Immunosenescence: a Key Player in Cancer Development Jingyao Lian1,2†, Ying Yue1,2,3†, Weina Yu1,2† and Yi Zhang1,2*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

M.Tech. BT ( R14 Regulations)
M.Tech. BT ( R14 Regulations) CMR COLLEGE OF ENGINEERING & TECHNOLOGY (An Autonomous Institution) ACADEMIC REGULATIONS FOR M. TECH. (REGULAR) DEGREE COURSE Applicable for the students of M. Tech. (Regular) Course from the Academic Year 2014-15 and onwards The M. Tech. degree shall be conferred on candidates who are admitted to the program and who fulfil all the requirements for the award of the degree. 1.0 Eligibility for Admissions Admission to the above program shall be made subject to eligibility, qualification and specialization as prescribed by the State Government from time to time. 2.0 Award of M. Tech. degree 2.1 A student shall be declared eligible for the award of the M. Tech. Degree, if he pursues a course of study in not less than two and not more than four academic years. 2.2 A student, who fails to fulfill all the academic requirements for the award of the degree within four academic years from the year of his admission, shall forfeit his seat in M. Tech. course. 2.3 The student shall register for all 88 credits and secure all the 88 credits. 2.4 The minimum instruction days in each semester are 90. 2.5 The medium of instruction and examination shall be English. 3.0 A. Courses of Study The following specializations are offered at present for the M. Tech. course of study. 1. Bio-Technology 2. Embedded Systems 3. Power Electronics 4. Structural Engineering 5. Computer Science & Engineering 6. Machine Design and any other course as approved by the College/ University/AICTE from time to time. -

Uva-DARE (Digital Academic Repository)
UvA-DARE (Digital Academic Repository) Balancing effector lymphocyte formation via CD27-CD70 interactions Arens, R. Publication date 2003 Link to publication Citation for published version (APA): Arens, R. (2003). Balancing effector lymphocyte formation via CD27-CD70 interactions. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:27 Sep 2021 Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens*, Kiki Tesselaar*, Paul A. Baars, Gijs M.W. van Schijndel, Jenny Hendriks, Steven T. Pals, Paul Krimpenfort, Jannie Borst, Marinus H.J. van Oers, and René A.W. van Lier 'These authors contributed equally to this work Immunity 15, 801-812 (2001) Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens123#, Kiki Tesselaar23", Paul A. -

Defining Natural Antibodies
PERSPECTIVE published: 26 July 2017 doi: 10.3389/fimmu.2017.00872 Defining Natural Antibodies Nichol E. Holodick1*, Nely Rodríguez-Zhurbenko2 and Ana María Hernández2* 1 Department of Biomedical Sciences, Center for Immunobiology, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, MI, United States, 2 Natural Antibodies Group, Tumor Immunology Division, Center of Molecular Immunology, Havana, Cuba The traditional definition of natural antibodies (NAbs) states that these antibodies are present prior to the body encountering cognate antigen, providing a first line of defense against infection thereby, allowing time for a specific antibody response to be mounted. The literature has a seemingly common definition of NAbs; however, as our knowledge of antibodies and B cells is refined, re-evaluation of the common definition of NAbs may be required. Defining NAbs becomes important as the function of NAb production is used to define B cell subsets (1) and as these important molecules are shown to play numerous roles in the immune system (Figure 1). Herein, we aim to briefly summarize our current knowledge of NAbs in the context of initiating a discussion within the field of how such an important and multifaceted group of molecules should be defined. Edited by: Keywords: natural antibody, antibodies, natural antibody repertoire, B-1 cells, B cell subsets, B cells Harry W. Schroeder, University of Alabama at Birmingham, United States NATURAL ANTIBODY (NAb) PRODUCING CELLS Reviewed by: Andre M. Vale, Both murine and human NAbs have been discussed in detail since the late 1960s (2, 3); however, Federal University of Rio cells producing NAbs were not identified until 1983 in the murine system (4, 5). -

