Metabolic Alterations Caused by Defective Cardiolipin Remodeling in Inherited Cardiomyopathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Novel Gene Fusions in Glioblastoma Tumor Tissue and Matched Patient Plasma
cancers Article Novel Gene Fusions in Glioblastoma Tumor Tissue and Matched Patient Plasma 1, 1, 1 1 1 Lan Wang y, Anudeep Yekula y, Koushik Muralidharan , Julia L. Small , Zachary S. Rosh , Keiko M. Kang 1,2, Bob S. Carter 1,* and Leonora Balaj 1,* 1 Department of Neurosurgery, Massachusetts General Hospital and Harvard Medical School, Boston, MA 02115, USA; [email protected] (L.W.); [email protected] (A.Y.); [email protected] (K.M.); [email protected] (J.L.S.); [email protected] (Z.S.R.); [email protected] (K.M.K.) 2 School of Medicine, University of California San Diego, San Diego, CA 92092, USA * Correspondence: [email protected] (B.S.C.); [email protected] (L.B.) These authors contributed equally. y Received: 11 March 2020; Accepted: 7 May 2020; Published: 13 May 2020 Abstract: Sequencing studies have provided novel insights into the heterogeneous molecular landscape of glioblastoma (GBM), unveiling a subset of patients with gene fusions. Tissue biopsy is highly invasive, limited by sampling frequency and incompletely representative of intra-tumor heterogeneity. Extracellular vesicle-based liquid biopsy provides a minimally invasive alternative to diagnose and monitor tumor-specific molecular aberrations in patient biofluids. Here, we used targeted RNA sequencing to screen GBM tissue and the matched plasma of patients (n = 9) for RNA fusion transcripts. We identified two novel fusion transcripts in GBM tissue and five novel fusions in the matched plasma of GBM patients. The fusion transcripts FGFR3-TACC3 and VTI1A-TCF7L2 were detected in both tissue and matched plasma. -
Technical Reports
TECHNICAL REPORTS Lipid microarrays identify key mediators of autoimmune brain inflammation Jennifer L Kanter1,2, Sirisha Narayana2, Peggy P Ho2, Ingrid Catz3, Kenneth G Warren3, Raymond A Sobel4,6, Lawrence Steinman2 & William H Robinson5,6 Recent studies suggest that increased T-cell and autoantibody against phospholipids and gangliosides contribute to the pathogenesis reactivity to lipids may be present in the autoimmune in systemic lupus erythematosus and Guillain-Barre´ syndrome, respec- demyelinating disease multiple sclerosis. To perform large-scale tively10. Despite reports of myelin-specific lipid responses in multiple multiplex analysis of antibody responses to lipids in multiple sclerosis, the role of lipid-specific autoimmunity in multiple sclerosis sclerosis, we developed microarrays composed of lipids remains controversial11. Most lipids are presented to T cells bound to 12 http://www.nature.com/naturemedicine present in the myelin sheath, including ganglioside, sulfatide, CD1 molecules and CD1 expression is increased in CNS lesions in cerebroside, sphingomyelin and total brain lipid fractions. Lipid- both multiple sclerosis and experimental autoimmune encephalomye- array analysis showed lipid-specific antibodies against sulfatide, litis (EAE)13–15. These observations led us to hypothesize that myelin sphingomyelin and oxidized lipids in cerebrospinal fluid (CSF) lipids may be target autoantigens in individuals with multiple sclerosis derived from individuals with multiple sclerosis. Sulfatide- and to develop lipid-array technology to investigate this hypothesis. specific antibodies were also detected in SJL/J mice with We developed simple, large-scale lipid microarrays for detection of acute experimental autoimmune encephalomyelitis (EAE). autoantibodies present in biological fluids such as serum and cere- Immunization of mice with sulfatide plus myelin peptide brospinal fluid (CSF). -

