Autoantibodies Diagnostic Tools for Autoimmune Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lactoferrin and Its Detection Methods: a Review
nutrients Review Lactoferrin and Its Detection Methods: A Review Yingqi Zhang, Chao Lu and Jin Zhang * Department of Chemical and Biochemical Engineering, University of Western Ontario, London, ON N6A 5B9, Canada; [email protected] (Y.Z.); [email protected] (C.L.) * Correspondence: [email protected] Abstract: Lactoferrin (LF) is one of the major functional proteins in maintaining human health due to its antioxidant, antibacterial, antiviral, and anti-inflammatory activities. Abnormal levels of LF in the human body are related to some serious diseases, such as inflammatory bowel disease, Alzheimer’s disease and dry eye disease. Recent studies indicate that LF can be used as a biomarker for diagnosis of these diseases. Many methods have been developed to detect the level of LF. In this review, the biofunctions of LF and its potential to work as a biomarker are introduced. In addition, the current methods of detecting lactoferrin have been presented and discussed. We hope that this review will inspire efforts in the development of new sensing systems for LF detection. Keywords: lactoferrin; biomarkers; immunoassay; instrumental analysis; sensor 1. Introduction Lactoferrin (known as lactotransferrin, LF), with a molecular weight of about 80 kDa, is a functional glycoprotein, which contains about 690 amino acid residues. It was first isolated from bovine milk by Sorensen in 1939 and was first isolated from human milk by Citation: Zhang, Y.; Lu, C.; Zhang, J. Johanson in 1960 [1,2]. The three-dimensional structure of LF has been unveiled by high Lactoferrin and Its Detection resolution X-ray crystallographic analysis, and it consists of two homologous globular lobes Methods: A Review. -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -
Domino Effect in a Patient with Epstein-Barr Virus Infection and Autoimmunity: a Case Report Case Report Appointments Scheduled
International Journal of Case Report Clinical Rheumatology Domino effect in a patient with Epstein- Barr Virus infection and autoimmunity: A case report The link between autoimmune diseases and viral infections has been characterized, but specific Margarite Matossian, Carrie mechanisms behind this association remain a current area of investigation. Whether viral infections Crook, Alec Goldberg, Anna trigger or unmask autoimmunity, or if the pathologies occur concurrently, is not yet completely Stathopoulos, Justin Tien, understood. Specifically, Epstein - Barr virus (EBV) is implicated in several autoimmune disorders, Sheela Sheth, Osaid Saqqa & including Systemic Lupus Erythematosus (SLE). It is hypothesized that common immunologic Christopher Dale Shamburger* pathways are activated in the two pathologic states. This case report is an example of this confusing Department of Medicine, Tulane University presentation, and the importance of recognizing the association between autoimmunity and viral Health Sciences Center, New Orleans LA infections. This patient presented with symptoms concerning for SLE and hepatic autoimmunity 70115, USA with serology suggesting a recent infection with EBV. Given this complicated presentation, it is *Author for correspondence: difficult to determine which disease state presented first in patients with evidence of both SLE and EBV infection and whether this information is clinically relevant for ongoing treatment and [email protected] monitoring. Here, we provide an in-depth discussion of current genomic and immunological research that supports the associations amongst these disease pathologies. Introduction by an intricate psychiatric history. Then Autoimmune diseases have increased in we discuss the contribution of infection to frequency in industrialized countries over autoimmune disease states and important recent years [1]. The etiology of autoimmune distinctions between autoimmune diseases diseases, a self-reactive adaptive immune and autoinflammatory responses. -

