Molecular Biology of Hodgkin Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Angiogenin Fused to Human CD30 Ligand (Ang-CD30L) Exhibits Specific Cytotoxicity Against CD30-Positive Lymphoma1
[CANCER RESEARCH 61, 8737–8742, December 15, 2001] Human Angiogenin Fused to Human CD30 Ligand (Ang-CD30L) Exhibits Specific Cytotoxicity against CD30-positive Lymphoma1 Michael Huhn, Stephanie Sasse, Mehmet K. Tur, Ba¨rbel Matthey, Timo Schinko¨the, Susanna M. Rybak, Stefan Barth,2 and Andreas Engert Fraunhofer IME, Department of Pharmaceutical Product Development, 52074 Aachen, Germany [M. K. T., M. H., S. B.]; Laboratory of Immunotherapy, Department I of Internal Medicine, University Hospital Cologne, 50931 Cologne, Germany [S. S., B. M., T. S., A. E.]; Developmental Therapeutics Program, Division of Cancer Treatment and Diagnosis, National Cancer Institute-Frederick Cancer Research and Development Center, Frederick, MD 21702 [S. M. R.] ABSTRACT first and then to administer ITs to kill residual H-RS cells. One of the most promising target antigens for immunotherapy of malignant lym- A number of different immunotoxins composed of cell-specific target- phoma such as Hodgkin’s lymphoma or anaplastic large cell lym- ing structures coupled to plant or bacterial toxins have increasingly been phoma is the CD30 receptor. This antigen was originally discovered evaluated for immunotherapy. Because these foreign proteins are highly immunogenic in humans, we have developed a new CD30 ligand-based on cultured H-RS cells using the moab Ki-1 (1). The gene encoding fusion toxin (Ang-CD30L) using the human RNase angiogenin. The com- the CD30 receptor molecule (2) is located on chromosome 1p36. The pletely human fusion gene was inserted into a pET-based expression naturally occurring CD30 ligand has also been identified and cloned plasmid. Transformed Escherichia coli BL21(DE3) were grown under (3). -

4-1BB Signaling Beyond T Cells
Cellular & Molecular Immunology (2011) 8, 281–284 ß 2011 CSI and USTC. All rights reserved 1672-7681/11 $32.00 www.nature.com/cmi MINI REVIEW 4-1BB signaling beyond T cells Dass S Vinay1 and Byoung S Kwon1,2 Originally discovered as a T cell-activating molecule, 4-1BB (CD137) is now also recognized as an activator of non-T cells, thus imparting a new dimension to its potential in vivo effects. 4-1BB expression is seen on a variety of non-T cells including activated dendritic cells (DCs), monocytes, neutrophils, B cells and natural killer (NK) cells, and promotes their individual effector functions. The T cell- and non-T cell-activating ability of 4-1BB may be the basis of its powerful anti-cancer, anti-autoimmune and anti-viral effects. Here we discuss the consequence and importance of 4-1BB signaling in non-T cells. We consider its effects on immune regulation, and the distinct and/or overlapping pathways involved in these responses, as well as possible therapeutic applications. Cellular & Molecular Immunology (2011) 8, 281–284; doi:10.1038/cmi.2010.82; published online 10 January 2011 Keywords: APC; cytokines; natural killer cells; T cells; 4-1BB INTRODUCTION focus on the functions of 4-1BB in non-T cells including DCs, mono- 4-1BB (CD137; TNFRSF9), discovered originally on T cells,1 is a 50- cytes, neutrophils, B cells and NK cells, and discuss how its expression to 55-kDa protein concerned with progressive immunity.2,3 4-1BB might be manipulated to treat various immune diseases. expression is in most cases activation induced. -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Tools for Cell Therapy and Immunoregulation
