Dendritic Cell Expression of CD70 in Vivo Potent Cellular Immunity By
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Uva-DARE (Digital Academic Repository)
UvA-DARE (Digital Academic Repository) Balancing effector lymphocyte formation via CD27-CD70 interactions Arens, R. Publication date 2003 Link to publication Citation for published version (APA): Arens, R. (2003). Balancing effector lymphocyte formation via CD27-CD70 interactions. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:27 Sep 2021 Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens*, Kiki Tesselaar*, Paul A. Baars, Gijs M.W. van Schijndel, Jenny Hendriks, Steven T. Pals, Paul Krimpenfort, Jannie Borst, Marinus H.J. van Oers, and René A.W. van Lier 'These authors contributed equally to this work Immunity 15, 801-812 (2001) Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens123#, Kiki Tesselaar23", Paul A. -
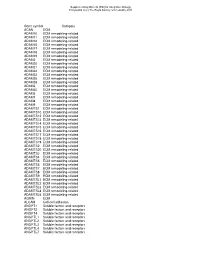
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Belongs to the TNF Family a New Class of Reverse Signaling
A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink This information is current as J Immunol 2007; 179:4307-4312; ; of September 27, 2021. doi: 10.4049/jimmunol.179.7.4307 http://www.jimmunol.org/content/179/7/4307 References This article cites 85 articles, 38 of which you can access for free at: Downloaded from http://www.jimmunol.org/content/179/7/4307.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision http://www.jimmunol.org/ • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: by guest on September 27, 2021 http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. THE JOURNAL OF IMMUNOLOGY BRIEF REVIEWS A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink1 Recent evidence shows that many molecules of the TNF still remains unclear (7). The N-terminal cytoplasmic domains family serve as counter-receptors, inducing costimulation of most TNF family members are conserved across species but through reverse signals in addition to delivering signals not between family members, suggesting that the intracellular through their respective TNF receptors. -

CD95 Ligand - Death Factor and Costimulatory Molecule?
Cell Death and Differentiation (2003) 10, 1215–1225 & 2003 Nature Publishing Group All rights reserved 1350-9047/03 $25.00 www.nature.com/cdd Review CD95 ligand - death factor and costimulatory molecule? O Janssen*,1, J Qian1, A Linkermann1 and D Kabelitz1 Tissue and Cellular Expression of CD95L 1 Institute for Immunology, Medical Center Schleswig-Holstein, Campus Kiel, Michaelisstrasse 5, D-24105 Kiel, Germany The CD95 ligand (CD95L, Apo-1L, FasL, CD178) is a 281- * Corresponding author: O Janssen. Tel: þ 49-431-5973377; Fax: þ 49-431- amino-acid-containing type II transmembrane protein of the 5973335; E-mail: [email protected] TNF family of death factors (Figure 1).1 Its death-inducing function is best documented in the context of activation- Received 24.4.03; revised 12.6.03; accepted 20.6.03; published online 1 August 2003 induced cell death (AICD) in T cells.2 CD95L is expressed as a Edited by T Ferguson death factor in cytotoxic T lymphocytes (CTL) to kill virally infected or transformed target cells and in natural killer (NK) cells, where it is upregulated by CD16 engagement and 3 Abstract cytokines including IL-2 and IL-12. Similarly, high levels of intracellular CD95L have been detected in monocytic cells The CD95 ligand is involved as a death factor in the with an inducible release upon activation.4 Under physiologi- regulation of activation-induced cell death, establishment cal conditions, CD95L is implicated in the control of erythroid of immune privilege and tumor cell survival. In addition, differentiation,5 angiogenesis in the eye6 and skin home- 7 CD95L may serve as a costimulatory molecule for T-cell ostasis. -
Immunosenescence: a Key Player in Cancer Development Jingyao Lian1,2†, Ying Yue1,2,3†, Weina Yu1,2† and Yi Zhang1,2*
Lian et al. J Hematol Oncol (2020) 13:151 https://doi.org/10.1186/s13045-020-00986-z REVIEW Open Access Immunosenescence: a key player in cancer development Jingyao Lian1,2†, Ying Yue1,2,3†, Weina Yu1,2† and Yi Zhang1,2* Abstract Immunosenescence is a process of immune dysfunction that occurs with age and includes remodeling of lymphoid organs, leading to changes in the immune function of the elderly, which is closely related to the development of infections, autoimmune diseases, and malignant tumors. T cell–output decline is an important feature of immunose- nescence as well as the production of senescence-associated secretory phenotype, increased glycolysis, and reactive oxygen species. Senescent T cells exhibit abnormal phenotypes, including downregulation of CD27, CD28, and upreg- ulation of CD57, killer cell lectin-like receptor subfamily G, Tim-3, Tight, and cytotoxic T-lymphocyte-associated protein 4, which are tightly related to malignant tumors. The role of immunosenescence in tumors is sophisticated: the many factors involved include cAMP, glucose competition, and oncogenic stress in the tumor microenvironment, which can induce the senescence of T cells, macrophages, natural killer cells, and dendritic cells. Accordingly, these senescent immune cells could also afect tumor progression. In addition, the efect of immunosenescence on the response to immune checkpoint blocking antibody therapy so far is ambiguous due to the low participation of elderly cancer patients in clinical trials. Furthermore, many other senescence-related interventions could be possible with genetic and pharmacological methods, including mTOR inhibition, interleukin-7 recombination, and NAD + activation. Overall, this review aims to highlight the characteristics of immunosenescence and its impact on malignant tumors and immunotherapy, especially the future directions of tumor treatment through senescence-focused strategies. -

