Transglutaminase in Ocular Health and Pathological Processes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Technical Reports
TECHNICAL REPORTS Lipid microarrays identify key mediators of autoimmune brain inflammation Jennifer L Kanter1,2, Sirisha Narayana2, Peggy P Ho2, Ingrid Catz3, Kenneth G Warren3, Raymond A Sobel4,6, Lawrence Steinman2 & William H Robinson5,6 Recent studies suggest that increased T-cell and autoantibody against phospholipids and gangliosides contribute to the pathogenesis reactivity to lipids may be present in the autoimmune in systemic lupus erythematosus and Guillain-Barre´ syndrome, respec- demyelinating disease multiple sclerosis. To perform large-scale tively10. Despite reports of myelin-specific lipid responses in multiple multiplex analysis of antibody responses to lipids in multiple sclerosis, the role of lipid-specific autoimmunity in multiple sclerosis sclerosis, we developed microarrays composed of lipids remains controversial11. Most lipids are presented to T cells bound to 12 http://www.nature.com/naturemedicine present in the myelin sheath, including ganglioside, sulfatide, CD1 molecules and CD1 expression is increased in CNS lesions in cerebroside, sphingomyelin and total brain lipid fractions. Lipid- both multiple sclerosis and experimental autoimmune encephalomye- array analysis showed lipid-specific antibodies against sulfatide, litis (EAE)13–15. These observations led us to hypothesize that myelin sphingomyelin and oxidized lipids in cerebrospinal fluid (CSF) lipids may be target autoantigens in individuals with multiple sclerosis derived from individuals with multiple sclerosis. Sulfatide- and to develop lipid-array technology to investigate this hypothesis. specific antibodies were also detected in SJL/J mice with We developed simple, large-scale lipid microarrays for detection of acute experimental autoimmune encephalomyelitis (EAE). autoantibodies present in biological fluids such as serum and cere- Immunization of mice with sulfatide plus myelin peptide brospinal fluid (CSF). -

Surgically Induced Scleral Staphyloma
Original Article Surgically induced scleral staphyloma Yong Yao1, Ming-Zhi Zhang1, Vishal Jhanji1,2 1Joint International Eye Center of Shantou University and The Chinese University of Hong Kong, Shantou 515041, China; 2Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Hong Kong, China Contributions: (I) Conception and design: Y Yao; (II) Administrative support: MZ Zhang; (III) Provision of study materials or patients: Y Yao; (IV) Collection and assembly of data: Y Yao; (V) Data analysis and interpretation: Y Yao; V Jhanji; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Yong Yao. Shantou International Eye Center, Jinping District, Guangxia New Town, Shantou 515041, China. Email: [email protected] or [email protected]. Background: To report the clinical features of surgically induced scleral staphyloma and investigate the management. Methods: Retrospective uncontrolled study. Results: A full ophthalmological evaluation of surgically induced scleral staphyloma in four patients was performed. The first patient was a 3-year-old young girl underwent corneal dermoid resection. The second patient was a 60-year-old man underwent nasal pterygium excision and conjunctival autograft without Mitomycin C (MMC). The other two were respectively a 74-year-old woman and a 69-year-old man underwent cataract surgery. All patients performed allogeneic sclera patch graft. In the at least half a year follow-up, the best corrected visual acuity (BCVA) of all the four patients were no worse than that of preoperative. Ocular symptoms disappeared, including eye pain, foreign body sensation, and so on. Unfortunately, the fourth patient showed sclera rejection and partial dissolution at postoperative 1 month. -

Long-Term Ocular Surface Stability in Conjunctival Limbal Autograft Donor Eyes
