How We Die in North Carolina
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Physician-Assisted Suicide
Recent Developments in Physician-Assisted Suicide October 2001 Copyright © 2001 Valerie J. Vollmar, all rights reserved. LITIGATION 1. Sampson v. Alaska, No. 3AN-98-11288CI (Alaska Super. Ct.), aff'd, 31 P.3d 88 (Alaska 2001). On 12/15/98, Kevin Sampson (a 43-year-old HIV-positive man) and "Jane Doe" (a female physician in her 60's with cancer) filed suit in Alaska Superior Court in Anchorage challenging Alaska's ban on physician-assisted suicide based on state constitutional claims of privacy, liberty, and equal protection. On 9/9/99, Judge Eric T. Sanders issued a written opinion rejecting the plaintiffs' claims and granting summary judgment to the defendant. On 11/14/00, the Alaska Supreme Court heard arguments on the appeal. On 9/21/01, the supreme court issued an opinion affirming the lower court's decision. 2. Cooley v. Granholm, No. 99-CV-75484 (E.D. Mich.), appeal pending, No. 01-1067 (6th Cir.). On 11/12/99, Professor Robert Sedler filed a federal lawsuit against Attorney General Jennifer Granholm and the Michigan Board of Medicine on behalf of two Michigan physicians, Roy Cooley and M.W. El-Nachef. The plaintiffs claimed that Michigan's ban on assisted suicide violates the Fourteenth Amendment right "to be relieved from unbearable pain and suffering." On 12/20/00, Judge Nancy G. Edmunds granted the defendants' motion for summary judgment and dismissed the complaint. On 1/12/01, plaintiffs appealed to the Sixth Circuit Court of Appeals. The final brief on appeal was filed on 6/4/01. Both sides have requested oral argument. -

The Right to Assisted Suicide and Euthanasia
THE RIGHT TO ASSISTED SUICIDE AND EUTHANASIA NEIL M. GORSUCH* I. INTRODUCTION ........................................................ 600 I. THE COURTS ............................................................. 606 A. The Washington Due Process Litigation............ 606 1. The Trial Court ...................... 606 2. The Ninth Circuit Panel Decision ............. 608 3. The En Banc Court ...................................... 609 B. The New York Equal ProtectionLitigation ........ 611 1. The Trial Court ........................................... 611 2. The Second Circuit ..................................... 612 C. The Supreme Court............................................. 613 1. The Majority Opinion ................................. 614 2. The Concurrences ....................................... 616 D. The Consequences ofGlucksberg and Quill .... 619 III. ARGUMENTS FROM HISTORY ................................... 620 A. Which History?................................................... 620 B. The Ancients ....................................................... 623 C. Early Christian Thinkers .................................... 627 D. English Common Law ......................................... 630 E. ColonialAmerican Experience........................... 631 F. The Modern Consensus: Suicide ........................ 633 G. The Modern Consensus: Assisting Suicide and Euthanasia.......................................................... 636 IV. ARGUMENTS FROM FAIRNESS .................................. 641 A . Causation........................................................... -
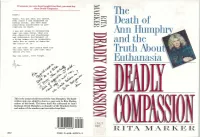
The Death of and the -1 Truth About, Euthanasia
If someone you care about bought FinaZElxit, you must buy them D~lyComl,assiOn. Derek : The There. You got what you wanted. Ever since I was diagnosed as having cancer, you have done Death of everything conceivable to pre- cipitate my death. I was not alone in recognizing what you were doing. What you Hulll~hrvA did--desertion and abandonment Ann and subsequent harrassment of a dying woman--is so unspeakble there are no words to describe -1 the horror of it. and the Yet you know. And others know too. You will have to live with this untiol you die. Truth About, 1 May you never, ever forget. Euthanasia This is the actual suicide letter left by Ann Humphry. The hand- written note was added by Ann to a copy sent to Rita Marker, author of this book. The letter itself was addressed to Ann's husband, Derek Humphry, co-founder of the Hemlock Society and author of the number-one best-seller Rnal Exit. - '1 MAR 1 t RITA MARKER ISBN 0-688-12223-3 8 ,'\- IF " ISBN 0-688-12221-3 FPT $18.00 wtinuedfiomfiotatjap) ,, Tack Kevorkian. who has written article advocating medical experiments on death row prisoners -while they are still alive. An( she explains the ramifications of euthanasia course is not the same as giving in a country without adequate health insur- doctors the right to kill ance, like America, where people who really their patients on demand. want to live might choose death rather than bankrupt their families. Deadly Compassion is essential reading for anyone who has misgivings about giving DEADLY COMPASSION doctors the right to kill. -

