Changes in Lipid Profile of Keratinocytes from Rat Skin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Technical Reports
TECHNICAL REPORTS Lipid microarrays identify key mediators of autoimmune brain inflammation Jennifer L Kanter1,2, Sirisha Narayana2, Peggy P Ho2, Ingrid Catz3, Kenneth G Warren3, Raymond A Sobel4,6, Lawrence Steinman2 & William H Robinson5,6 Recent studies suggest that increased T-cell and autoantibody against phospholipids and gangliosides contribute to the pathogenesis reactivity to lipids may be present in the autoimmune in systemic lupus erythematosus and Guillain-Barre´ syndrome, respec- demyelinating disease multiple sclerosis. To perform large-scale tively10. Despite reports of myelin-specific lipid responses in multiple multiplex analysis of antibody responses to lipids in multiple sclerosis, the role of lipid-specific autoimmunity in multiple sclerosis sclerosis, we developed microarrays composed of lipids remains controversial11. Most lipids are presented to T cells bound to 12 http://www.nature.com/naturemedicine present in the myelin sheath, including ganglioside, sulfatide, CD1 molecules and CD1 expression is increased in CNS lesions in cerebroside, sphingomyelin and total brain lipid fractions. Lipid- both multiple sclerosis and experimental autoimmune encephalomye- array analysis showed lipid-specific antibodies against sulfatide, litis (EAE)13–15. These observations led us to hypothesize that myelin sphingomyelin and oxidized lipids in cerebrospinal fluid (CSF) lipids may be target autoantigens in individuals with multiple sclerosis derived from individuals with multiple sclerosis. Sulfatide- and to develop lipid-array technology to investigate this hypothesis. specific antibodies were also detected in SJL/J mice with We developed simple, large-scale lipid microarrays for detection of acute experimental autoimmune encephalomyelitis (EAE). autoantibodies present in biological fluids such as serum and cere- Immunization of mice with sulfatide plus myelin peptide brospinal fluid (CSF). -

Transglutaminase in Ocular Health and Pathological Processes
perim Ex en l & ta a l ic O p in l h t C h f Journal of Clinical & Experimental a Tong et al. J Clinic Experiment Ophthalmol 2011, S:2 o l m l a o n l DOI: 10.4172/2155-9570.S2-002 r o g u y o J Ophthalmology ISSN: 2155-9570 ResearchResearch Article Article OpenOpen Access Access Recent Advances: Transglutaminase in Ocular Health and Pathological Processes Louis Tong1,2,3*, Evelyn Png2, Wanwen Lan2 and Andrea Petznick2 1Singapore National Eye Center, Singapore 2Singapore Eye Research Institute, Singapore 3Duke-NUS Graduate Medical School, Singapore Abstract Transglutaminase (TG) is a diverse class of crosslinking enzymes involved in the regulation of cytokine production, endocytosis, cell adhesion, migration, apoptosis and autophagy. It has been implicated in inflammatory diseases, neurodegenerative processes and cancer. The eye is a specialized organ which subserves the important function of vision and has distinctive physiological and anatomical properties that differ from other body tissues. Understanding of the roles of various TGs in the eye therefore require studies specific to cells and tissues of ocular origin. We review the advances in TG research in ocular diseases, including pterygium, glaucoma, cataract and proliferative vitreoretinopathy. TG1 is a molecule important for keratinisation in many cicatrizing diseases of the ocular surface, including keratoconjunctivitis sicca. TG2, with multiple functions, has been shown to be important in inflammation and cell adhesion in various ocular diseases. The results of TG research in each region of the eye are critically assessed and the implications of these studies in the treatment of ocular diseases are discussed. -

Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (Membrane/Cardiolipin/Gangliosides/Ca + +/Phase Transition) J
Proc. Nat. Acad. Sci. USA Vol. 70, No. 5, pp. 1406-1409, May 1973 Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (membrane/cardiolipin/gangliosides/Ca + +/phase transition) J. M. BOGGS AND J. C. HSIA Department of Pharmacology, Faculty of Medicine, University of Toronto, Toronto M5S 1A8 Ontario, Canada Communicated by David E. Green, March 5, 1973 ABSTRACT The acyl chain of spin-labeled fatty acids preferred orientation in cylindrical and spherical micellar intercalates between the lipid hydrocarbon chains in hexag- phases with the long axis parallel to the lipid acyl chains, onal and micellar phases with the carboxyl group anchored at the lipid water interface. The spectra are resulting in spectra characteristic of rapid anisotropic motion characteristic of anisotropic motion and cannot be dis- and (b) there is a fluidity gradient in the hexagonal phase, tinguished from the spectra of these probes in lamellar i.e., the motional freedom of the acyl chains increases toward dispersions. In the hexagonal and micellar phases the the terminal methyl group as has been observed for the molecular motion of the spin label increases as it is moved further away from the carboxyl group, similar to the be- lamellar phase (2, 4, 5). havior in the lamellar phase (Jost et al. (1971) J. Mol. Biol. 59, 77-98). The similarity in packing of the acyl chains in MATERIALS AND METHODS the hexagonal and lamellar phases suggests that localized 5-Doxyl-palmitic acid [1(10,3)] and 8-doxyl-palmitic acid regions of hexagonal phase are compatible with a bilayer [I(7,6)] were prepared according to the method of Hubbell matrix. -
Technical Data Sheet
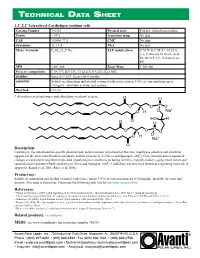
TECHNICAL DA T A SHEE T 1,1’,2,2’ Tetraoleoyl Cardiolipin (sodium salt) Catalog Number 710335 Physical state Powder; chloroform solution Purity > 99% Transition temp. No data CAS 115404-77-8 CMC No data Synonyms 18:1 CA PKA No data Molec. Formula C81H148O17P2Na2 TLC mobile phase C:M:W & C:M:A*, 65:25:4, v/v; C:Hexane:M:Acetic Acid 50:30:10:5, v/v, if want to see PG MW 1,501.000 Exact Mass 1,501.000 Percent composition C 64.77% H 9.93% O 18.11% P 4.12% Na 3.06% Stability Store in <-20°C freezer for 6 months Solubility Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Web link 710335 * chloroform:methanol:water and chloroform:methanol:acetone Description: Cardiolipin, the mitochondrial-specific phospholipid, helps maintain mitochondrial function, membrane potential and structural support for the inner mitochondrial membrane and the proteins in it (Chicco and Sparagna, 2007). Concentration and composition changes of cardiolipin have been implicated in pathological conditions including ischemia, hypothyroidism, aging, heart failure and cardioskeletal myopathy (Barth syndrome) (Chicco and Sparagna, 2007). Cardiolipin has also been shown as a signaling molecule in apoptosis (Kagan et al, 2006; Ritov et al, 2006). Product use: Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Also used in liposomes. Please use the following web link for liposome preparation. References: • Huang and Frohman (2009). -

Antiphospholipid Antibodies Detected by Line Immunoassay Differentiate
Roggenbuck et al. Arthritis Research & Therapy (2016) 18:111 DOI 10.1186/s13075-016-1018-x RESEARCH ARTICLE Open Access Antiphospholipid antibodies detected by line immunoassay differentiate among patients with antiphospholipid syndrome, with infections and asymptomatic carriers Dirk Roggenbuck1,2*†, Maria Orietta Borghi3,4†, Valentina Somma2, Thomas Büttner5, Peter Schierack2, Katja Hanack6, Claudia Grossi4, Caterina Bodio3, Paolo Macor7, Philipp von Landenberg8, Francesco Boccellato9, Michael Mahler10 and Pier Luigi Meroni3,4 Abstract Background: Antiphospholipid antibodies (aPL) can be detected in asymptomatic carriers and infectious patients. The aim was to investigate whether a novel line immunoassay (LIA) differentiates between antiphospholipid syndrome (APS) and asymptomatic aPL+ carriers or patients with infectious diseases (infectious diseases controls (IDC)). Methods: Sixty-one patients with APS (56 primary, 22/56 with obstetric events only, and 5 secondary), 146 controls including 24 aPL+ asymptomatic carriers and 73 IDC were tested on a novel hydrophobic solid phase coated with cardiolipin (CL), phosphatic acid, phosphatidylcholine, phosphatidylethanolamine, phosphatidylglycerol, phosphatidylinositol, phosphatidylserine, beta2-glycoprotein I (β2GPI), prothrombin, and annexin V. Samples were also tested by anti-CL and anti-β2GPI ELISAs and for lupus anticoagulant activity. Human monoclonal antibodies (humoAbs) against human β2GPI or PL alone were tested on the same LIA substrates in the absence or presence of human serum, purified human β2GPI or after CL-micelle absorption. Results: Comparison of LIA with the aPL-classification assays revealed good agreement for IgG/IgM aß2GPI and aCL. Anti-CL and anti-ß2GPI IgG/IgM reactivity assessed by LIA was significantly higher in patients with APS versus healthy controls and IDCs, as detected by ELISA. -