Extending the Phenotypic Spectrum of Sengers Syndrome: Congenital Lactic Acidosis with Synthetic Liver Dysfunction
Himmelfarb Health Sciences Library, The George Washington University Health Sciences Research Commons Pathology Faculty Publications Pathology 4-13-2018 Extending the phenotypic spectrum of Sengers syndrome: Congenital lactic acidosis with synthetic liver dysfunction. David B Beck Kristina Cusmano-Ozog George Washington University Nickie Andescavage George Washington University Eyby Leon George Washington University Follow this and additional works at: https://hsrc.himmelfarb.gwu.edu/smhs_path_facpubs Part of the Medical Pathology Commons, Pathology Commons, and the Translational Medical Research Commons APA Citation Beck, D., Cusmano-Ozog, K., Andescavage, N., & Leon, E. (2018). Extending the phenotypic spectrum of Sengers syndrome: Congenital lactic acidosis with synthetic liver dysfunction.. Translational Science of Rare Diseases, 3 (1). http://dx.doi.org/10.3233/ TRD-180020 This Journal Article is brought to you for free and open access by the Pathology at Health Sciences Research Commons. It has been accepted for inclusion in Pathology Faculty Publications by an authorized administrator of Health Sciences Research Commons. For more information, please contact [email protected]. Translational Science of Rare Diseases 3 (2018) 45–48 45 DOI 10.3233/TRD-180020 IOS Press Original Research Extending the phenotypic spectrum of Sengers syndrome: Congenital lactic acidosis with synthetic liver dysfunction David B. Becka, Kristina Cusmano-Ozogb, Nickie Andescavagec and Eyby Leonb,∗ aNational Human Genome Research Institute, National Institute of Health, Bethesda, MD, USA bChildren’s National Health System, Rare Disease Institute, Genetics and Metabolism, Washington, DC, USA cChildren’s National Health System, Pediatrics, Neonatology, Washington, DC, USA Abstract. Sengers syndrome is a rare autosomal recessive mitochondrial disease characterized by lactic acidosis, hypertrophic cardiomyopathy and bilateral cataracts. -

Cardiolipin and Mitochondrial Cristae Organization
Biochimica et Biophysica Acta 1859 (2017) 1156–1163 Contents lists available at ScienceDirect Biochimica et Biophysica Acta journal homepage: www.elsevier.com/locate/bbamem Cardiolipin and mitochondrial cristae organization Nikita Ikon, Robert O. Ryan ⁎ Children's Hospital Oakland Research Institute, 5700 Martin Luther King Jr. Way, Oakland, CA 94609, United States article info abstract Article history: A fundamental question in cell biology, under investigation for over six decades, is the structural organization of Received 23 December 2016 mitochondrial cristae. Long known to harbor electron transport chain proteins, crista membrane integrity is key Received in revised form 3 March 2017 to establishment of the proton gradient that drives oxidative phosphorylation. Visualization of cristae morphol- Accepted 18 March 2017 ogy by electron microscopy/tomography has provided evidence that cristae are tube-like extensions of the mito- Available online 20 March 2017 chondrial inner membrane (IM) that project into the matrix space. Reconciling ultrastructural data with the lipid Keywords: composition of the IM provides support for a continuously curved cylindrical bilayer capped by a dome-shaped Cardiolipin tip. Strain imposed by the degree of curvature is relieved by an asymmetric distribution of phospholipids in Mitochondria monolayer leaflets that comprise cristae membranes. The signature mitochondrial lipid, cardiolipin (~18% of Cristae IM phospholipid mass), and phosphatidylethanolamine (34%) segregate to the negatively curved monolayer leaf- Membrane curvature let facing the crista lumen while the opposing, positively curved, matrix-facing monolayer leaflet contains pre- Non-bilayer lipid dominantly phosphatidylcholine. Associated with cristae are numerous proteins that function in distinctive Electron transport chain ways to establish and/or maintain their lipid repertoire and structural integrity. -

Two Novel Mutations in the AGK Gene: Two Case Reports with Sengers
Techno e lo Kor et al., Gene Technol 2016, 5:1 n g e y G Gene Technology DOI: 10.4172/2329-6682.1000140 ISSN: 2329-6682 Case Report Open Access Two Novel Mutations in the AGK Gene: Two Case Reports with Sengers Syndrome Deniz Kor1*, Berna Seker Yılmaz1, Ozden Ozgur Horoz2, Gulay Ceylaner3, Selcuk Sızmaz4, Fadli Demir2 and Neslihan Onenli Mungan1 1Department of Pediatric Metabolism and Nutrition, Faculty of Medicine, Cukurova University, Adana, Turkey 2Department of Pediatrics, Faculty of Medicine, Cukurova University, Adana, Turkey 3Intergen Genetic Laboratory, Ankara, Turkey 4Department of Ophthalmology, Cukurova University Faculty of Medicine, Adana, Turkey Abstract Mutations in the AGK gene are known to cause Sengers Syndrome, a rare recessive disorder characterized by congenital cataracts, hypertrophic cardiomyopathy, skeletal myopathy, exercise intolerance and lactic acidosis with normal mental development. Since the first report in 1975 by Sengers et al. about 50 individuals have been described as having this syndrome. Here we report two novel mutations in the AGK gene in two patients with neonatal Sengers syndrome. Keywords: AGK gene; Sengers syndrome; Cardiomyopathy; acylcarnitine levels, plasma amino acids and urine organic acids) Myopathy; Cataract were within normal limits except elevated levels of creatine kinases and lactate. Echocardiographic evaluation documented hypertrophic Introduction cardiomyopathy with an ejection fraction of 30%. Electromyography Sengers Syndrome (OMIM 212350), also known as cardiomyopathic and cerebral MRI showed no abnormality. A quadriceps muscle biopsy mitochondrial DNA depletion syndrome-10 (MTDPS10) is a rare revealed fatty infiltrations in the muscle fibers and myopathic changes. autosomal-recessive disorder characterized by congenital cataracts, Based on these observations a clinical diagnosis of Sengers Syndrome hypertrophic cardiomyopathy, skeletal myopathy, exercise intolerance was made. -