Freedom to Flourish: a Catholic Analysis of Doctor–Prescribed Suicide and Euthanasia
V VERITAS Freedom to Flourish: A Catholic Analysis of Doctor–Prescribed Suicide and Euthanasia Jason B. Negri, JD and Father Christopher M. Saliga, O.P., RN The Veritas Series is dedicated to Blessed Michael McGivney (1852-1890), priest of Jesus Christ and founder of the Knights of Columbus. The Knights of Columbus presents The Veritas Series “Proclaiming the Faith in the Third Millennium” Freedom to Flourish: A Catholic Analysis of Doctor-Prescribed Suicide and Euthanasia by JASON B. NEGRI, JD & FR. CHRISTOPHER M. SALIGA, O.P., RN General Editor Fr. Juan-Diego Brunetta, O.P. Catholic Information Service Knights of Columbus Supreme Council Printed With Ecclesiastical Permission. Most Reverend Earl Boyea November 3, 2010 Diocese of Lansing Copyright ©2011-2021 by Knights of Columbus Supreme Council. All rights reserved. Cover: © 2011-2021 by Knights of Columbus Supreme Council. All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by information storage and retrieval system, without permission in writing from the publisher. Write: Catholic Information Service Knights of Columbus Supreme Council PO Box 1971 New Haven CT 06521-1971 www.kofc.org/cis [email protected] 203-752-4267 800-735-4605 fax Printed in the United States of America CONTENTS INTRODUCTION . 5 KILLING TO END SUFFERING?. 6 RATIONALE FOR KILLING . 7 SUFFERING. 9 LOSS OF AUTONOMY . 11 AUTONOMY AND THE CASE OF JO ROMAN . 13 FREEDOM TO FLOURISH . 15 FREEDOM TO FLOURISH: THE CASE OF CHRISTI CHRONOWSKI . 17 CHRISTI’S DIAGNOSIS: A VIRTUAL GUARANTEE OF SUFFERING AND DEATH. -

Physician-Assisted Suicide: Why Physicians Should Oppose It
Physician-Assisted Suicide: Why Physicians Should Oppose It Joseph E. Marine, MD, MBA Division of Cardiology Johns Hopkins University School of Medicine February 2, 2018 Disclosures • No relevant financial disclosures • I am a member of the American College of Physicians, the American Medical Association, and the Baltimore City Medical Society • All of these organizations oppose legalization of physician-assisted suicide and all other forms of euthanasia • There are no drugs or devices that have been approved by the US FDA for physician-assisted suicide or euthanasia Some Definitions • Physician-Assisted Suicide: A form of euthanasia (“good death) where a physician provides the means (such as a lethal drug prescription) for a patient to end his/her own life • Synonyms/ Euphemisms: • Physician/doctor-assisted death • Death with Dignity • End-of-Life Option • (Medical) Aid-in-Dying • includes euthanasia by lethal injection in Canada • Usual drugs used: 90-100 x 100 mg secobarbital tabs dissolved in liquid and swallowed quickly • Antiemetic premed usually given to prevent vomiting PAS/Euthanasia: Background • Mid-1800s – increasing medical use of morphine and chloroform anesthesia leads to proposals to use to hasten death for patients with advanced illnesses • 1906: Euthanasia law proposed in Ohio state legislature, voted down 79-23 • 1920s-1930s: Public support for euthanasia increases in USA, though not legally adopted • 1939-1945: WWII, Nuremberg trials Euthanasia in post-war era • 1945-1980: Little activity • 1980: Derek Humphry, a British journalist, founds Hemlock Society to promote euthanasia and assisted suicide for patients with advanced illness • 1992: Publication of Final Exit • 2003-4: Hemlock Society becomes Compassion and Choices Dr. -