Dendritic Cell Expression of CD70 in Vivo Potent Cellular Immunity By
Combined TLR/CD40 Stimulation Mediates Potent Cellular Immunity by Regulating Dendritic Cell Expression of CD70 In Vivo This information is current as Phillip J. Sanchez, Jennifer A. McWilliams, Catherine of September 25, 2021. Haluszczak, Hideo Yagita and Ross M. Kedl J Immunol 2007; 178:1564-1572; ; doi: 10.4049/jimmunol.178.3.1564 http://www.jimmunol.org/content/178/3/1564 Downloaded from References This article cites 57 articles, 25 of which you can access for free at: http://www.jimmunol.org/content/178/3/1564.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 25, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Combined TLR/CD40 Stimulation Mediates Potent Cellular Immunity by Regulating Dendritic Cell Expression of CD70 In Vivo1 Phillip J. Sanchez,* Jennifer A. McWilliams,* Catherine Haluszczak,* Hideo Yagita,† and Ross M. Kedl2* We previously showed that immunization with a combination of TLR and CD40 agonists (combined TLR/CD40 agonist immu- nization) resulted in an expansion of Ag-specific CD8 T cells exponentially greater than the expansion observed to immunization with either agonist alone. -
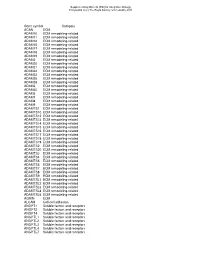
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Instant Notes: Immunology, Second Edition
Immunology Second Edition The INSTANT NOTES series Series Editor: B.D. Hames School of Biochemistry and Molecular Biology, University of Leeds, Leeds, UK Animal Biology 2nd edition Biochemistry 2nd edition Bioinformatics Chemistry for Biologists 2nd edition Developmental Biology Ecology 2nd edition Immunology 2nd edition Genetics 2nd edition Microbiology 2nd edition Molecular Biology 2nd edition Neuroscience Plant Biology Chemistry series Consulting Editor: Howard Stanbury Analytical Chemistry Inorganic Chemistry 2nd edition Medicinal Chemistry Organic Chemistry 2nd edition Physical Chemistry Psychology series Sub-series Editor: Hugh Wagner Dept of Psychology, University of Central Lancashire, Preston, UK Psychology Cognitive Psychology Forthcoming title Physiological Psychology Immunology Second Edition P.M. Lydyard Department of Immunology and Molecular Pathology, Royal Free and University College Medical School, University College London, London, UK A. Whelan Department of Immunology, Trinity College and St James’ Hospital, Dublin, Ireland and M.W. Fanger Department of Microbiology and Immunology, Dartmouth Medical School, Lebanon, New Hampshire, USA © Garland Science/BIOS Scientific Publishers Limited, 2004 First published 2000 This edition published in the Taylor & Francis e-Library, 2005. “To purchase your own copy of this or any of Taylor & Francis or Routledge’s collection of thousands of eBooks please go to www.eBookstore.tandf.co.uk.” Second edition published 2004 All rights reserved. No part of this book may be reproduced or -

Belongs to the TNF Family a New Class of Reverse Signaling
A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink This information is current as J Immunol 2007; 179:4307-4312; ; of September 27, 2021. doi: 10.4049/jimmunol.179.7.4307 http://www.jimmunol.org/content/179/7/4307 References This article cites 85 articles, 38 of which you can access for free at: Downloaded from http://www.jimmunol.org/content/179/7/4307.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision http://www.jimmunol.org/ • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: by guest on September 27, 2021 http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. THE JOURNAL OF IMMUNOLOGY BRIEF REVIEWS A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink1 Recent evidence shows that many molecules of the TNF still remains unclear (7). The N-terminal cytoplasmic domains family serve as counter-receptors, inducing costimulation of most TNF family members are conserved across species but through reverse signals in addition to delivering signals not between family members, suggesting that the intracellular through their respective TNF receptors. -

CD95 Ligand - Death Factor and Costimulatory Molecule?
Cell Death and Differentiation (2003) 10, 1215–1225 & 2003 Nature Publishing Group All rights reserved 1350-9047/03 $25.00 www.nature.com/cdd Review CD95 ligand - death factor and costimulatory molecule? O Janssen*,1, J Qian1, A Linkermann1 and D Kabelitz1 Tissue and Cellular Expression of CD95L 1 Institute for Immunology, Medical Center Schleswig-Holstein, Campus Kiel, Michaelisstrasse 5, D-24105 Kiel, Germany The CD95 ligand (CD95L, Apo-1L, FasL, CD178) is a 281- * Corresponding author: O Janssen. Tel: þ 49-431-5973377; Fax: þ 49-431- amino-acid-containing type II transmembrane protein of the 5973335; E-mail: [email protected] TNF family of death factors (Figure 1).1 Its death-inducing function is best documented in the context of activation- Received 24.4.03; revised 12.6.03; accepted 20.6.03; published online 1 August 2003 induced cell death (AICD) in T cells.2 CD95L is expressed as a Edited by T Ferguson death factor in cytotoxic T lymphocytes (CTL) to kill virally infected or transformed target cells and in natural killer (NK) cells, where it is upregulated by CD16 engagement and 3 Abstract cytokines including IL-2 and IL-12. Similarly, high levels of intracellular CD95L have been detected in monocytic cells The CD95 ligand is involved as a death factor in the with an inducible release upon activation.4 Under physiologi- regulation of activation-induced cell death, establishment cal conditions, CD95L is implicated in the control of erythroid of immune privilege and tumor cell survival. In addition, differentiation,5 angiogenesis in the eye6 and skin home- 7 CD95L may serve as a costimulatory molecule for T-cell ostasis. -