Attenuation of Ganglioside GM1 Accumulation in the Brain of GM1 Gangliosidosis Mice by Neonatal Intravenous Gene Transfer
Gene Therapy (2003) 10, 1487–1493 & 2003 Nature Publishing Group All rights reserved 0969-7128/03 $25.00 www.nature.com/gt RESEARCH ARTICLE Attenuation of ganglioside GM1 accumulation in the brain of GM1 gangliosidosis mice by neonatal intravenous gene transfer N Takaura1, T Yagi2, M Maeda2, E Nanba3, A Oshima4, Y Suzuki5, T Yamano1 and A Tanaka1 1Department of Pediatrics, Osaka City University Graduate School of Medicine, Osaka, Japan; 2Department of Neurobiology and Anatomy, Osaka City University Graduate School of Medicine, Osaka, Japan; 3Gene Research Center, Tottori University, Yonago, Japan; 4Department of Pediatrics, Takagi Hospital, Saitama, Japan; and 5Pediatrics, Clinical Research Center, Nasu Institute for Developmental Disabilities, International University of Health and Welfare, Ohtawara, Japan A single intravenous injection with 4 Â 107 PFU of recombi- ganglioside GM1 was above the normal range in all treated nant adenovirus encoding mouse b-galactosidase cDNA to mice, which was speculated to be the result of reaccumula- newborn mice provided widespread increases of b-galacto- tion. However, the values were still definitely lower in most of sidase activity, and attenuated the development of the the treated mice than those in untreated mice. In the disease including the brain at least for 60 days. The b- histopathological study, X-gal-positive cells, which showed galactosidase activity showed 2–4 times as high a normal the expression of exogenous b-galactosidase gene, were activity in the liver and lung, and 50 times in the heart. In the observed in the brain. It is noteworthy that neonatal brain, while the activity was only 10–20% of normal, the administration via blood vessels provided access to the efficacy of the treatment was distinct. -

Monoclonal Antibody Playbook
Federal Response to COVID-19: Monoclonal Antibody Clinical Implementation Guide Outpatient administration guide for healthcare providers 2 SEPTEMBER 2021 1 Introduction to COVID-19 Monoclonal Antibody Therapy 2 Overview of Emergency Use Authorizations 3 Site and Patient Logistics Site preparation Patient pathways to monoclonal administration 4 Team Roles and Responsibilities Leadership Administrative Clinical Table of 5 Monoclonal Antibody Indications and Administration Indications Contents Preparation Administration Response to adverse events 6 Supplies and Resources Infrastructure Administrative Patient Intake Administration 7 Examples: Sites of Administration and Staffing Patterns 8 Additional Resources 1 1. Introduction to Monoclonal Therapy 2 As of 08/13/21 Summary of COVID-19 Therapeutics 1 • No Illness . Health, no infections • Exposed Asymptomatic Infected . Scope of this Implementation Guide . Not hospitalized, no limitations . Monoclonal Antibodies for post-exposure prophylaxis (Casirivimab + Imdevimab (RGN)) – EUA Issued. • Early Symptomatic . Scope of this Implementation Guide . Not hospitalized, with limitations . Monoclonal Antibodies for treatment (EUA issued): Bamlanivimab + Etesevimab1 (Lilly) Casirivimab + Imdevimab (RGN) Sotrovimab (GSK/Vir) • Hospital Adminission. Treated with Remdesivir (FDA Approved) or Tocilizumab (EUA Issued) . Hospitalized, no acute medical problems . Hospitalized, not on oxygen . Hospitlaized, on oxygen • ICU Admission . Hospitalized, high flow oxygen, non-invasive ventilation -
Technical Reports
TECHNICAL REPORTS Lipid microarrays identify key mediators of autoimmune brain inflammation Jennifer L Kanter1,2, Sirisha Narayana2, Peggy P Ho2, Ingrid Catz3, Kenneth G Warren3, Raymond A Sobel4,6, Lawrence Steinman2 & William H Robinson5,6 Recent studies suggest that increased T-cell and autoantibody against phospholipids and gangliosides contribute to the pathogenesis reactivity to lipids may be present in the autoimmune in systemic lupus erythematosus and Guillain-Barre´ syndrome, respec- demyelinating disease multiple sclerosis. To perform large-scale tively10. Despite reports of myelin-specific lipid responses in multiple