Antiphospholipid Antibodies Are Directed Against Epitopes of Oxidized Phospholipids
Antiphospholipid antibodies are directed against epitopes of oxidized phospholipids. Recognition of cardiolipin by monoclonal antibodies to epitopes of oxidized low density lipoprotein. S Hörkkö, … , W Palinski, J L Witztum J Clin Invest. 1996;98(3):815-825. https://doi.org/10.1172/JCI118854. Research Article The optimal clinical management of patients with antiphospholipid antibody syndrome (APS) is uncertain because of a lack of an underlying hypothesis to explain why antiphospholipid autoantibodies (aPL) form to such ubiquitous compounds as phospholipids (PL). In this paper, we demonstrate that many, if not most, aPL are actually directed at neoepitopes of oxidized PL, or neoepitopes generated by adduct formation between breakdown products of oxidized PL and associated proteins. Each cardiolipin (CL) molecule contains four unsaturated fatty acids and is highly susceptible to oxidation, particularly upon exposure to air. Yet, standard anticardiolipin antibodies (aCL) immunoassays routinely bind CL to microtiter wells by evaporation of the ethanol solvent overnight at 4 degrees C. Using a variety of techniques, we demonstrated that rapid oxidation occurs when CL is plated and exposed to air. Sera from apo E-deficient mice, which have high autoantibody titers to oxidized low density lipoprotein, showed a striking time-dependent increase in binding to CL that was exposed to air for increasing periods of time. Monoclonal antibodies to oxidized LDL, cloned from the apo E- deficient mice, also bound to oxidized CL. Both sera and affinity-purified aCL-IgG from APS patients bound to CL progressively as it was oxidized. However, the monoclonal antibodies from apo E-deficient mice, or sera or aCL-IgG from APS patients did not bind to a reduced CL analog […] Find the latest version: https://jci.me/118854/pdf Antiphospholipid Antibodies Are Directed against Epitopes of Oxidized Phospholipids Recognition of Cardiolipin by Monoclonal Antibodies to Epitopes of Oxidized Low Density Lipoprotein Sohvi Hörkkö,* Elizabeth Miller,* Eric Dudl,* Peter Reaven,* Linda K. -

Induction of Antiphospholipid Autoantibodies by Immunization with Beta 2 Glycoprotein I (Apolipoprotein H)
Induction of antiphospholipid autoantibodies by immunization with beta 2 glycoprotein I (apolipoprotein H). A E Gharavi, … , J Wen, K B Elkon J Clin Invest. 1992;90(3):1105-1109. https://doi.org/10.1172/JCI115927. Research Article A subset of patients with systemic lupus erythematosus has autoantibodies to acidic phospholipids. Since lipids are poor immunogens, the mechanism responsible for the induction of these antibodies is unclear. Immunization of a normal rabbit and normal mice with purified human beta 2-glycoprotein I (apolipoprotein H) resulted in the production of high levels of two non-cross-reactive antibody populations, anti-apolipoprotein H, and antiphospholipid. The antiphospholipid antibodies had binding specificities indistinguishable from autoantibodies obtained from human and murine lupus. These findings suggest a novel mechanism for the induction of antiphospholipid autoantibodies. Find the latest version: https://jci.me/115927/pdf Rapid Publication Induction of Antiphospholipid Autoantibodies by Immunization with ,B2 Glycoprotein I (Apolipoprotein H) Azzudin E. Gharavi, Lisa R. Sammaritano, Jiaying Wen, and Keith B. Elkon Division ofRheumatic Diseases, The Hospitalfor Special Surgery-Cornell University Medical Center, New York 10021 Abstract coated Staphylococcus aureus ( 16), and intrasplenic immuni- zation with Salmonella minnesota coated with lipid ( 17). aPL A subset of patients with systemic lupus erythematosus has have also been induced in experimental animals by immuniza- autoantibodies to acidic phospholipids. -