Supplemental Information
Supplemental information Dissection of the genomic structure of the miR-183/96/182 gene. Previously, we showed that the miR-183/96/182 cluster is an intergenic miRNA cluster, located in a ~60-kb interval between the genes encoding nuclear respiratory factor-1 (Nrf1) and ubiquitin-conjugating enzyme E2H (Ube2h) on mouse chr6qA3.3 (1). To start to uncover the genomic structure of the miR- 183/96/182 gene, we first studied genomic features around miR-183/96/182 in the UCSC genome browser (http://genome.UCSC.edu/), and identified two CpG islands 3.4-6.5 kb 5’ of pre-miR-183, the most 5’ miRNA of the cluster (Fig. 1A; Fig. S1 and Seq. S1). A cDNA clone, AK044220, located at 3.2-4.6 kb 5’ to pre-miR-183, encompasses the second CpG island (Fig. 1A; Fig. S1). We hypothesized that this cDNA clone was derived from 5’ exon(s) of the primary transcript of the miR-183/96/182 gene, as CpG islands are often associated with promoters (2). Supporting this hypothesis, multiple expressed sequences detected by gene-trap clones, including clone D016D06 (3, 4), were co-localized with the cDNA clone AK044220 (Fig. 1A; Fig. S1). Clone D016D06, deposited by the German GeneTrap Consortium (GGTC) (http://tikus.gsf.de) (3, 4), was derived from insertion of a retroviral construct, rFlpROSAβgeo in 129S2 ES cells (Fig. 1A and C). The rFlpROSAβgeo construct carries a promoterless reporter gene, the β−geo cassette - an in-frame fusion of the β-galactosidase and neomycin resistance (Neor) gene (5), with a splicing acceptor (SA) immediately upstream, and a polyA signal downstream of the β−geo cassette (Fig. -

Serum from Pediatric Dilated Cardiomyopathy Patients Causes Dysregulation of Cardiolipin Biosynthesis and Mitochondrial Function Julie Pires Da Silva, Anastacia M
Serum From Pediatric Dilated Cardiomyopathy Patients Causes Dysregulation of Cardiolipin Biosynthesis and Mitochondrial Function Julie Pires Da Silva, Anastacia M. Garcia, Carissa A. Miyano, Genevieve C. Sparagna, Raleigh Jonscher, Hanan Elajaili, and Carmen C. Sucharov. University of Colorado Anschutz Medical Campus, Aurora, CO Dilated Cardiomyopathy (DCM) Hypothesis - Dilated cardiomyopathy (DCM) is defined as a disorder characterized by Using a novel in vitro model of DCM-related cardiomyocyte remodeling that dilation and impaired contraction of the left ventricle or both ventricles. reproduces the molecular characteristics of pediatric DCM, we hypothesized that the alteration of mitochondrial function in NRVM treated - DCM is the most common form of cardiomyopathy and cause of heart with DCM pediatric sera is associate with changes in cardiolipin content and failure in children older than 1 year of age with an annual incidence of 0.57 mitochondrial β-oxidation pathway. per 100,000 children. - The causes of heart failure (HF) in children differ substantially from those Results found in the adult population and children do not respond well to adult HF therapies. Cardiolipin (CL) - Cardiolipin is a mitochondrial dimeric phospholipid normally located in the inner mitochondrial membrane Figure 5. DCM serum induces significant changes in metabolite levels involved in fatty acid oxidation pathway in NRVMs. A. Heatmap of 41 - CL represent 12-15% of phospholipid mass in heart. In the metabolites differentially expressed in NF and DCM serum-treated NRVMs. n = 4 NF, n= 4 DCM samples, p<0.05. B. Pathway enrichment map analysis heart, 70-80% is (18:2)4CL. of differential metabolites between NF and DCM groups using Figure 3. -