Role of Lymphocytic Choriomeningitis Virus (LCMV) in Understanding Viral Immunology: Past, Present and Future
Viruses 2012, 4, 2650-2669; doi:10.3390/v4112650 OPEN ACCESS viruses ISSN 1999-4915 www.mdpi.com/journal/viruses Review Role of Lymphocytic Choriomeningitis Virus (LCMV) in Understanding Viral Immunology: Past, Present and Future Xin Zhou 1, Srividya Ramachandran 1, Margaret Mann 1 and Daniel L. Popkin 2,* 1 Department of Dermatology, Case Western Reserve University, 10900 Euclid Avenue, Cleveland, OH 44106, USA; E-Mails: [email protected] (X.Z.); [email protected] (S.R.); [email protected] (M.M.) 2 Department of Dermatology, Pathology, Microbiology & Molecular Biology, Case Western Reserve University, 10900 Euclid Avenue, Cleveland, OH 44106, USA * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-216-368-0237; Fax: +1-216-844-8993. Received: 30 September 2012; in revised form: 18 October 2012 / Accepted: 24 October 2012 / Published: 29 October 2012 Abstract: Lymphocytic choriomeningitis virus (LCMV) is a common infection of rodents first identified over eighty years ago in St. Louis, MO, U.S.A. It is best known for its application in immunological studies. The history of LCMV closely correlates with the development of modern immunology. With the use of LCMV as a model pathogen several key concepts have emerged: Major Histocompatibility Complex (MHC) restriction, T cell memory, persistent infections, T cell exhaustion and the key role of immune pathology in disease. Given the phenomenal infrastructure within this field (e.g., defined immunodominant and subdominant epitopes to all T cell receptor specificities as well as the cognate tetramers for enumeration in vivo) the study of LCMV remains an active and productive platform for biological research across the globe to this day. -

Targeting Costimulatory Molecules in Autoimmune Disease
Targeting costimulatory molecules in autoimmune disease Natalie M. Edner1, Gianluca Carlesso2, James S. Rush3 and Lucy S.K. Walker1 1Institute of Immunity & Transplantation, Division of Infection & Immunity, University College London, Royal Free Campus, London, UK NW3 2PF 2Early Oncology Discovery, Early Oncology R&D, AstraZeneca, Gaithersburg, MD, USA 3Autoimmunity, Transplantation and Inflammation Disease Area, Novartis Institutes for Biomedical Research, Basel, Switzerland *Correspondence: Professor Lucy S.K. Walker. Institute of Immunity & Transplantation, Division of Infection & Immunity, University College London, Royal Free Campus, London, UK NW3 2PF. Tel: +44 (0)20 7794 0500 ext 22468. Email: [email protected]. 1 Abstract Therapeutic targeting of immune checkpoints has garnered significant attention in the area of cancer immunotherapy, and efforts have focused in particular on the CD28 family members CTLA-4 and PD-1. In autoimmunity, these same pathways can be targeted to opposite effect, to curb the over- exuberant immune response. The CTLA-4 checkpoint serves as an exemplar, whereby CTLA-4 activity is blocked by antibodies in cancer immunotherapy and augmented by the provision of soluble CTLA-4 in autoimmunity. Here we review the targeting of costimulatory molecules in autoimmune disease, focusing in particular on the CD28 family and TNFR family members. We present the state-of-the-art in costimulatory blockade approaches, including rational combinations of immune inhibitory agents, and discuss the future opportunities and challenges in this field. 2 The risk of autoimmune disease is an inescapable consequence of the manner in which the adaptive immune system operates. To ensure effective immunity against a diverse array of unknown pathogens, antigen recognition systems based on random gene rearrangement and mutagenesis have evolved to anticipate the antigenic universe. -

Immunology 101
Immunology 101 Justin Kline, M.D. Assistant Professor of Medicine Section of Hematology/Oncology Committee on Immunology University of Chicago Medicine Disclosures • I served as a consultant on Advisory Boards for Merck and Seattle Genetics. • I will discuss non-FDA-approved therapies for cancer 2 Outline • Innate and adaptive immune systems – brief intro • How immune responses against cancer are generated • Cancer antigens in the era of cancer exome sequencing • Dendritic cells • T cells • Cancer immune evasion • Cancer immunotherapies – brief intro 3 The immune system • Evolved to provide protection against invasive pathogens • Consists of a variety of cells and proteins whose purpose is to generate immune responses against micro-organisms • The immune system is “educated” to attack foreign invaders, but at the same time, leave healthy, self-tissues unharmed • The immune system can sometimes recognize and kill cancer cells • 2 main branches • Innate immune system – Initial responders • Adaptive immune system – Tailored attack 4 The immune system – a division of labor Innate immune system • Initial recognition of non-self (i.e. infection, cancer) • Comprised of cells (granulocytes, monocytes, dendritic cells and NK cells) and proteins (complement) • Recognizes non-self via receptors that “see” microbial structures (cell wall components, DNA, RNA) • Pattern recognition receptors (PRRs) • Necessary for priming adaptive immune responses 5 The immune system – a division of labor Adaptive immune system • Provides nearly unlimited diversity of receptors to protect the host from infection • B cells and T cells • Have unique receptors generated during development • B cells produce antibodies which help fight infection • T cells patrol for infected or cancerous cells • Recognize “foreign” or abnormal proteins on the cell surface • 100,000,000 unique T cells are present in all of us • Retains “memory” against infections and in some cases, cancer.