FDA Regulation and Patient Assisted Suicides
FDA Regulation and Patient Assisted Suicides The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation FDA Regulation and Patient Assisted Suicides (1995 Third Year Paper) Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:8965589 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA FDA Regulation and Patient Assisted Suicides David S. Weiss The 20th century has witnessed a steady, marked increase in the average life expectancy of Americans. Advances in nutrition, an increased em- phasis on preventative health care, and developments in the treatment and miti- gation of cancer and other fatal illnesses are among the many factors which have contributed most recently to the ability of Americans to live longer, healthier lives. Even with these advances, however, there are an increasing number of Americans who believe that the marginal benefit of surviving a few extra months is not worth the cost of suffering the pain, physical and/or mental deterioration, or increased dependency they would experience during that period due to a terminal illness or a debilitating condition. For these people, the right to opt to die painlessly, simply, and with dignity at the time and place of their choosing is paramount, and in recent years they have taken steps to secure that right. Their convictions have given rise to the Hemlock Society,1 the passage of an Oregon referendum authorizing physician-assisted suicide,2 and the work of Dr. -

The Hemlock Society: What We Are, What We Aren't, and Why
Journal of Civil Rights and Economic Development Volume 12 Issue 3 Volume 12, Summer 1997, Issue 3 Article 12 The Hemlock Society: What We Are, What We Aren't, and Why Faye J. Girsh Follow this and additional works at: https://scholarship.law.stjohns.edu/jcred This Symposium is brought to you for free and open access by the Journals at St. John's Law Scholarship Repository. It has been accepted for inclusion in Journal of Civil Rights and Economic Development by an authorized editor of St. John's Law Scholarship Repository. For more information, please contact [email protected]. THE HEMLOCK SOCIETY: WHAT WE ARE, WHAT WE AREN'T, AND WHY FAYE J. GIRSH* According to my count, the position favoring physician-aid-in- dying is outnumbered here eight to three. So, as the wrap-up speaker, I will try to summarize some of the arguments. I do want to note, however, that this eight to three ratio is the oppo- site of what we see in public opinion polls, which show at least 70% support for some form of legalization of physician aid in dying not only in the United States, but in Canada, Australia, and the United Kingdom. Surveys indicate that Americans favor the right by about three to one, 1 and this number is growing, I 2 might add, as every survey comes in. * Executive Director, Hemlock Society USA; Ed.D, Harvard University. Before accept- ing her position as Executive Director of the Hemlock Society USA, Dr. Girsh was a clini- cal and forensic psychologist in San Diego testifying and evaluating litigants in civil and criminal cases, as well as Founder, President and Newsletter Editor of the Hemlock So- ciety of San Diego; President of the San Diego Psych-Law Society and Psychologists in Addictive Behavior; Board Member of KPBS, the public broadcasting station in San Di- ego, and Board Member of several ACLU affiliates, Americans for Death with Dignity and the Euthanasia Research and Guidance Organization. -