Transglutaminase in Ocular Health and Pathological Processes
perim Ex en l & ta a l ic O p in l h t C h f Journal of Clinical & Experimental a Tong et al. J Clinic Experiment Ophthalmol 2011, S:2 o l m l a o n l DOI: 10.4172/2155-9570.S2-002 r o g u y o J Ophthalmology ISSN: 2155-9570 ResearchResearch Article Article OpenOpen Access Access Recent Advances: Transglutaminase in Ocular Health and Pathological Processes Louis Tong1,2,3*, Evelyn Png2, Wanwen Lan2 and Andrea Petznick2 1Singapore National Eye Center, Singapore 2Singapore Eye Research Institute, Singapore 3Duke-NUS Graduate Medical School, Singapore Abstract Transglutaminase (TG) is a diverse class of crosslinking enzymes involved in the regulation of cytokine production, endocytosis, cell adhesion, migration, apoptosis and autophagy. It has been implicated in inflammatory diseases, neurodegenerative processes and cancer. The eye is a specialized organ which subserves the important function of vision and has distinctive physiological and anatomical properties that differ from other body tissues. Understanding of the roles of various TGs in the eye therefore require studies specific to cells and tissues of ocular origin. We review the advances in TG research in ocular diseases, including pterygium, glaucoma, cataract and proliferative vitreoretinopathy. TG1 is a molecule important for keratinisation in many cicatrizing diseases of the ocular surface, including keratoconjunctivitis sicca. TG2, with multiple functions, has been shown to be important in inflammation and cell adhesion in various ocular diseases. The results of TG research in each region of the eye are critically assessed and the implications of these studies in the treatment of ocular diseases are discussed. -

Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (Membrane/Cardiolipin/Gangliosides/Ca + +/Phase Transition) J
Proc. Nat. Acad. Sci. USA Vol. 70, No. 5, pp. 1406-1409, May 1973 Orientation and Motion of Amphiphilic Spin Labels in Hexagonal Lipid Phases (membrane/cardiolipin/gangliosides/Ca + +/phase transition) J. M. BOGGS AND J. C. HSIA Department of Pharmacology, Faculty of Medicine, University of Toronto, Toronto M5S 1A8 Ontario, Canada Communicated by David E. Green, March 5, 1973 ABSTRACT The acyl chain of spin-labeled fatty acids preferred orientation in cylindrical and spherical micellar intercalates between the lipid hydrocarbon chains in hexag- phases with the long axis parallel to the lipid acyl chains, onal and micellar phases with the carboxyl group anchored at the lipid water interface. The spectra are resulting in spectra characteristic of rapid anisotropic motion characteristic of anisotropic motion and cannot be dis- and (b) there is a fluidity gradient in the hexagonal phase, tinguished from the spectra of these probes in lamellar i.e., the motional freedom of the acyl chains increases toward dispersions. In the hexagonal and micellar phases the the terminal methyl group as has been observed for the molecular motion of the spin label increases as it is moved further away from the carboxyl group, similar to the be- lamellar phase (2, 4, 5). havior in the lamellar phase (Jost et al. (1971) J. Mol. Biol. 59, 77-98). The similarity in packing of the acyl chains in MATERIALS AND METHODS the hexagonal and lamellar phases suggests that localized 5-Doxyl-palmitic acid [1(10,3)] and 8-doxyl-palmitic acid regions of hexagonal phase are compatible with a bilayer [I(7,6)] were prepared according to the method of Hubbell matrix. -

