Technical Reports
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Attenuation of Ganglioside GM1 Accumulation in the Brain of GM1 Gangliosidosis Mice by Neonatal Intravenous Gene Transfer
Gene Therapy (2003) 10, 1487–1493 & 2003 Nature Publishing Group All rights reserved 0969-7128/03 $25.00 www.nature.com/gt RESEARCH ARTICLE Attenuation of ganglioside GM1 accumulation in the brain of GM1 gangliosidosis mice by neonatal intravenous gene transfer N Takaura1, T Yagi2, M Maeda2, E Nanba3, A Oshima4, Y Suzuki5, T Yamano1 and A Tanaka1 1Department of Pediatrics, Osaka City University Graduate School of Medicine, Osaka, Japan; 2Department of Neurobiology and Anatomy, Osaka City University Graduate School of Medicine, Osaka, Japan; 3Gene Research Center, Tottori University, Yonago, Japan; 4Department of Pediatrics, Takagi Hospital, Saitama, Japan; and 5Pediatrics, Clinical Research Center, Nasu Institute for Developmental Disabilities, International University of Health and Welfare, Ohtawara, Japan A single intravenous injection with 4 Â 107 PFU of recombi- ganglioside GM1 was above the normal range in all treated nant adenovirus encoding mouse b-galactosidase cDNA to mice, which was speculated to be the result of reaccumula- newborn mice provided widespread increases of b-galacto- tion. However, the values were still definitely lower in most of sidase activity, and attenuated the development of the the treated mice than those in untreated mice. In the disease including the brain at least for 60 days. The b- histopathological study, X-gal-positive cells, which showed galactosidase activity showed 2–4 times as high a normal the expression of exogenous b-galactosidase gene, were activity in the liver and lung, and 50 times in the heart. In the observed in the brain. It is noteworthy that neonatal brain, while the activity was only 10–20% of normal, the administration via blood vessels provided access to the efficacy of the treatment was distinct. -

Antibody Testing in Peripheral Neuropathies Steven Vernino, MD, Phd*, Gil I
Neurol Clin 25 (2007) 29–46 Antibody Testing in Peripheral Neuropathies Steven Vernino, MD, PhD*, Gil I. Wolfe, MD Department of Neurology, University of Texas Southwestern Medical Center, Dallas, TX, USA Causes of peripheral neuropathy (PN) include a wide range of genetic, toxic, metabolic, and inflammatory disorders. Several PNs have an autoim- mune basis, either as a consequence of systemic autoimmune disease, an au- toimmune disorder specifically targeting peripheral nerve or ganglia, or a remote effect of malignancy. Several clinical presentations are distinctive for the autoimmune neuropathies. Subacute progression, asymmetric or multifocal deficits, and selective involvement of motor, sensory, or auto- nomic nerves are clues suggesting an autoimmune, inflammatory cause. The clinical presentation, however, may be indistinguishable from other forms of chronic length-dependent sensorimotor PN. Antibodies against specific glycolipids or glycoproteins, such as anti- GM1 and anti–myelin-associated glycoprotein (MAG), are associated with inflammatory (often demyelinating) peripheral nerve syndromes. In some cases, these antibodies identify motor or sensory neuropathies that are responsive to immunotherapy [1–3] or those with a different prognosis [4,5]. Antineuronal nuclear and cytoplasmic antibodies (such as anti-Hu and CRMP-5) help identify patients who have paraneoplastic neuropathy resulting from remote immunologic effects of malignancy [6,7]. Various other serologic tests, although less specific, can be used to provide clues about the presence of systemic autoimmune disease that can affect the nerves. These include serologic markers for Sjo¨gren’s syndrome (SS), rheu- matoid arthritis, celiac disease, and systemic vasculitides (such as Churg- Strauss syndrome) [8,9]. Because the cause of acquired neuropathies often is obscure, autoanti- body testing can be of great diagnostic value in identifying autoimmune * Corresponding author. -