2020-Winter.Pdf
FINAL EXIT NETWORK VOL 19 • NO 1 WINTER 2020 IN THIS ISSUE • A devoted husband’s murder-suicide farewell Page 2 • Mary Ewert: dementia and the growing RTD crisis 4 • How ‘Nora’ easily bequeathed a ‘thank you’ gift 5 • Volunteer Hall still leaves a distinguished mark 6 • Veterinarian has poetic take on peaceful deaths 12 • Grateful clients give voice to the essence of FEN 14 T R A I BULETN TO DELIVERANCE ‘My father shot my mother and then himself because her Alzheimer’s was too advanced for anyone to think she was competent to make a decision.’ By Jay Niver, FEN Editor criminal case,” Janet said. “They don’t cover suicides.” murder-suicide usually makes news. The details were unknown to all but the But when that tragedy involves an close friends and family to whom Bob wrote a elderly, devoted couple – and one or A letter, explaining their choice two days before both of them have debilitating dementia or a he pulled the trigger: first for his wife of more terminal disease – it grabs few headlines. than 60 years; then for himself. Authorities, family, friends, and courts The Shavers, too, had a long and storybook recognize that the victims planned and chose marriage. Alma was 80 and he was 79. It ended their exit because they didn’t have (or know) for them on a warm, Sunday afternoon last another way. June as they lay together on their canopy bed. Richard and Alma Shaver decided upon Some would say it ended such a death. But theirs made news across the for them much country after the Sunday New York Times ran a major feature last Dec. -

Don't Tell: the Secret Practice of Physician-Assisted Suicide, 44 Hastings L.J
Hastings Law Journal Volume 44 | Issue 6 Article 3 1-1993 Don't Ask--Don't Tell: The ecrS et Practice of Physician-Assisted Suicide Julia Pugliese Follow this and additional works at: https://repository.uchastings.edu/hastings_law_journal Part of the Law Commons Recommended Citation Julia Pugliese, Don't Ask--Don't Tell: The Secret Practice of Physician-Assisted Suicide, 44 Hastings L.J. 1291 (1993). Available at: https://repository.uchastings.edu/hastings_law_journal/vol44/iss6/3 This Note is brought to you for free and open access by the Law Journals at UC Hastings Scholarship Repository. It has been accepted for inclusion in Hastings Law Journal by an authorized editor of UC Hastings Scholarship Repository. For more information, please contact [email protected]. Note Don't Ask-Don't Tell: The Secret Practice of Physician-Assisted Suicide by JULIA PUGLIESE* It hath often been said that it is not death but dying that is terrible.1 Introduction Initially, Dr. Ethan Green2 was opposed to assisted suicide.3 How- ever, he was forced to reevaluate his position when a patient with AIDS, Michael Ellis, asked him for help in ending his life. Dr. Green thought he would be able to dissuade Michael by suggesting an aggressive pain treatment plan. After consultation the patient refused to accept the treatment option. Michael wanted to die. Dr. Green agonized over whether he should help Michael. He ini- tially told Michael that he needed to know more about him and his views and about the situation before he could make a decision to help. Dr. -