Autoantibodies Diagnostic Tools for Autoimmune Disorders
Autoantibodies Diagnostic tools for autoimmune disorders What are autoantibodies? Despite these limitations, autoantibodies are a valuable tool for the diagnosis (when considered with other clinical Autoantibodies bind non-foreign structures within us and have and laboratory information) and monitoring of many been found in most well-defined autoimmune disorders. They autoimmune disorders. also occur in other disorders with an inflammatory component and even in some malignant disorders as paraneoplastic phenomena. How is tissue injury caused in With a few important exceptions, autoantibodies have no direct autoimmune disorders? Are role in pathogenesis and their main value is as a ‘marker’ adding autoantibodies always pathological? weight to a clinical diagnoses. Much tissue damage in autoimmune diseases is probably Circulating forms of autoantibodies may be detected by mediated by T cells and their effector mechanisms, rather than assays on serum. Tissue-bound antibodies may also be by B cells and their products, autoantibodies. Systemic lupus detected by direct immunofluorescence studies of non-fixed erythematosus and other connective tissue disorders are biopsy specimens. characterised by polyclonal self-reactive B cell expansions. Normal immune system functions include the recognition of, and Do autoantibodies ever occur naturally, discrimination between, self and non-self targets and unleashing without clinical associations? of effector mechanisms, such as complement proteins, cytotoxic T cells, cytokines and other phagocytic cells onto non-self Low-level autoantibodies occur naturally and more commonly in targets. persons who are older, female, have chronic diseases and often a family history of autoimmune abnormalities. These natural Autoantibody production is a consequence of ongoing autoantibodies occur in low concentrations and have weak recognition of self targets by both T and B cells. -

Diagnostic Automation / Cortez Diagnostics
Galli et al. (3) and Viard, et al. (8) reported that anti-cardiolipin antibody AccuDiag™ derived from SLE and APS were directed to the ß2GP1 molecule coated on polystyrene plates. Koike and Matsuura showed conclusively that ß2GP1 is Beta 2 Glycoprotein 1 IgG indeed the antigen to which many anticardiolipin antibody patients are actually ELISA binding and furthermore showed that the phospholipid merely serves to link the ß2GP1 to the solid phase. (2~9) Anti-ß2GP1 autoantibodies are found in the immunoglobulin classes IgG, IgM 1495-11 and IgA. The determination of IgM antibodies is a valuable indicator in the diagnosis of beginning autoimmune disease, whereas IgG and/or IgA antibodies will be found in progressive stages of manifested autoimmune disorders. IgA antibodies are often associated with IgG antibodies. The determination of IgA See external Label 96 Tests antibodies seems to have a greater validity in thrombosis and fetal loss. (10). Indications for determination of anti ß2GP1 antibodies are: SLE, Thrombosis, Thrombocytopenia, Cerebral Ischemia, Chorea, Epilepsy, Recurrent Abortion and Intrauterine Death. Beta 2 Glycoprotein 1 IgG Test ELISA Enzyme Linked Method TEST PRINCIPLE Immunosorbent Assay Purified ß2GP1 antigens are coated on the surface of microwells. Diluted Indirect; Antigen Coated patient serum or plasma, and calibrators, are added to the wells. The Anti Principle Plate ß2GP1 specific antibodies, if present, bind to the antigens. All unbound materials are washed away. After adding enzyme conjugate, it binds to the Detection Range 6.3-200 SGU antibody-antigen complex. Excess enzyme conjugate is washed off, and TMB Sample 5µL Chromogenic substrate is added. -

Epilepsy: an Autoimmune Disease?
J Neurol Neurosurg Psychiatry 2000;69:711–714 711 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.69.6.711 on 1 December 2000. Downloaded from EDITORIAL Epilepsy: an autoimmune disease? Epilepsy may present as a symptom of many neurological LANDAU-KLEFFNER SYNDROME disorders and often an aetiological explanation cannot be This childhood syndrome, first described in 1957, is char- identified. There is growing evidence that autoimmune acterised by aphasia, behavioural problems, and seizures mechanisms might have a role in some patients. This (often of partial motor in type). The EEG recorded during includes numerous reports of the detection of theoretically sleep is diagnostic and shows focal and multifocal spikes relevant serum autoantibodies, experimental data showing and spike wave discharges predominantly in the temporal that antibodies can be epileptogenic, and a response of and parietal regions. In many cases onset can be temporally some epilepsy syndromes to immunomodulation. related to a previous infection. Autoantibodies directed The evidence for immunological mechanisms in epilepsy against brain endothelial cells and neuronal nuclear can be examined within the following three main areas: the proteins have been reported.7 Case reports of successful childhood epilepsy syndromes, epilepsy associated with treatment with IVIg treatment exist,89although this is not other immunologically mediated diseases, and the more an invariable finding. common unselected groups of patients with epilepsy. copyright. WEST’S SYNDROME (INFANTILE SPASMS) AND Childhood epilepsy syndromes LENNOX-GASTAUT SYNDROME Although both West’s syndrome and Lennox-Gastaut syn- RASMUSSEN’S ENCEPHALITIS Rasmussen’s encephalitis is a rare progressive disorder of drome have very diVerent clinical phenotypes, both syndromes have been reported to respond well to IVIg unilateral brain dysfunction, focal seizures, and inflamma- 10–13 tory histopathology. -