CLINICAL SCIENCE Long-Term Ocular Surface Stability in Conjunctival Limbal Autograft Donor Eyes Albert Y. Cheung, MD,*† Enrica Sarnicola, MD,*†‡ and Edward J. Holland, MD*† (OSST) procedures can provide healthy limbal stem cells Purpose: fi – To investigate the incidence of limbal stem cell de ciency and conjunctiva to rehabilitate a damaged ocular surface.2 8 (LSCD) in donor eyes after conjunctival limbal autograft (CLAU). Conjunctival limbal autograft (CLAU) is a technique that ; Methods: An observational retrospective review was performed on transplants a portion (typically 3to6clockhours)ofthe all patients who underwent CLAU alone, combined keratolimbal healthy stem cells from an unaffected eye to the contralat- allograft with CLAU (“Modified Cincinnati Procedure”), or com- eral affected eye in individuals affected by unilateral LSCD.6 bined living-related conjunctival limbal allograft (lr-CLAL) with 7 $ Cultivated limbal epithelial transplantation (CLET) CLAU having 6 months of follow-up after surgery. The outcome 8 measures were best-corrected visual acuity (BCVA) and ocular and simple limbal epithelial transplantation (SLET) provide surface status. ex vivo and in vivo expansion of stem cells, respectively, to repopulate the ocular surface. In contrast to CLET and SLET, Results: The inclusion criteria were fulfilled by 45 patients. Of CLAU is ideal for rehabilitating severe unilateral LSCD these, 26 patients underwent CLAU, 18 underwent combined requiring combined conjunctival limbal transplantation and keratolimbal allograft/CLAU, and 1 underwent combined lr- for reconstruction of the ocular surface. Proponents of CLET CLAL/CLAU. Mean age at the time of surgery was 39.6 years. and SLET have raised concerns regarding the potential Mean logMAR preoperative BCVA was 20.08. -

Managing Ocular Surface Inflammation”
E Y 7th EDITION OLOGIES OF THE E OLOGIES OF th H 7 AT EDITION P THEA INTERNATIONAL CONTEST OF CLINICAL CASES IN PATHOLOGIES OF THE EYE THEA INTERNATIONAL CONTEST OF CLINICAL CASES IN PATHOLOGIES OF THE EYE NTEST OF CLINICAL CASES IN OF CLINICAL NTEST O This brochure is produced under the sole responsibility of the authors. Laboratoires Théa are not involved in the writing of this document. This brochure may contain MA off-label and/or not validated by health authorities information. NATIONAL C NATIONAL R HEA INTE HEA T 2018 - 2019 EDITION 2018 - 2019 EDITION MANAGING MANAGING OCULAR SURFACE OCULAR SURFACE INFLAMMATION THE BEST CLINICAL CASES FROM 22 COUNTRIES INFLAMMATION THE BEST CLINICAL CASES FROM 22 COUNTRIES WWW.THEA-TROPHY.COM CLINICAL CASES CLINICAL - BA WTROBRO0120 WWW.THEA-TROPHY.COM Laboratoires Théa • 12, rue Louis Blériot 63017 Clermont-Ferrand Cedex 2 • France T +33 4 73 98 14 36 Laboratoires Théa F +33 4 73 98 14 38 LABORATOIRES-THEA.COM th 7 EDITION This brochure is produced under the sole responsibility of the authors, Laboratoires Théa are not involved in the writing of the clinical cases. This brochure may contain MA off-label and/or not validated by health authorities information. PREFACE Mr. JEAN-FRÉDÉRIC CHIBRET TROPHY 2018-2019 the Clinical Cases 2 M. Jean-Frédéric CHIBRET President of Laboratoires Théa Théa has focused its activities on research, development and commercialization of eye-care products, but at the same time has invested in education and knowledge promotion in line with the strong Chibret family tradition. In this way, Théa supports many projects and educational activities such as the European Meeting of Young Ophthalmologists (EMYO) or its partnership with the European Board of Ophthalmology (EBO). -
Amniotic Membrane Grafts in Pediatric Corneal Limbal Dermoids with Conjunctival Eyelashes: a Case Presentation
Open Journal of Ophthalmology, 2016, 6, 191-197 http://www.scirp.org/journal/ojoph ISSN Online: 2165-7416 ISSN Print: 2165-7408 Amniotic Membrane Grafts in Pediatric Corneal Limbal Dermoids with Conjunctival Eyelashes: A Case Presentation Larisa Akah Che1, Linda A. Morgan2, Donny W. Suh2,3 1University of Nebraska Medical Center, Omaha, NE, USA 2Children’s Hospital & Medical Center, Omaha, NE, USA 3Department of Ophthalmology and Visual Sciences, Truhlsen Eye Institute, University of Nebraska Medical Center, Omaha, NE, USA How to cite this paper: Che, L.A., Morgan, Abstract L.A. and Suh, D.W. (2016) Amniotic Mem- brane Grafts in Pediatric Corneal Limbal Purpose: To report a case of a pediatric corneal limbal dermoid with eyelashes and Dermoids with Conjunctival Eyelashes: A to describe post-operative changes after excision with reconstruction using amniotic Case Presentation. Open Journal of Oph- membrane grafting, sutures and fibrinogen-thrombin glue. Case Report: One pedia- thalmology, 6, 191-197. http://dx.doi.org/10.4236/ojoph.2016.64027 tric patient was identified with a grade II infratemporal corneal-limbal dermoid with conjunctival eyelashes. The dermoid was surgically excised and the cornea recon- Received: August 23, 2016 structed with amniotic membrane using sutures and fibrinogen/thrombin glue. Pre- Accepted: October 11, 2016 operative and postoperative measurement of astigmatism, anisometropia and pres- Published: October 14, 2016 ence of exposure keratopathy were performed. Copyright © 2016 by authors and Scientific Research Publishing Inc. Keywords This work is licensed under the Creative Commons Attribution International Corneal Limbal Dermoid, Amniotic Membrane Graft, Choriostoma License (CC BY 4.0). http://creativecommons.org/licenses/by/4.0/ Open Access 1. -

Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (Membrane/Cardiolipin/Gangliosides/Ca + +/Phase Transition) J
Proc. Nat. Acad. Sci. USA Vol. 70, No. 5, pp. 1406-1409, May 1973 Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (membrane/cardiolipin/gangliosides/Ca + +/phase transition) J. M. BOGGS AND J. C. HSIA Department of Pharmacology, Faculty of Medicine, University of Toronto, Toronto M5S 1A8 Ontario, Canada Communicated by David E. Green, March 5, 1973 ABSTRACT The acyl chain of spin-labeled fatty acids preferred orientation in cylindrical and spherical micellar intercalates between the lipid hydrocarbon chains in hexag- phases with the long axis parallel to the lipid acyl chains, onal and micellar phases with the carboxyl group anchored at the lipid water interface. The spectra are resulting in spectra characteristic of rapid anisotropic motion characteristic of anisotropic motion and cannot be dis- and (b) there is a fluidity gradient in the hexagonal phase, tinguished from the spectra of these probes in lamellar i.e., the motional freedom of the acyl chains increases toward dispersions. In the hexagonal and micellar phases the the terminal methyl group as has been observed for the molecular motion of the spin label increases as it is moved further away from the carboxyl group, similar to the be- lamellar phase (2, 4, 5). havior in the lamellar phase (Jost et al. (1971) J. Mol. Biol. 59, 77-98). The similarity in packing of the acyl chains in MATERIALS AND METHODS the hexagonal and lamellar phases suggests that localized 5-Doxyl-palmitic acid [1(10,3)] and 8-doxyl-palmitic acid regions of hexagonal phase are compatible with a bilayer [I(7,6)] were prepared according to the method of Hubbell matrix. -

Ethical Issues in Living-Related Corneal Tissue Transplantation
Viewpoint Ethical issues in living-related corneal J Med Ethics: first published as 10.1136/medethics-2018-105146 on 23 May 2019. Downloaded from tissue transplantation Joséphine Behaegel, 1,2 Sorcha Ní Dhubhghaill,1,2 Heather Draper3 1Department of Ophthalmology, ABSTRact injury, typically chemical burns, chronic inflamma- Antwerp University Hospital, The cornea was the first human solid tissue to be tion and certain genetic diseases, the limbal stem Edegem, Belgium 2 transplanted successfully, and is now a common cells may be lost and the cornea becomes vascula- Faculty of Medicine and 5 6 Health Sciences, Dept of procedure in ophthalmic surgery. The grafts come from rised and opaque, leading to blindness (figure 1). Ophthalmology, Visual Optics deceased donors. Corneal therapies are now being In such cases, standard corneal transplants fail and Visual Rehabilitation, developed that rely on tissue from living-related donors. because of the inability to maintain a healthy epithe- University of Antwerp, Wilrijk, This presents new ethical challenges for ophthalmic lium. Limbal stem cell transplantation is designed to Belgium 3Division of Health Sciences, surgeons, who have hitherto been somewhat insulated address this problem by replacing the damaged or Warwick Medical School, from debates in transplantation and donation ethics. lost limbal stem cells (LSC) and restoring the ocular University of Warwick, Coventry, This paper provides the first overview of the ethical surface, which in turn increases the success rates of United Kingdom considerations generated by ocular tissue donation subsequent sight-restoring corneal transplants.7 8 from living donors and suggests how these might Limbal stem cell donations only entail the removal Correspondence to be addressed in practice. -
Technical Data Sheet
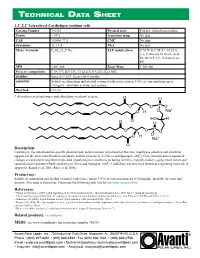