Transglutaminase in Ocular Health and Pathological Processes
perim Ex en l & ta a l ic O p in l h t C h f Journal of Clinical & Experimental a Tong et al. J Clinic Experiment Ophthalmol 2011, S:2 o l m l a o n l DOI: 10.4172/2155-9570.S2-002 r o g u y o J Ophthalmology ISSN: 2155-9570 ResearchResearch Article Article OpenOpen Access Access Recent Advances: Transglutaminase in Ocular Health and Pathological Processes Louis Tong1,2,3*, Evelyn Png2, Wanwen Lan2 and Andrea Petznick2 1Singapore National Eye Center, Singapore 2Singapore Eye Research Institute, Singapore 3Duke-NUS Graduate Medical School, Singapore Abstract Transglutaminase (TG) is a diverse class of crosslinking enzymes involved in the regulation of cytokine production, endocytosis, cell adhesion, migration, apoptosis and autophagy. It has been implicated in inflammatory diseases, neurodegenerative processes and cancer. The eye is a specialized organ which subserves the important function of vision and has distinctive physiological and anatomical properties that differ from other body tissues. Understanding of the roles of various TGs in the eye therefore require studies specific to cells and tissues of ocular origin. We review the advances in TG research in ocular diseases, including pterygium, glaucoma, cataract and proliferative vitreoretinopathy. TG1 is a molecule important for keratinisation in many cicatrizing diseases of the ocular surface, including keratoconjunctivitis sicca. TG2, with multiple functions, has been shown to be important in inflammation and cell adhesion in various ocular diseases. The results of TG research in each region of the eye are critically assessed and the implications of these studies in the treatment of ocular diseases are discussed. -

Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (Membrane/Cardiolipin/Gangliosides/Ca + +/Phase Transition) J
Proc. Nat. Acad. Sci. USA Vol. 70, No. 5, pp. 1406-1409, May 1973 Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (membrane/cardiolipin/gangliosides/Ca + +/phase transition) J. M. BOGGS AND J. C. HSIA Department of Pharmacology, Faculty of Medicine, University of Toronto, Toronto M5S 1A8 Ontario, Canada Communicated by David E. Green, March 5, 1973 ABSTRACT The acyl chain of spin-labeled fatty acids preferred orientation in cylindrical and spherical micellar intercalates between the lipid hydrocarbon chains in hexag- phases with the long axis parallel to the lipid acyl chains, onal and micellar phases with the carboxyl group anchored at the lipid water interface. The spectra are resulting in spectra characteristic of rapid anisotropic motion characteristic of anisotropic motion and cannot be dis- and (b) there is a fluidity gradient in the hexagonal phase, tinguished from the spectra of these probes in lamellar i.e., the motional freedom of the acyl chains increases toward dispersions. In the hexagonal and micellar phases the the terminal methyl group as has been observed for the molecular motion of the spin label increases as it is moved further away from the carboxyl group, similar to the be- lamellar phase (2, 4, 5). havior in the lamellar phase (Jost et al. (1971) J. Mol. Biol. 59, 77-98). The similarity in packing of the acyl chains in MATERIALS AND METHODS the hexagonal and lamellar phases suggests that localized 5-Doxyl-palmitic acid [1(10,3)] and 8-doxyl-palmitic acid regions of hexagonal phase are compatible with a bilayer [I(7,6)] were prepared according to the method of Hubbell matrix. -

Activated Receptor 4 Ala120thr Variant Alters Platelet Responsiveness to Low‐