Snapshot: Cytokines III Cristina M
SnapShot: Cytokines III Cristina M. Tato and Daniel J. Cua Schering-Plough Biopharma (Formerly DNAX Research), Palo Alto, CA 94304, USA Cytokine Receptor Source Targets Major Function Disease Association TNFα Murine: Macrophages, Neutrophils, Inflammatory; ↓ = disregulated fever; increased TNFR,p55; TNFR,p75 monocytes, T cells, macrophages, promotes activation susceptibility to bacterial infection; others monocytes, and production of enhanced resistance to LPS-induced septic Human: endothelial cells acute-phase proteins shock TNFR,p60; TNFR,p80 ↑ = exacerbation of arthritis and colitis LTα Murine: T cells, B cells Many cell types Promotes activation ↓ = defective response to bacterial TNFR,p55; TNFR,p75 and cytotoxicity; pathogens; absence of peripheral lymph development of lymph nodes and Peyer’s patches Human: nodes and Peyer’s TNFR,p60; TNFR,p80 patches LTβ LTβR T cells, B cells Myeloid cells, other Peripheral lymph ↓ = increased susceptibility to bacterial cell types node development; infection; absence of lymph nodes and proinflammatory Peyer’s patches ↑ = ectopic lymph node formation LIGHTa LTβR, DcR3, HVEM Activated T cells, B cells, NK cells, Costimulatory; ↓ = defective CD8 T cell costimulation monocytes, DCs DCs, other tissue promotes CTL activity TWEAK Fn14 Monocytes, Tissue progenitors, Proinflammatory; macrophages, epithelial, promotes cell growth endothelial endothelial for tissue repair and remodeling APRIL TACI, BAFF-R, BCMA Macrophages, DCs B cell subsets Promotes T cell- ↓ = impaired class switching to IgA independent -

Molecular Biology of Hodgkin Lymphoma
Leukemia (2021) 35:968–981 https://doi.org/10.1038/s41375-021-01204-6 REVIEW ARTICLE Lymphoma Molecular biology of Hodgkin lymphoma 1 1 Marc A. Weniger ● Ralf Küppers Received: 17 November 2020 / Revised: 1 February 2021 / Accepted: 18 February 2021 / Published online: 8 March 2021 © The Author(s) 2021. This article is published with open access Abstract Classical Hodgkin lymphoma (cHL) is unique among lymphoid malignancies in several key biological features. (i) The Hodgkin and Reed-Sternberg (HRS) tumor cells are rare among an extensive and complex microenvironment. (ii) They derive from B cells, but have largely lost the B-cell typical gene expression program. (iii) Their specific origin appears to be pre-apoptotic germinal center (GC) B cells. (iv) They consistently develop bi- or multinucleated Reed-Sternberg cells from mononuclear Hodgkin cells. (v) They show constitutive activation of numerous signaling pathways. Recent studies have begun to uncover the basis of these specific features of cHL: HRS cells actively orchestrate their complex microenvironment and attract many distinct subsets of immune cells into the affected tissues, to support their survival and proliferation, and to create an immunosuppressive environment. Reed-Sternberg cells are generated by incomplete cytokinesis and refusion of Hodgkin cells. Epstein-Barr virus (EBV) plays a major role in the rescue of crippled GC B cells 1234567890();,: 1234567890();,: from apoptosis and hence is a main player in early steps of lymphomagenesis of EBV+ cHL cases. The analysis of the landscape of genetic lesions in HRS cells so far did not reveal any highly recurrent HRS cell-specific lesions, but major roles of genetic lesions in members of the NF-κB and JAK/STAT pathways and of factors of immune evasion. -

Identification of Novel CD4+ T Cell Subsets in the Target Tissue Of
Identification of Novel CD4+ T Cell Subsets in the Target Tissue of Sjögren's Syndrome and Their Differential Regulation by the Lymphotoxin/LIGHT Signaling Axis This information is current as of October 2, 2021. Scott Haskett, Jian Ding, Wei Zhang, Alice Thai, Patrick Cullen, Shanqin Xu, Britta Petersen, Galina Kuznetsov, Luke Jandreski, Stefan Hamann, Taylor L. Reynolds, Norm Allaire, Timothy S. Zheng and Michael Mingueneau J Immunol 2016; 197:3806-3819; Prepublished online 7 Downloaded from October 2016; doi: 10.4049/jimmunol.1600407 http://www.jimmunol.org/content/197/10/3806 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2016/10/06/jimmunol.160040 Material 7.DCSupplemental References This article cites 46 articles, 8 of which you can access for free at: http://www.jimmunol.org/content/197/10/3806.full#ref-list-1 Why The JI? Submit online. by guest on October 2, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. -