TECHNICAL DA T A SHEE T 1,1’,2,2’ Tetraoleoyl Cardiolipin (sodium salt) Catalog Number 710335 Physical state Powder; chloroform solution Purity > 99% Transition temp. No data CAS 115404-77-8 CMC No data Synonyms 18:1 CA PKA No data Molec. Formula C81H148O17P2Na2 TLC mobile phase C:M:W & C:M:A*, 65:25:4, v/v; C:Hexane:M:Acetic Acid 50:30:10:5, v/v, if want to see PG MW 1,501.000 Exact Mass 1,501.000 Percent composition C 64.77% H 9.93% O 18.11% P 4.12% Na 3.06% Stability Store in <-20°C freezer for 6 months Solubility Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Web link 710335 * chloroform:methanol:water and chloroform:methanol:acetone Description: Cardiolipin, the mitochondrial-specific phospholipid, helps maintain mitochondrial function, membrane potential and structural support for the inner mitochondrial membrane and the proteins in it (Chicco and Sparagna, 2007). Concentration and composition changes of cardiolipin have been implicated in pathological conditions including ischemia, hypothyroidism, aging, heart failure and cardioskeletal myopathy (Barth syndrome) (Chicco and Sparagna, 2007). Cardiolipin has also been shown as a signaling molecule in apoptosis (Kagan et al, 2006; Ritov et al, 2006). Product use: Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Also used in liposomes. Please use the following web link for liposome preparation. References: • Huang and Frohman (2009). -

Antiphospholipid Antibodies Detected by Line Immunoassay Differentiate
Roggenbuck et al. Arthritis Research & Therapy (2016) 18:111 DOI 10.1186/s13075-016-1018-x RESEARCH ARTICLE Open Access Antiphospholipid antibodies detected by line immunoassay differentiate among patients with antiphospholipid syndrome, with infections and asymptomatic carriers Dirk Roggenbuck1,2*†, Maria Orietta Borghi3,4†, Valentina Somma2, Thomas Büttner5, Peter Schierack2, Katja Hanack6, Claudia Grossi4, Caterina Bodio3, Paolo Macor7, Philipp von Landenberg8, Francesco Boccellato9, Michael Mahler10 and Pier Luigi Meroni3,4 Abstract Background: Antiphospholipid antibodies (aPL) can be detected in asymptomatic carriers and infectious patients. The aim was to investigate whether a novel line immunoassay (LIA) differentiates between antiphospholipid syndrome (APS) and asymptomatic aPL+ carriers or patients with infectious diseases (infectious diseases controls (IDC)). Methods: Sixty-one patients with APS (56 primary, 22/56 with obstetric events only, and 5 secondary), 146 controls including 24 aPL+ asymptomatic carriers and 73 IDC were tested on a novel hydrophobic solid phase coated with cardiolipin (CL), phosphatic acid, phosphatidylcholine, phosphatidylethanolamine, phosphatidylglycerol, phosphatidylinositol, phosphatidylserine, beta2-glycoprotein I (β2GPI), prothrombin, and annexin V. Samples were also tested by anti-CL and anti-β2GPI ELISAs and for lupus anticoagulant activity. Human monoclonal antibodies (humoAbs) against human β2GPI or PL alone were tested on the same LIA substrates in the absence or presence of human serum, purified human β2GPI or after CL-micelle absorption. Results: Comparison of LIA with the aPL-classification assays revealed good agreement for IgG/IgM aß2GPI and aCL. Anti-CL and anti-ß2GPI IgG/IgM reactivity assessed by LIA was significantly higher in patients with APS versus healthy controls and IDCs, as detected by ELISA. -

Antiphospholipid Antibodies Are Directed Against Epitopes of Oxidized Phospholipids
Antiphospholipid antibodies are directed against epitopes of oxidized phospholipids. Recognition of cardiolipin by monoclonal antibodies to epitopes of oxidized low density lipoprotein. S Hörkkö, … , W Palinski, J L Witztum J Clin Invest. 1996;98(3):815-825. https://doi.org/10.1172/JCI118854. Research Article The optimal clinical management of patients with antiphospholipid antibody syndrome (APS) is uncertain because of a lack of an underlying hypothesis to explain why antiphospholipid autoantibodies (aPL) form to such ubiquitous compounds as phospholipids (PL). In this paper, we demonstrate that many, if not most, aPL are actually directed at neoepitopes of oxidized PL, or neoepitopes generated by adduct formation between breakdown products of oxidized PL and associated proteins. Each cardiolipin (CL) molecule contains four unsaturated fatty acids and is highly susceptible to oxidation, particularly upon exposure to air. Yet, standard anticardiolipin antibodies (aCL) immunoassays routinely bind CL to microtiter wells by evaporation of the ethanol solvent overnight at 4 degrees C. Using a variety of techniques, we demonstrated that rapid oxidation occurs when CL is plated and exposed to air. Sera from apo E-deficient mice, which have high autoantibody titers to oxidized low density