Physician-Assisted Suicide
Recent Developments in Physician-Assisted Suicide July 1998 Copyright © 1998 Valerie J. Vollmar, all rights reserved. LITIGATION 1. Lee v. Oregon, 107 F.3d 1382 (9th Cir. 1997), cert. denied sub nom Lee v. Harcleroad, 118 S.Ct. 328, 139 L.Ed.2d 254 (1997). Pursuant to the Ninth Circuit's mandate, U.S. District Judge Michael Hogan dismissed this case during a status hearing held on 11/25/97. However, Judge Hogan agreed to entertain further briefs regarding standing questions. On 2/18/98, Judge Hogan heard argument on the plaintiffs' motion to amend their complaint to allege that plaintiff Janice Elsner has standing due to the "stigmatic injury" that has resulted because legalizing physician-assisted suicide devalues her life; Judge Hogan has taken this motion under advisement. Also on 2/18/98, the plaintiffs filed another motion to amend their complaint to join Peter Begin, a terminally ill patient, as a new plaintiff; although Begin died on 2/26/98, Troy Thompson, a 36-year-old man with ALS, has agreed to serve as a plaintiff. On 4/7/98, plaintiffs filed a motion to certify the case as a class action. A hearing on pending motions is scheduled for 7/13/98. The plaintiffs hope that a favorable ruling on the standing question would lead Judge Hogan to resurrect his decision on the merits. If Judge Hogan rules against the plaintiffs, the opponents of the Oregon Death with Dignity Act are expected to file a new lawsuit. 2. Kevorkian v. Arnett, 939 F.Supp. 725 (C.D. -
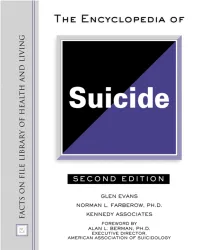
The Encyclopedia of Suicide, 2Nd Revised Edition (Facts on File
THE ENCYCLOPEDIA OF SUICIDE Second Edition THE ENCYCLOPEDIA OF SUICIDE Second Edition Glen Evans Norman L. Farberow, Ph.D. Kennedy Associates Foreword by Alan L. Berman, Ph.D. Executive Director, American Association of Suicidology The Encyclopedia of Suicide, Second Edition Copyright © 2003 by Margaret M. Evans All rights reserved. No part of this book may be reproduced or utilized in any form or by any means, elec- tronic or mechanical, including photocopying, recording, or by any information storage or retrieval sys- tems, without permission in writing from the publisher. For information contact: Facts On File, Inc. 132 West 31st Street New York NY 10001 Library of Congress Cataloging-in-Publication Data Evans, Glen The encyclopedia of suicide / Glen Evans, Norman L. Farberow.—2nd ed. p. cm. Includes bibliographical references and index. ISBN 0-8160-4525-9 1. Suicide—Dictionaries. 2. Suicide—United States—Dictionaries. 3. Suicide—United States—Statistics. 4. Suicide victims—Services for—United States—Directories. 5. Suicide victims—Services for— Canada—Directories. I. Farberow, Norman L. II. Title. III. Series. HV6545 .E87 2003 362.28'03—dc21 2002027166 Facts On File books are available at special discounts when purchased in bulk quantities for businesses, associations, institutions, or sales promotions. Please call our Special Sales Department in New York at (212) 967-8800 or (800) 322-8755. You can find Facts On File on the World Wide Web at http://www.factsonfile.com Text and cover design by Cathy Rincon Printed in the United States of America VB FOF 10 9 8 7 6 5 4 3 2 1 This book is printed on acid-free paper. -

Legalizing Physician-Assisted Suicide: Some Thoughts and Concerns
Special A rticle Legalizing Physician-Assisted Suicide: Some Thoughts and Concerns Harold G. Koenig, M D, M HSc Durham, North Carolina Surveys show that most Americans favor the decrimi medicine in unpredictable ways, yet physicians are par nalization of phvsician-assisted suicide in certain cir ticipating relatively little in deliberations concerning cumstances. Several states are now considering legisla this issue. The problem o f suffering in persons with tion to bring this about and make the United States chronic and terminal illness cannot be ignored. C om the first place in the civilized world where physician aid passionate, effective, and ethical solutions must be in dying is sanctioned. In the Netherlands, where phy found. As a former family physician and now geriatric sician-assisted suicide is practiced but officially remains psychiatrist, I review the pros and cons of physician-as illegal, 85% o f assisted suicides occur in the elderly, sisted suicide (emphasizing arguments against legaliza and most involve the help o f general practitioners. In tion) and encourage family physicians to debate this the United States, family physicians provide health care matter. to many older adults with chronic or terminal illness whose numbers will increase as the elderly population Key words. Suicide; aged; euthanasia; ethics; patient expands. The legalization o f physician-assisted suicide advocacy; quality' o f life. ( / Fam Fract 1993; would affect the way American physicians practice 37:171-179) Most physicians have had patients with advanced cancer, Clarification of Terms end-stage heart failure, severe chronic obstructive pulmo To discuss this topic intelligently, one must carefully nary disease, or other disabling and painful diseases.