multiplex analysis of antibody responses to lipids in multiple sclerosis, the role of lipid-specific autoimmunity in multiple sclerosis sclerosis, we developed microarrays composed of lipids remains controversial11. Most lipids are presented to T cells bound to 12 http://www.nature.com/naturemedicine present in the myelin sheath, including ganglioside, sulfatide, CD1 molecules and CD1 expression is increased in CNS lesions in cerebroside, sphingomyelin and total brain lipid fractions. Lipid- both multiple sclerosis and experimental autoimmune encephalomye- array analysis showed lipid-specific antibodies against sulfatide, litis (EAE)13–15. These observations led us to hypothesize that myelin sphingomyelin and oxidized lipids in cerebrospinal fluid (CSF) lipids may be target autoantigens in individuals with multiple sclerosis derived from individuals with multiple sclerosis. Sulfatide- and to develop lipid-array technology to investigate this hypothesis. specific antibodies were also detected in SJL/J mice with We developed simple, large-scale lipid microarrays for detection of acute experimental autoimmune encephalomyelitis (EAE). autoantibodies present in biological fluids such as serum and cere- Immunization of mice with sulfatide plus myelin peptide brospinal fluid (CSF). -

Antibody Testing in Peripheral Neuropathies Steven Vernino, MD, Phd*, Gil I
Neurol Clin 25 (2007) 29–46 Antibody Testing in Peripheral Neuropathies Steven Vernino, MD, PhD*, Gil I. Wolfe, MD Department of Neurology, University of Texas Southwestern Medical Center, Dallas, TX, USA Causes of peripheral neuropathy (PN) include a wide range of genetic, toxic, metabolic, and inflammatory disorders. Several PNs have an autoim- mune basis, either as a consequence of systemic autoimmune disease, an au- toimmune disorder specifically targeting peripheral nerve or ganglia, or a remote effect of malignancy. Several clinical presentations are distinctive for the autoimmune neuropathies. Subacute progression, asymmetric or multifocal deficits, and selective involvement of motor, sensory, or auto- nomic nerves are clues suggesting an autoimmune, inflammatory cause. The clinical presentation, however, may be indistinguishable from other forms of chronic length-dependent sensorimotor PN. Antibodies against specific glycolipids or glycoproteins, such as anti- GM1 and anti–myelin-associated glycoprotein (MAG), are associated with inflammatory (often demyelinating) peripheral nerve syndromes. In some cases, these antibodies identify motor or sensory neuropathies that are responsive to immunotherapy [1–3] or those with a different prognosis [4,5]. Antineuronal nuclear and cytoplasmic antibodies (such as anti-Hu and CRMP-5) help identify patients who have paraneoplastic neuropathy resulting from remote immunologic effects of malignancy [6,7]. Various other serologic tests, although less specific, can be used to provide clues about the presence of systemic autoimmune disease that can affect the nerves. These include serologic markers for Sjo¨gren’s syndrome (SS), rheu- matoid arthritis, celiac disease, and systemic vasculitides (such as Churg- Strauss syndrome) [8,9]. Because the cause of acquired neuropathies often is obscure, autoanti- body testing can be of great diagnostic value in identifying autoimmune * Corresponding author. -

Improvement of Spontaneous Alternation Behavior Deficit by Activation Ofα4β2 Nicotinic Acetylcholine Receptor Signaling in the Ganglioside GM3-Deficient Mice