lipoprotein, showed a striking time-dependent increase in binding to CL that was exposed to air for increasing periods of time. Monoclonal antibodies to oxidized LDL, cloned from the apo E- deficient mice, also bound to oxidized CL. Both sera and affinity-purified aCL-IgG from APS patients bound to CL progressively as it was oxidized. However, the monoclonal antibodies from apo E-deficient mice, or sera or aCL-IgG from APS patients did not bind to a reduced CL analog […] Find the latest version: https://jci.me/118854/pdf Antiphospholipid Antibodies Are Directed against Epitopes of Oxidized Phospholipids Recognition of Cardiolipin by Monoclonal Antibodies to Epitopes of Oxidized Low Density Lipoprotein Sohvi Hörkkö,* Elizabeth Miller,* Eric Dudl,* Peter Reaven,* Linda K. -

Amniotic Membrane Transplantation for the Ocular Surface
Name of Blue Advantage Policy: Amniotic Membrane Transplantation for the Ocular Surface Policy #: 624 Latest Review Date: February 2021 Category: Medical Policy Grade: C BACKGROUND: Blue Advantage medical policy does not conflict with Local Coverage Determinations (LCDs), Local Medical Review Policies (LMRPs) or National Coverage Determinations (NCDs) or with coverage provisions in Medicare manuals, instructions or operational policy letters. In order to be covered by Blue Advantage the service shall be reasonable and necessary under Title XVIII of the Social Security Act, Section 1862(a)(1)(A). The service is considered reasonable and necessary if it is determined that the service is: 1. Safe and effective; 2. Not experimental or investigational*; 3. Appropriate, including duration and frequency that is considered appropriate for the service, in terms of whether it is: • Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member; • Furnished in a setting appropriate to the patient’s medical needs and condition; • Ordered and furnished by qualified personnel; • One that meets, but does not exceed, the patient’s medical need; and • At least as beneficial as an existing and available medically appropriate alternative. *Routine costs of qualifying clinical trial services with dates of service on or after September 19, 2000 which meet the requirements of the Clinical Trials NCD are considered reasonable and necessary by Medicare. Providers should bill Original Medicare for covered services that are related to clinical trials that meet Medicare requirements (Refer to Medicare National Coverage Determinations Manual, Chapter 1, Section 310 and Medicare Claims Processing Manual Chapter 32, Sections 69.0-69.11). -
Changes in Lipid Profile of Keratinocytes from Rat Skin
antioxidants Article Changes in Lipid Profile of Keratinocytes from Rat Skin Exposed to Chronic UVA or UVB Radiation and Topical Application of Cannabidiol Wojciech Łuczaj 1,* , Maria do Rosário Domingues 2,3 , Pedro Domingues 2 and El˙zbietaSkrzydlewska 1 1 Department of Analytical Chemistry, Medical University of Bialystok, Mickiewicza 2d, 15-222 Bialystok, Poland; [email protected] 2 Mass Spectrometry Center, LAQV, Department of Chemistry, Campus Universitário de Santiago, University of Aveiro, 3810-193 Aveiro, Portugal; [email protected] (M.d.R.D.); [email protected] (P.D.) 3 CESAM, Department of Chemistry, University of Aveiro, Campus Universitário de Santiago, 3810-193 Aveiro, Portugal * Correspondence: [email protected]; Tel.: +48-857485882 Received: 1 November 2020; Accepted: 23 November 2020; Published: 25 November 2020 Abstract: UV radiation is a well-established environmental risk factor known to cause oxidative stress and disrupt the metabolism of keratinocyte phospholipids. Cannabidiol (CBD) is a phytocannabinoid with anti-inflammatory and antioxidant effects. In this study, we examined changes in the keratinocyte phospholipid profile from nude rat skin exposed to UVA and UVB radiation that was also treated topically with CBD. UVA and UVB radiation promoted up-regulation of phosphatidylcholines (PC), lysophosphatidylcholines (LPC), phosphatidylethanolamines (PE) and down-regulation of sphingomyelin (SM) levels and enhanced the activity of phospholipase A2 (PLA2) and sphingomyelinase (SMase). Application of CBD to the skin of control rats led to down-regulation of SM and up-regulation of SMase activity. After CBD treatment of rats irradiated with UVA or UVB, SM was up-regulated and down-regulated, respectively, while ceramide (CER) levels and SMase activity were down-regulated and up-regulated, respectively.