Journal of Thrombosis and Haemostasis, 16: 2501–2514 DOI: 10.1111/jth.14318 ORIGINAL ARTICLE The protease-activated receptor 4 Ala120Thr variant alters platelet responsiveness to low-dose thrombin and protease-activated receptor 4 desensitization, and is blocked by non-competitive P2Y12 inhibition M. J. WHITLEY,* D. M. HENKE,† A. GHAZI,† M. NIEMAN,‡ M. STOLLER,§ L. M. SIMON,† E. CHEN,† J. VESCI,* M. HOLINSTAT,¶ S. E. MCKENZIE,* C. A. SHAW,† ** L. C. EDELSTEIN* andP. F. BRAY§ *The Cardeza Foundation for Hematologic Research and the Department of Medicine, Thomas Jefferson University, Jefferson Medical College, Philadelphia, PA; †Department of Human & Molecular Genetics, Baylor College of Medicine, Houston, TX; ‡Department of Pharmacology, Case Western Reserve University, Cleveland, OH; §Program in Molecular Medicine and the Division of Hematology and Hematologic Malignancies, Department of Internal Medicine, University of Utah, Salt Lake City, UT; ¶Department of Pharmacology, University of Michigan, Ann Arbor, MI; and **Department of Statistics, Rice University, Houston, TX, USA To cite this article: Whitley MJ, Henke DM, Ghazi A, Nieman M, Stoller M, Simon LM, Chen E, Vesci J, Holinstat M, McKenzie SE, Shaw CA, Edelstein LC, Bray PF. The protease-activated receptor 4 Ala120Thr variant alters platelet responsiveness to low-dose thrombin and protease- activated receptor 4 desensitization, and is blocked by non-competitive P2Y12 inhibition. J Thromb Haemost 2018; 16: 2501–14. thrombin was assessed without and with antiplatelet antag- Essentials onists. The association of rs773902 alleles with stroke was assessed in the Stroke Genetics Network study. Results: • The rs773902 SNP results in differences in platelet pro- As compared with rs773902 GG donors, platelets from tease-activated receptor (PAR4) function. -
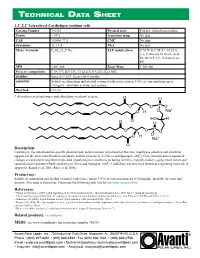
Technical Data Sheet
TECHNICAL DA T A SHEE T 1,1’,2,2’ Tetraoleoyl Cardiolipin (sodium salt) Catalog Number 710335 Physical state Powder; chloroform solution Purity > 99% Transition temp. No data CAS 115404-77-8 CMC No data Synonyms 18:1 CA PKA No data Molec. Formula C81H148O17P2Na2 TLC mobile phase C:M:W & C:M:A*, 65:25:4, v/v; C:Hexane:M:Acetic Acid 50:30:10:5, v/v, if want to see PG MW 1,501.000 Exact Mass 1,501.000 Percent composition C 64.77% H 9.93% O 18.11% P 4.12% Na 3.06% Stability Store in <-20°C freezer for 6 months Solubility Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Web link 710335 * chloroform:methanol:water and chloroform:methanol:acetone Description: Cardiolipin, the mitochondrial-specific phospholipid, helps maintain mitochondrial function, membrane potential and structural support for the inner mitochondrial membrane and the proteins in it (Chicco and Sparagna, 2007). Concentration and composition changes of cardiolipin have been implicated in pathological conditions including ischemia, hypothyroidism, aging, heart failure and cardioskeletal myopathy (Barth syndrome) (Chicco and Sparagna, 2007). Cardiolipin has also been shown as a signaling molecule in apoptosis (Kagan et al, 2006; Ritov et al, 2006). Product use: Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Also used in liposomes. Please use the following web link for liposome preparation. References: • Huang and Frohman (2009). -
Nicotinic Acetylcholine Receptor Signaling in Neuroprotection
Akinori Akaike · Shun Shimohama Yoshimi Misu Editors Nicotinic Acetylcholine Receptor Signaling in Neuroprotection Nicotinic Acetylcholine Receptor Signaling in Neuroprotection Akinori Akaike • Shun Shimohama Yoshimi Misu Editors Nicotinic Acetylcholine Receptor Signaling in Neuroprotection Editors Akinori Akaike Shun Shimohama Department of Pharmacology, Graduate Department of Neurology, School of School of Pharmaceutical Sciences Medicine Kyoto University Sapporo Medical University Kyoto, Japan Sapporo, Hokkaido, Japan Wakayama Medical University Wakayama, Japan Yoshimi Misu Graduate School of Medicine Yokohama City University Yokohama, Kanagawa, Japan ISBN 978-981-10-8487-4 ISBN 978-981-10-8488-1 (eBook) https://doi.org/10.1007/978-981-10-8488-1 Library of Congress Control Number: 2018936753 © The Editor(s) (if applicable) and The Author(s) 2018. This book is an open access publication. Open Access This book is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made. The images or other third party material in this book are included in the book’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. The use of general descriptive names, registered names, trademarks, service marks, etc. -