Biomedical Research 34 (4) 189-195, 2013 Improvement of spontaneous alternation behavior deficit by activation of α4β2 nicotinic acetylcholine receptor signaling in the ganglioside GM3- deficient mice 1 1 2 1 2 1 Kimie NIIMI , Chieko NISHIOKA , Tomomi MIYAMOTO , Eiki TAKAHASHI , Ichiro MIYOSHI , Chitoshi ITAKURA , 3, 4 and Tadashi YAMASHITA 1 Riken Brain Science Institute, Saitama 351-0198, Japan; 2 Graduate School of Medical Sciences, Nagoya City University, Nagoya 467- 8601, Japan; 3 Graduate School of Veterinary Medicine, Azabu University, Sagamihara 252-5201, Japan; and 4 World Class University Program, Kyungpook National University School of Medicine, Daegu, South Korea (Received 13 May 2013; and accepted 17 June 2013) ABSTRACT We have reported that in ganglioside GM3-deficient (GM3−/−) mice, spontaneous alternation be- havior assessed by a Y-maze task was significantly lower, and total arm entries were significantly higher than in wild-type mice. The objective of the present study was to examine the role of nico- tinic acetylcholine receptor (nAChR) signaling in impairment of spontaneous alternation behavior of GM3−/− mice. Nicotine treatment (0.3, 1.0 mg/kg, s.c.) dose dependently improved the sponta- neous alternation deficit without affecting total arm entries in GM3−/− mice. The nicotine-induced (1.0 mg/kg, s.c.) improvement was significantly abolished by the nAChR antagonist mecamyla- mine (1.0 mg/kg, i.p.). The α4β2 nAChR antagonist dihydro-β-erythroidine (2.5, 10.0 mg/kg, i.p.) dose dependently counteracted the nicotine-induced improvement of spontaneous alternation in GM3−/− mice, whereas the α7 nAChR antagonist methyllycaconitine (2.5, 10.0 mg/kg, i.p.) did not. -

Pediatric Motor Inflammatory Neuropathy: the Role Of
brain sciences Case Report Pediatric Motor Inflammatory Neuropathy: The Role of Antiphospholipid Antibodies Claudia Brogna 1,2,*, Marco Luigetti 3 , Giulia Norcia 1, Roberta Scalise 1, Gloria Ferrantini 1, Beatrice Berti 1, Domenico M. Romeo 4, Raffaele Manna 5, Eugenio Mercuri 1 and Marika Pane 1 1 Pediatric Neurology and Nemo Clinical Centre, Fondazione Policlinico Universitario A. Gemelli IRCSS, Università Cattolica del Sacro Cuore, 00168 Roma, Italy; [email protected] (G.N.); [email protected] (R.S.); [email protected] (G.F.); [email protected] (B.B.); [email protected] (E.M.); [email protected] (M.P.) 2 Pediatric Neuropsichiatric Unit, ASL, 83100 Avellino, Italy 3 Institute of Neurology, Fondazione Policlinico Universitario A. Gemelli IRCSS, Università Cattolica del sacro Cuore, 00168 Roma, Italy; [email protected] 4 Pediatric Neurology, Fondazione Policlinico Universitario A. Gemelli IRCSS, Università Cattolica del Sacro Cuore, 00168 Roma, Italy; [email protected] 5 Periodic Fevers Research Centre and rare disease. Department of Internal Medicine, Fondazione Policlinico Universitario A. Gemelli IRCSS, Università Cattolica del Sacro Cuore, 00168 Roma, Italy; raff[email protected] * Correspondence: [email protected] Received: 4 February 2020; Accepted: 5 March 2020; Published: 7 March 2020 Abstract: We report the clinical case of a nine-year-old girl who presented with progressive motor neuropathy, revealed via the detection of a higher delay in F-wave recording using digitalized nerve conduction/electromyography. Since the lupus anticoagulant (LAC) positivity, detected using diluted Russell viper venom time (dRVVT), switched to persistent serological anticardiolipin immunoglobulin G (IgG) positivity, a possible non-thrombotic antiphospholipid antibody (aPL)-related clinical manifestation was suspected, and intravenous immunoglobulin treatment (IVIG) was started. -
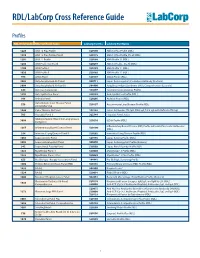
RDL/Labcorp Cross Reference Guide
RDL/LabCorp Cross Reference Guide Profiles RDL Order Code RDL Test/Panel Name LabCorp Test No. LabCorp Test Name 1228 ANA 12 Plus Profile 520180 ANA 12 Plus Profile (RDL) 1230 ANA 12 Plus Profile, Do All 520175 ANA 12 Plus Profile, Do all (RDL) 1201 ANA 12 Profile 520188 ANA Profile 12 (RDL) 1206 ANA Profile 12, Do All 520299 ANA 12 Profile , Do All (RDL) 1100 ANA Profile I 520185 ANA Profile 11 (RDL) 1020 ANA Profile II 520185 ANA Profile 11 (RDL) 994 ANCA Panel 520149 ANCA Profile (RDL) 3003 Antiphospholipid Ab Panel I 500711 Lupus Anticoagulant/Cardiolipin Antibody (Esoterix) 3004 Antiphospholipid Ab Panel II 504400 Antiphospholipid Syndrome (APS), Comprehensive (Esoterix) 644 Anti-Saccharomyces 164657 Saccharomyces cerevisiae Profile 1292 Anti-Synthetase Panel 520193 Anti-Synthetase Profile (RDL) 996 Arthritis Panel 520205 Arthritis Profile (RDL) Autoimmune Liver Disease Panel, 558 520197 Autoimmune Liver Disease Profile (RDL) Comprehensive 1044 Celiac Disease Ab Panel 165142 Celiac Antibodies tTG IgA, EMA IgA, Total IgA with Reflex to tTG IgG 705 Hepatitis Panel II 322744 Hepatitis Panel, Acute ILDdxComplete (Interstitial Lung Disease 3008 520210 ILDdx Profile (RDL) Complete) Inflammatory Bowel Disease (IBD) Profile with Anti-Pancreatic Antibodies 1265 Inflammatory Bowel Disease Panel 520190 (RDL) 354 Interstitial Lung Disease Panel II 520202 Interstitial Lung Disease Profile (RDL) 1065 Lupus Activity Panel 520195 Lupus Activity Profile (RDL) 3002 Lupus Anticoagulant Panel 500070 Lupus Anticoagulant Profile (Esoterix) 342 Lupus Renal -