RnDSy-lu-2945 Tools for Cell Therapy and Immunoregulation Target Cell TIM-4 SLAM/CD150 BTNL8 PD-L2/B7-DC B7-H1/PD-L1 (Human) Unknown PD-1 B7-1/CD80 TIM-1 SLAM/CD150 Receptor TIM Family SLAM Family Butyrophilins B7/CD28 Families T Cell Multiple Co-Signaling Molecules Co-stimulatory Co-inhibitory Ig Superfamily Regulate T Cell Activation Target Cell T Cell Target Cell T Cell B7-1/CD80 B7-H1/PD-L1 T cell activation requires two signals: 1) recognition of the antigenic peptide/ B7-1/CD80 B7-2/CD86 CTLA-4 major histocompatibility complex (MHC) by the T cell receptor (TCR) and 2) CD28 antigen-independent co-stimulation induced by interactions between B7-2/CD86 B7-H1/PD-L1 B7-1/CD80 co-signaling molecules expressed on target cells, such as antigen-presenting PD-L2/B7-DC PD-1 ICOS cells (APCs), and their T cell-expressed receptors. Engagement of the TCR in B7-H2/ICOS L 2Ig B7-H3 (Mouse) the absence of this second co-stimulatory signal typically results in T cell B7-H1/PD-L1 B7/CD28 Families 4Ig B7-H3 (Human) anergy or apoptosis. In addition, T cell activation can be negatively regulated Unknown Receptors by co-inhibitory molecules present on APCs. Therefore, integration of the 2Ig B7-H3 Unknown B7-H4 (Mouse) Receptors signals transduced by co-stimulatory and co-inhibitory molecules following TCR B7-H5 4Ig B7-H3 engagement directs the outcome and magnitude of a T cell response Unknown Ligand (Human) B7-H5 including the enhancement or suppression of T cell proliferation, B7-H7 Unknown Receptor differentiation, and/or cytokine secretion. -

Megakaryopoiesis in Dengue Virus Infected K562 Cell Promotes Viral Replication Which Inhibits 2 Endomitosis and Accumulation of ROS Associated with Differentiation
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.25.172544; this version posted June 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Title: Megakaryopoiesis in Dengue virus infected K562 cell promotes viral replication which inhibits 2 endomitosis and accumulation of ROS associated with differentiation 3 Jaskaran Kaur *1, Yogita Rawat *1, Vikas Sood 2, Deepak Rathore1, Shrikant K. Kumar1, Niraj K. Kumar1 4 and Sankar Bhattacharyya1 5 1 Translational Health Science and Technology Institute, NCR Biotech Science Cluster, PO Box# 4, 6 Faridabad-Gurgaon expressway, Faridabad, Haryana-121001, India 7 2 Department of Biochemistry, School of Chemical and Life Sciences, Jamia Hamdard (Hamdard 8 University) Hamdard Nagar, New Delhi - 110062, India 9 10 *Equal contribution 11 Email for correspondence: [email protected] 12 13 14 Keywords: Dengue virus replication, Megakaryopoiesis, Reactive oxygen species, Endomitosis 15 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.06.25.172544; this version posted June 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 16 Abstract: In the human host blood Monocytes and bone marrow Megakaryocytes are implicated as major 17 sites supporting high replication. The human K562 cell line supports DENV replication and represent 18 Megakaryocyte-Erythrocyte progenitors (MEP), replicating features of in vivo Megakaryopoiesis upon 19 stimulation with Phorbol esters. In this article, we report results that indicate the mutual influence of 20 Megakaryopoiesis and DENV replication on each other, through comparison of PMA-induced 21 differentiation of either mock-infected or DENV-infected K562 cells. -

Autologous T Cells Expressing CD30 Chimeric Antigen Receptors For