Diffusion of Lipids and GPI-Anchored Proteins in Actin-Free Plasma Membrane Vesicles Measured by STED-FCS Falk Schneidera, Mathias P
bioRxiv preprint doi: https://doi.org/10.1101/076109; this version posted September 19, 2016. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Diffusion of lipids and GPI-anchored proteins in actin-free plasma membrane vesicles measured by STED-FCS Falk Schneidera, Mathias P. Clausena,b, Dominic Waithec, Thomas Kollera, Gunes Ozhand,e, Christian Eggelinga,c,*, Erdinc Sezgina,* a MRC Human Immunology Unit, Weatherall Institute of Molecular Medicine, University of Oxford, OX39DS, Oxford, United Kingdom b MEMPHYS – Center for Biomembrane Physics, Department of Physics, Chemistry, and Pharmacy, University of Southern Denmark, Campusvej 55, 5230 Odense M, Denmark c Wolfson Imaging Centre Oxford, Weatherall Institute of Molecular Medicine, University of Oxford, OX39DS, Oxford, United Kingdom d Izmir International Biomedicine and Genome Institute (iBG-izmir), Dokuz Eylul University, Inciralti- Balcova, 35340 Izmir, Turkey; e Department of Medical Biology and Genetics, Dokuz Eylul University Medical School, Inciralti-Balcova, 35340 Izmir, Turkey. Correspondence: [email protected]; [email protected] Running title: Diffusion in actin-free plasma membrane vesicles Keywords: plasma membrane biophysics, fluorescence correlation spectroscopy, lipid raft, GPI anchored proteins, STED microscopy, STED-FCS, giant plasma membrane vesicles, Abbreviations: giant plasma membrane vesicles (GPMVs), giant unilamellar vesicles (GUVs), Glycophosphatidylinositol anchored protein (GPI-AP), phospholipid (PL), Stimulated emission depletion (STED), fluorescence correlation spectroscopy (FCS) Character count: 19,026 1 bioRxiv preprint doi: https://doi.org/10.1101/076109; this version posted September 19, 2016. -

Antiphospholipid Antibodies Detected by Line Immunoassay Differentiate
Roggenbuck et al. Arthritis Research & Therapy (2016) 18:111 DOI 10.1186/s13075-016-1018-x RESEARCH ARTICLE Open Access Antiphospholipid antibodies detected by line immunoassay differentiate among patients with antiphospholipid syndrome, with infections and asymptomatic carriers Dirk Roggenbuck1,2*†, Maria Orietta Borghi3,4†, Valentina Somma2, Thomas Büttner5, Peter Schierack2, Katja Hanack6, Claudia Grossi4, Caterina Bodio3, Paolo Macor7, Philipp von Landenberg8, Francesco Boccellato9, Michael Mahler10 and Pier Luigi Meroni3,4 Abstract Background: Antiphospholipid antibodies (aPL) can be detected in asymptomatic carriers and infectious patients. The aim was to investigate whether a novel line immunoassay (LIA) differentiates between antiphospholipid syndrome (APS) and asymptomatic aPL+ carriers or patients with infectious diseases (infectious diseases controls (IDC)). Methods: Sixty-one patients with APS (56 primary, 22/56 with obstetric events only, and 5 secondary), 146 controls including 24 aPL+ asymptomatic carriers and 73 IDC were tested on a novel hydrophobic solid phase coated with cardiolipin (CL), phosphatic acid, phosphatidylcholine, phosphatidylethanolamine, phosphatidylglycerol, phosphatidylinositol, phosphatidylserine, beta2-glycoprotein I (β2GPI), prothrombin, and annexin V. Samples were also tested by anti-CL and anti-β2GPI ELISAs and for lupus anticoagulant activity. Human monoclonal antibodies (humoAbs) against human β2GPI or PL alone were tested on the same LIA substrates in the absence or presence of human serum, purified human β2GPI or after CL-micelle absorption. Results: Comparison of LIA with the aPL-classification assays revealed good agreement for IgG/IgM aß2GPI and aCL. Anti-CL and anti-ß2GPI IgG/IgM reactivity assessed by LIA was significantly higher in patients with APS versus healthy controls and IDCs, as detected by ELISA. -