Transglutaminase in Ocular Health and Pathological Processes
perim Ex en l & ta a l ic O p in l h t C h f Journal of Clinical & Experimental a Tong et al. J Clinic Experiment Ophthalmol 2011, S:2 o l m l a o n l DOI: 10.4172/2155-9570.S2-002 r o g u y o J Ophthalmology ISSN: 2155-9570 ResearchResearch Article Article OpenOpen Access Access Recent Advances: Transglutaminase in Ocular Health and Pathological Processes Louis Tong1,2,3*, Evelyn Png2, Wanwen Lan2 and Andrea Petznick2 1Singapore National Eye Center, Singapore 2Singapore Eye Research Institute, Singapore 3Duke-NUS Graduate Medical School, Singapore Abstract Transglutaminase (TG) is a diverse class of crosslinking enzymes involved in the regulation of cytokine production, endocytosis, cell adhesion, migration, apoptosis and autophagy. It has been implicated in inflammatory diseases, neurodegenerative processes and cancer. The eye is a specialized organ which subserves the important function of vision and has distinctive physiological and anatomical properties that differ from other body tissues. Understanding of the roles of various TGs in the eye therefore require studies specific to cells and tissues of ocular origin. We review the advances in TG research in ocular diseases, including pterygium, glaucoma, cataract and proliferative vitreoretinopathy. TG1 is a molecule important for keratinisation in many cicatrizing diseases of the ocular surface, including keratoconjunctivitis sicca. TG2, with multiple functions, has been shown to be important in inflammation and cell adhesion in various ocular diseases. The results of TG research in each region of the eye are critically assessed and the implications of these studies in the treatment of ocular diseases are discussed. -

Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (Membrane/Cardiolipin/Gangliosides/Ca + +/Phase Transition) J
Proc. Nat. Acad. Sci. USA Vol. 70, No. 5, pp. 1406-1409, May 1973 Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (membrane/cardiolipin/gangliosides/Ca + +/phase transition) J. M. BOGGS AND J. C. HSIA Department of Pharmacology, Faculty of Medicine, University of Toronto, Toronto M5S 1A8 Ontario, Canada Communicated by David E. Green, March 5, 1973 ABSTRACT The acyl chain of spin-labeled fatty acids preferred orientation in cylindrical and spherical micellar intercalates between the lipid hydrocarbon chains in hexag- phases with the long axis parallel to the lipid acyl chains, onal and micellar phases with the carboxyl group anchored at the lipid water interface. The spectra are resulting in spectra characteristic of rapid anisotropic motion characteristic of anisotropic motion and cannot be dis- and (b) there is a fluidity gradient in the hexagonal phase, tinguished from the spectra of these probes in lamellar i.e., the motional freedom of the acyl chains increases toward dispersions. In the hexagonal and micellar phases the the terminal methyl group as has been observed for the molecular motion of the spin label increases as it is moved further away from the carboxyl group, similar to the be- lamellar phase (2, 4, 5). havior in the lamellar phase (Jost et al. (1971) J. Mol. Biol. 59, 77-98). The similarity in packing of the acyl chains in MATERIALS AND METHODS the hexagonal and lamellar phases suggests that localized 5-Doxyl-palmitic acid [1(10,3)] and 8-doxyl-palmitic acid regions of hexagonal phase are compatible with a bilayer [I(7,6)] were prepared according to the method of Hubbell matrix.