Published OnlineFirst August 31, 2016; DOI: 10.1158/1078-0432.CCR-16-1365 Cancer Therapy: Clinical Clinical Cancer Research Autologous T Cells Expressing CD30 Chimeric Antigen Receptors for Relapsed or Refractory Hodgkin Lymphoma: An Open-Label Phase I Trial Chun-Meng Wang1, Zhi-Qiang Wu2,YaoWang3, Ye-Lei Guo3,Han-RenDai3, Xiao-Hui Wang2, Xiang Li2, Ya-Jing Zhang1,Wen-YingZhang1, Mei-Xia Chen1, Yan Zhang1, Kai-Chao Feng1,YangLiu4,Su-XiaLi4, Qing-Ming Yang1, and Wei-Dong Han3 Abstract Purpose: Relapsed or refractory Hodgkin lymphoma is a chal- tolerated, with grade 3 toxicities occurring only in two of 18 lenge for medical oncologists because of poor overall survival. We patients. Of 18 patients, seven achieved partial remission and six aimed to assess the feasibility, safety, and efficacy of CD30- achieved stable disease. An inconsistent response of lymphoma targeting CAR T cells in patients with progressive relapsed or was observed: lymph nodes presented a better response than refractory Hodgkin lymphoma. extranodal lesions and the response of lung lesions seemed to Experimental Design: Patients with relapsed or refractory be relatively poor. Lymphocyte recovery accompanied by an Hodgkin lymphoma received a conditioning chemotherapy fol- increase of circulating CAR T cells (peaking between 3 and 9 days lowed by the CART-30 cell infusion. The level of CAR transgenes after infusion) is a probable indictor of clinical response. Analysis in peripheral blood and biopsied tumor tissues was measured of biopsied tissues by qPCR and immunohistochemistry revealed periodically according to an assigned protocol by quantitative the trafficking of CAR T cells into the targeted sites and reduction PCR (qPCR). -

Uva-DARE (Digital Academic Repository)
UvA-DARE (Digital Academic Repository) Balancing effector lymphocyte formation via CD27-CD70 interactions Arens, R. Publication date 2003 Link to publication Citation for published version (APA): Arens, R. (2003). Balancing effector lymphocyte formation via CD27-CD70 interactions. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:27 Sep 2021 Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens*, Kiki Tesselaar*, Paul A. Baars, Gijs M.W. van Schijndel, Jenny Hendriks, Steven T. Pals, Paul Krimpenfort, Jannie Borst, Marinus H.J. van Oers, and René A.W. van Lier 'These authors contributed equally to this work Immunity 15, 801-812 (2001) Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens123#, Kiki Tesselaar23", Paul A. -
Clinical Trials of CAR-T Cells in China Bingshan Liu1,2, Yongping Song2* and Delong Liu2*
Liu et al. Journal of Hematology & Oncology (2017) 10:166 DOI 10.1186/s13045-017-0535-7 RAPID COMMUNICATION Open Access Clinical trials of CAR-T cells in China Bingshan Liu1,2, Yongping Song2* and Delong Liu2* Abstract Novel immunotherapeutic agents targeting tumor-site microenvironment are revolutionizing cancer therapy. Chimeric antigen receptor (CAR)-engineered T cells are widely studied for cancer immunotherapy. CD19-specific CAR-T cells, tisagenlecleucel, have been recently approved for clinical application. Ongoing clinical trials are testing CAR designs directed at novel targets involved in hematological and solid malignancies. In addition to trials of single-target CAR-T cells, simultaneous and sequential CAR-T cells are being studied for clinical applications. Multi-target CAR-engineered T cells are also entering clinical trials. T cell receptor-engineered CAR-T and universal CAR-T cells represent new frontiers in CAR-T cell development. In this study, we analyzed the characteristics of CAR constructs and registered clinical trials of CAR-T cells in China and provided a quick glimpse of the landscape of CAR-T studies in China. Background “third generation chimeric,” and “fourth generation chimeric”; Novel immunotherapeutic agents targeting CTLA-4, country: China. All relevant trials registered at the Clinical- programmed cell death-1 protein receptor (PD-1), and the Trials.gov prior to July 18, 2017, were included in the analysis. ligand PD-L1 are revolutionizing cancer therapy [1–7]. One trial was excluded (NCT03121625) because the target Cancer immunotherapy by re-igniting T cells through antigen was not disclosed. A search of the PubMed blocking PD-1 and PD-L1 is highly potent in a variety of databasewasalsodonetoincludethosetrialsand malignancies [8–12]. -

Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Dendritic Cell Expression of CD70 in Vivo Potent Cellular Immunity By
Combined TLR/CD40 Stimulation Mediates Potent Cellular Immunity by Regulating Dendritic Cell Expression of CD70 In Vivo This information is current as Phillip J. Sanchez, Jennifer A. McWilliams, Catherine of September 25, 2021. Haluszczak, Hideo Yagita and Ross M. Kedl J Immunol 2007; 178:1564-1572; ; doi: 10.4049/jimmunol.178.3.1564 http://www.jimmunol.org/content/178/3/1564 Downloaded from References This article cites 57 articles, 25 of which you can access for free at: http://www.jimmunol.org/content/178/3/1564.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 25, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Combined TLR/CD40 Stimulation Mediates Potent Cellular Immunity by Regulating Dendritic Cell Expression of CD70 In Vivo1 Phillip J. Sanchez,* Jennifer A. McWilliams,* Catherine Haluszczak,* Hideo Yagita,† and Ross M. Kedl2* We previously showed that immunization with a combination of TLR and CD40 agonists (combined TLR/CD40 agonist immu- nization) resulted in an expansion of Ag-specific CD8 T cells exponentially greater than the expansion observed to immunization with either agonist alone. -
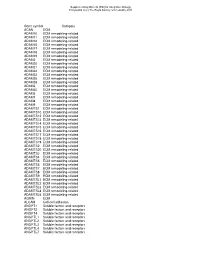
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

GM-CSF Receptor-Beta, Human, Recombinant Recombinant Human Granulocyte/Macrophage Colony Stimulating Factor Receptor Beta
GM-CSF Receptor-beta, human, recombinant Recombinant Human Granulocyte/Macrophage Colony Stimulating Factor Receptor beta Instruction Manual Catalog Number C-60430 Synonyms CSF2RB,Colony Stimulating Factor 2 Receptor, Beta, Low-Affinity (Granulocyte-Macrophage), GM-CSF/IL-3/IL-5 Receptor Common Beta Subunit, CDw131, IL3RB, SMDP5, IL5RB, Interleukin 3 Receptor/Granulocyte-Macrophage Colony Stimulating Factor 3 Receptor, Beta (High Affinity), Colony-Stimulating Factor-2 Receptor, Beta, Low-Affinity, GM-CSF/IL-3/IL-5 Receptor Common Beta-Chain, Cytokine Receptor Common Subunit Beta, CD131 Antigen, CD131 Description GM-CSF Receptor-beta, also known as CSF2RB is a member of the type I cytokine receptor family. CSF2RB is a high affinity receptor for interleukin-3, interleukin-5 as well as granulocyte- macrophage colony-stimulating factor. The CSF2RB unique form of receptor assembly applies also to IL-3 and IL-5 receptors, providing a structural basis for understanding their activation mechanism which is essential for the development of therapeutics. Human recombinant GM-CSF Receptor-beta produced in Sf9 cells is a single, glycosylated polypeptide chain of 435 amino acids (17-443 a.a), having a molecular mass of 49.7 kDa (migrates at 40-57 kDa on SDS-PAGE under reducing conditions). CSF2RB is fused to an 8 amino acid His-tag at the C-terminus and purified using proprietary chromatographic techniques. Quantity 10 µg Molecular Mass 49.7 kDa Source Sf9 insect cells Biological-Activity NA Specific Activity NA Formulation Sterile-filtered, clear protein solution (0.5 mg/ml) containing phosphate-buffered saline (pH 7.4) and 10% glycerol. Reconstitution Please Note: Always centrifuge product briefly before opening vial.