Acidic Phospholipids Directly Inhibit DNA Binding of Mammalian DNA Topoisomerase I
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Volume 261, number 1, 151-154 FEBS 08133 February 1990 Acidic phospholipids directly inhibit DNA binding of mammalian DNA topoisomerase I Hiro-omi Tamura, Yoji Ikegami, Katsuhiro Ono, Kazuhisa Sekimizu* and Toshiwo Andohl Department of Hygienic Chemistry, Meiji College of Pharmacy, Tanashi-shi, Tokyo 188 and *Faculty of Pharmaceutical Sciences, The University of Tokyo, Bunkyo-ku, Tokyo 113, Japan Received 22 November 1989; revised version received 2 January 1990 Inhibition of mammalian DNA topoisomerase I by phospholipids was investigated using purified enzyme. Acidic phospholipids inhibited the DNA relaxation activity of topoisomerase I whereas neutral phospholipid, phosphatidylethanolamine, did not. Accumulation of a protein-DNA cleavable complex, an intermediate which is known to accumulate upon inhibition by a specific inhibitor camptothecin, did not occur. The filter binding assay revealed that the DNA binding activity of the enzyme was inhibited by acidic phospholipids. Moreoever, direct binding of phosphatidylglycer- 01 to topoisomerase I was demonstrated. These results indicated that the inhibitory effect of acidic phospholipids on topoisomerase I was due to the loss of the DNA binding of the enzyme as a result of direct interaction between phospholipids and the enzyme. Topoisomerase I; Phospholipid 1. INTRODUCTION and phosphorylation [ 15,161 were found to modulate topoisomerase I activity in vitro. Recently eukaryotic DNA topoisomerase I has been Recently, Umekawa et al. reported that phospho- considered to have an important function in replica- lipids inhibit in vitro replication of an autonomous tion, transcription and recombination [l-7]. -

Transglutaminase 2 at the Crossroads Between Cell Death and Survival
P1: TIX/OSW P2: ABC JWBS076-05 JWBS076-Toone August 1, 2011 20:46 Printer Name: Yet to Come TRANSGLUTAMINASE 2 AT THE CROSSROADS BETWEEN CELL DEATH AND SURVIVAL MAURO PIACENTINI MANUELA D’ELETTO LAURA FALASCA MARIA GRAZIA FARRACE CARLO RODOLFO CONTENTS I. Transglutaminases A. TYPE 2 Transglutaminase B. TG2 Functions in the Cell II. Cell Death A. TG2 As a Proapoptotic Factor B. TG2 As an Antiapoptotic Factor III. Autophagy IV. TG2 In Diseases A. Inflammatory Diseases B. Intracellular Protein Inclusions-Related Disorders 1. Neurodegenerative Diseases 2. Liver Steatohepatitis 3. Cardiac Diseases V. Conclusions Acknowledgments References I. TRANSGLUTAMINASES Transglutaminases (TGases) are a peculiar family of enzymes that catal- yse the post-translational modification of proteins either through protein Advances in Enzymology and Related Areas of Molecular Biology, Volume 78. Edited by Eric J. Toone. © 2011 John Wiley & Sons, Inc. Published 2011 by John Wiley & Sons, Inc. 197 P1: TIX/OSW P2: ABC JWBS076-05 JWBS076-Toone August 1, 2011 20:46 Printer Name: Yet to Come 198 PIACENTINI MAURO ET AL. cross-linking, via ε-(␥-glutamyl) lysine bonds, or through the incorporation of primary amines, at the level peptide-bound glutamine residues [1]. The cross-linked protein products become resistant to mechanical chal- lenge and proteolytic degradation, their accumulation being found in a number of tissues, including skin and hair, in blood clotting, and wound healing [2]. In mammals, nine distinct TGases have been identified at the genomic level [3]; however, to date, only six have been characterized at the pro- tein level. These isoforms are the products of different genes that display a wide structural homology and are members of the papain-like superfam- ily of cysteine proteases [4].