Altered Traffic of Cardiolipin During Apoptosis: Exposure on the Cell Surface As a Trigger for (Antiphospholipid Antibodies)
Hindawi Publishing Corporation Journal of Immunology Research Volume 2015, Article ID 847985, 9 pages http://dx.doi.org/10.1155/2015/847985 Review Article Altered Traffic of Cardiolipin during Apoptosis: Exposure on the Cell Surface as a Trigger for (Antiphospholipid Antibodies) Valeria Manganelli,1 Antonella Capozzi,1 Serena Recalchi,1 Michele Signore,2 Vincenzo Mattei,1,3 Tina Garofalo,1 Roberta Misasi,1 Mauro Degli Esposti,4 and Maurizio Sorice1 1 Department of Experimental Medicine, Sapienza University of Rome, Viale Regina Elena 324, 00161 Rome, Italy 2Department of Hematology, Oncology and Molecular Medicine, National Institute of Health, Viale Regina Elena 299, 00161 Rome, Italy 3Laboratory of Experimental Medicine and Environmental Pathology, Sabina Universitas, Via dell’Elettronica, 02100 Rieti, Italy 4Italian Institute of Technology, Via Morego 30, 16136 Genoa, Italy Correspondence should be addressed to Maurizio Sorice; [email protected] Received 27 July 2015; Accepted 6 September 2015 Academic Editor: Douglas C. Hooper Copyright © 2015 Valeria Manganelli et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Apoptosis has been reported to induce changes in the remodelling of membrane lipids; after death receptor engagement, specific changes of lipid composition occur not only at the plasma membrane, but also in intracellular membranes. This paper focuses on one important aspect of apoptotic changes in cellular lipids, namely, the redistribution of the mitochondria-specific phospholipid, cardiolipin (CL). CL predominantly resides in the inner mitochondrial membrane, even if the rapid remodelling of its acyl chains and the subsequent degradation occur in other membrane organelles. -
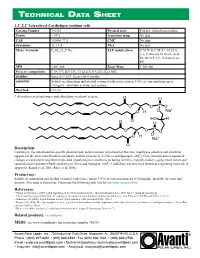
Technical Data Sheet
TECHNICAL DA T A SHEE T 1,1’,2,2’ Tetraoleoyl Cardiolipin (sodium salt) Catalog Number 710335 Physical state Powder; chloroform solution Purity > 99% Transition temp. No data CAS 115404-77-8 CMC No data Synonyms 18:1 CA PKA No data Molec. Formula C81H148O17P2Na2 TLC mobile phase C:M:W & C:M:A*, 65:25:4, v/v; C:Hexane:M:Acetic Acid 50:30:10:5, v/v, if want to see PG MW 1,501.000 Exact Mass 1,501.000 Percent composition C 64.77% H 9.93% O 18.11% P 4.12% Na 3.06% Stability Store in <-20°C freezer for 6 months Solubility Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Web link 710335 * chloroform:methanol:water and chloroform:methanol:acetone Description: Cardiolipin, the mitochondrial-specific phospholipid, helps maintain mitochondrial function, membrane potential and structural support for the inner mitochondrial membrane and the proteins in it (Chicco and Sparagna, 2007). Concentration and composition changes of cardiolipin have been implicated in pathological conditions including ischemia, hypothyroidism, aging, heart failure and cardioskeletal myopathy (Barth syndrome) (Chicco and Sparagna, 2007). Cardiolipin has also been shown as a signaling molecule in apoptosis (Kagan et al, 2006; Ritov et al, 2006). Product use: Soluble in chloroform and alcohol (warmed with water content 3-5%) at concentrations up to 10 mg/mL. Insoluble in water and acetone. Also used in liposomes. Please use the following web link for liposome preparation. References: • Huang and Frohman (2009). -

Identification of Kinase Fusion Oncogenes in Post-Chernobyl Radiation-Induced Thyroid Cancers
Identification of kinase fusion oncogenes in post-Chernobyl radiation-induced thyroid cancers Julio C. Ricarte-Filho, … , Christopher E. Mason, James A. Fagin J Clin Invest. 2013;123(11):4935-4944. https://doi.org/10.1172/JCI69766. Research Article Exposure to ionizing radiation during childhood markedly increases the risk of developing papillary thyroid cancer. We examined tissues from 26 Ukrainian patients with thyroid cancer who were younger than 10 years of age and living in contaminated areas during the time of the Chernobyl nuclear reactor accident. We identified nonoverlapping somatic driver mutations in all 26 cases through candidate gene assays and next-generation RNA sequencing. We found that 22 tumors harbored fusion oncogenes that arose primarily through intrachromosomal rearrangements. Altogether, 23 of the oncogenic drivers identified in this cohort aberrantly activate MAPK signaling, including the 2 somatic rearrangements resulting in fusion of transcription factor ETS variant 6 (ETV6) with neurotrophic tyrosine kinase receptor, type 3 (NTRK3) and fusion of acylglycerol kinase (AGK) with BRAF. Two other tumors harbored distinct fusions leading to overexpression of the nuclear receptor PPARγ. Fusion oncogenes were less prevalent in tumors from a cohort of children with pediatric thyroid cancers that had not been exposed to radiation but were from the same geographical regions. Radiation-induced thyroid cancers provide a paradigm of tumorigenesis driven by fusion oncogenes that activate MAPK signaling or, less frequently, a PPARγ-driven transcriptional program. Find the latest version: https://jci.me/69766/pdf Related Commentary, page 4566 Research article Identification of kinase fusion oncogenes in post-Chernobyl radiation-induced thyroid cancers Julio C.