The term euthanasia was derived from the Greek words “eu” and “thanatos” which means “good death” or “easy death.” It is also known as mercy killing. Euthanasia literally means putting a person to painless death especially in case of incurable suffering or when life becomes purposeless as a result of mental or physical handicap. Objective: To study the attitude of doctors toward euthanasia in Delhi. Methodology: It was a questionnaire based descriptive cross-sectional study carried out between July 2014 and December 2014. The study population included Doctors from 28 hospitals in Delhi both public and private. Equal numbers of doctors from four specialties were included in this study (50 oncologists, 50 hematologists, 50 psychiatrists, and 50 intensivists). Demographic questionnaire, as well as the Euthanasia Attitude Scale (EAS), a 30 items Likert-scale questionnaire developed by (Holloway, Hayslip and Murdock, 1995) was used to measure attitude toward Euthanasia. The scale uses both positively (16 items) and negatively (14 items) worded statements to control the effect of acquiescence. -
FENA Conversation with Fran
FINAL EXIT NETWORK VOL 18 • NO 1 WINTER, JAN/FEB 2019 CONTENTS TTHEHE TIME TO IMPROVE OREGON-STYLE LAWS? .........3 GOODGOOD DEMENTIA ADVANCE DEATHDEATH DIRECTIVES ...........................5 FISCAL YEAR REPORT ............9 SOCIETYSOCIETY AMERICANS ACCEPT FEN EUTHANASIA ..................... 11 A Conversation With Fran By Michael James, FEN Life Member enior Guide Fran Schindler’s voice was raspy after five days of protesting in Washington, DC, but this remarkable 79- Q: year-old’sS enthusiasm for FEN and life in general was loud and clear. “The privilege of someone being What’s going to willing to have me with them when they die, when I happen to you? only just sit with them, is the most meaningful thing I have ever done.” In the late 1980s, Fran faced a series of daunt- ing issues: a brain tumor, divorce, and mysterious A. symptoms which mimicked ALS. She acknowledg- es she became obsessed with finding ways to kill I will get dead. herself during those dark days. Eventually she heard Faye Girsh lecture about FEN. She quickly signed up for training and got her FEN membership card in November 2006. Twelve years later she estimates FRAN continued on page 2 Renew your membership online: www.finalexitnetwork.org FRAN continued from page 1 she’s been present for over 70 individuals who have taken their lives using FEN protocol. “At the FEN training class I discovered a major benefit of being a “Start doing FEN member. I looked at the trainers and my fellow classmates—people who didn’t know me—and real- what you want ized that if I needed them they would be there for me. -

NOW Is Time to Address Dementia
The Human Right To A Death With Dignity Special Edition FEN responds in hour of crises VOL 19 • NO 2 SPRING 2020 NOW is time to address dementia Final Exit Network has created surrounding the explosion in a new Advance Directive designed Alzheimer’s and other forms of to prevent dying people from being dementia, because no state that offers force fed against their wishes – Medical Aid in Dying accommodates even if suffering from dementia. patients who are not “of sound mind” What’s more, FEN will go to court when it is time to receive assistance. in an effort to set a legal precedent Now there is a second, more ensuring that VSED (Voluntarily pressing crisis: COVID-19. The Stopping Eating and Drinking) is specter of a ventilator is now reality always available to those who sign for many of us who were already the Supplemental Advance Directive concerned about how we would die. for Dementia Care. FEN is stepping up in this time This document, and the drive to of dual crises, and this edition of the make it legally binding, has been magazine is keenly focused on on our agenda for some time. We what we all need to know. recognized the growing crisis – Brian Ruder, FEN President Life (and death) in the time of COVID-19 By Lowrey Brown words apply equally well when applied to laws FEN Client Services Director and social customs that would rob so many of The title is hardly original wordplay at the right to shape how their life stories end. -

Physician-Assisted Suicide
Recent Developments in Physician-Assisted Suicide October 2001 Copyright © 2001 Valerie J. Vollmar, all rights reserved. LITIGATION 1. Sampson v. Alaska, No. 3AN-98-11288CI (Alaska Super. Ct.), aff'd, 31 P.3d 88 (Alaska 2001). On 12/15/98, Kevin Sampson (a 43-year-old HIV-positive man) and "Jane Doe" (a female physician in her 60's with cancer) filed suit in Alaska Superior Court in Anchorage challenging Alaska's ban on physician-assisted suicide based on state constitutional claims of privacy, liberty, and equal protection. On 9/9/99, Judge Eric T. Sanders issued a written opinion rejecting the plaintiffs' claims and granting summary judgment to the defendant. On 11/14/00, the Alaska Supreme Court heard arguments on the appeal. On 9/21/01, the supreme court issued an opinion affirming the lower court's decision. 2. Cooley v. Granholm, No. 99-CV-75484 (E.D. Mich.), appeal pending, No. 01-1067 (6th Cir.). On 11/12/99, Professor Robert Sedler filed a federal lawsuit against Attorney General Jennifer Granholm and the Michigan Board of Medicine on behalf of two Michigan physicians, Roy Cooley and M.W. El-Nachef. The plaintiffs claimed that Michigan's ban on assisted suicide violates the Fourteenth Amendment right "to be relieved from unbearable pain and suffering." On 12/20/00, Judge Nancy G. Edmunds granted the defendants' motion for summary judgment and dismissed the complaint. On 1/12/01, plaintiffs appealed to the Sixth Circuit Court of Appeals. The final brief on appeal was filed on 6/4/01. Both sides have requested oral argument.