Antiphospholipid Antibodies Are Directed Against Epitopes of Oxidized Phospholipids
Antiphospholipid antibodies are directed against epitopes of oxidized phospholipids. Recognition of cardiolipin by monoclonal antibodies to epitopes of oxidized low density lipoprotein. S Hörkkö, … , W Palinski, J L Witztum J Clin Invest. 1996;98(3):815-825. https://doi.org/10.1172/JCI118854. Research Article The optimal clinical management of patients with antiphospholipid antibody syndrome (APS) is uncertain because of a lack of an underlying hypothesis to explain why antiphospholipid autoantibodies (aPL) form to such ubiquitous compounds as phospholipids (PL). In this paper, we demonstrate that many, if not most, aPL are actually directed at neoepitopes of oxidized PL, or neoepitopes generated by adduct formation between breakdown products of oxidized PL and associated proteins. Each cardiolipin (CL) molecule contains four unsaturated fatty acids and is highly susceptible to oxidation, particularly upon exposure to air. Yet, standard anticardiolipin antibodies (aCL) immunoassays routinely bind CL to microtiter wells by evaporation of the ethanol solvent overnight at 4 degrees C. Using a variety of techniques, we demonstrated that rapid oxidation occurs when CL is plated and exposed to air. Sera from apo E-deficient mice, which have high autoantibody titers to oxidized low density lipoprotein, showed a striking time-dependent increase in binding to CL that was exposed to air for increasing periods of time. Monoclonal antibodies to oxidized LDL, cloned from the apo E- deficient mice, also bound to oxidized CL. Both sera and affinity-purified aCL-IgG from APS patients bound to CL progressively as it was oxidized. However, the monoclonal antibodies from apo E-deficient mice, or sera or aCL-IgG from APS patients did not bind to a reduced CL analog […] Find the latest version: https://jci.me/118854/pdf Antiphospholipid Antibodies Are Directed against Epitopes of Oxidized Phospholipids Recognition of Cardiolipin by Monoclonal Antibodies to Epitopes of Oxidized Low Density Lipoprotein Sohvi Hörkkö,* Elizabeth Miller,* Eric Dudl,* Peter Reaven,* Linda K. -

Autoantibodies and Anti-Microbial Antibodies
bioRxiv preprint doi: https://doi.org/10.1101/403519; this version posted August 29, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Autoantibodies and anti-microbial antibodies: Homology of the protein sequences of human autoantigens and the microbes with implication of microbial etiology in autoimmune diseases Peilin Zhang, MD., Ph.D. PZM Diagnostics, LLC Charleston, WV 25301 Correspondence: Peilin Zhang, MD., Ph.D. PZM Diagnostics, LLC. 500 Donnally St., Suite 303 Charleston, WV 25301 Email: [email protected] Tel: 304 444 7505 1 bioRxiv preprint doi: https://doi.org/10.1101/403519; this version posted August 29, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Abstract Autoimmune disease is a group of diverse clinical syndromes with defining autoantibodies within the circulation. The pathogenesis of autoantibodies in autoimmune disease is poorly understood. In this study, human autoantigens in all known autoimmune diseases were examined for the amino acid sequences in comparison to the microbial proteins including bacterial and fungal proteins by searching Genbank protein databases. Homologies between the human autoantigens and the microbial proteins were ranked high, medium, and low based on the default search parameters at the NCBI protein databases. Totally 64 human protein autoantigens important for a variety of autoimmune diseases were examined, and 26 autoantigens were ranked high, 19 ranked medium to bacterial proteins (69%) and 27 ranked high and 16 ranked medium to fungal proteins (66%) in their respective amino acid sequence homologies.