CD153 in Rheumatoid Arthritis: Detection of a Soluble Form in Serum and Synovial Fluid, and Expression by Mast Cells in the Rheumatic Synovium RICARDO F.S
CD153 in Rheumatoid Arthritis: Detection of a Soluble Form in Serum and Synovial Fluid, and Expression by Mast Cells in the Rheumatic Synovium RICARDO F.S. CARVALHO, ANN-KRISTIN ULFGREN, MARIANNE ENGSTRÖM, ERIK af KLINT, and GUNNAR NILSSON ABSTRACT. Objective. A CD30-CD153 mast cell axis has been described in skin inflammations and Hodgkin’s lymphoma. We investigated if a soluble form of CD153 is present in the serum and synovial fluid (SF) of patients with rheumatoid arthritis (RA), and determined whether mast cells express CD153 in the synovium of these patients. Methods. Soluble forms of CD30 and CD153 were quantified in serum and SF of patients with RA by ELISA. Consecutive sections of synovial biopsies from 12 patients were stained against tryptase (mast-cell marker), CD30, and CD153. Results. Elevated concentrations of the soluble form of CD153 were found in serum from 14/15 RA patients. In the SF, 11/20 patients had detectable levels of soluble CD153. CD30 and CD153 were expressed in all biopsies that were studied. Mast cells were present in all the synovial biopsies, and expressed CD153 in one-third of the cases. Conclusion. We observed that CD153 was expressed in the synovium of patients with RA and we were able to correlate the serum levels of soluble CD153 with SF levels in the same patients. Because CD30 can activate mast cells to release chemokines without degranulation, our finding that mast cells express CD153 in RA synovium raises the possibility that a CD30-CD153 axis may contribute to the activation of synovial mast cells in the absence of degranulation. -
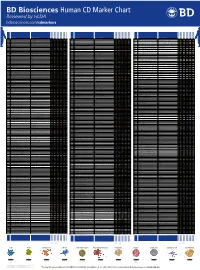
Human CD Marker Chart Reviewed by HLDA1 Bdbiosciences.Com/Cdmarkers
BD Biosciences Human CD Marker Chart Reviewed by HLDA1 bdbiosciences.com/cdmarkers 23-12399-01 CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD1a R4, T6, Leu6, HTA1 b-2-Microglobulin, CD74 + + + – + – – – CD93 C1QR1,C1qRP, MXRA4, C1qR(P), Dj737e23.1, GR11 – – – – – + + – – + – CD220 Insulin receptor (INSR), IR Insulin, IGF-2 + + + + + + + + + Insulin-like growth factor 1 receptor (IGF1R), IGF-1R, type I IGF receptor (IGF-IR), CD1b R1, T6m Leu6 b-2-Microglobulin + + + – + – – – CD94 KLRD1, Kp43 HLA class I, NKG2-A, p39 + – + – – – – – – CD221 Insulin-like growth factor 1 (IGF-I), IGF-II, Insulin JTK13 + + + + + + + + + CD1c M241, R7, T6, Leu6, BDCA1 b-2-Microglobulin + + + – + – – – CD178, FASLG, APO-1, FAS, TNFRSF6, CD95L, APT1LG1, APT1, FAS1, FASTM, CD95 CD178 (Fas ligand) + + + + + – – IGF-II, TGF-b latency-associated peptide (LAP), Proliferin, Prorenin, Plasminogen, ALPS1A, TNFSF6, FASL Cation-independent mannose-6-phosphate receptor (M6P-R, CIM6PR, CIMPR, CI- CD1d R3G1, R3 b-2-Microglobulin, MHC II CD222 Leukemia -

Contribution of CD30/CD153 but Not of CD27/CD70, CD134/OX40L, Or
Contribution of CD30/CD153 but not of CD27/CD70, CD134/OX40L, or CD137/4-1BBL to the optimal induction of protective immunity to Mycobacterium avium Manuela Flo´ rido,* Margarida Borges,* Hideo Yagita,† and Rui Appelberg*,‡,1 *Laboratory of Microbiology and Immunology of Infection, Institute for Molecular and Cell Biology, and ‡ICBAS, Instituto de Cieˆncias Biome´dicas de Abel Salazar, University of Porto, Portugal; and †Department of Immunology, Juntendo University School of Medicine, Tokyo, Japan Abstract: A panel of monoclonal antibodies spe- the role played by the TNFRSF members CD27 (TNFRSF7), cific for CD27 ligand (CD70), CD30 ligand CD30 (TNFRSF8), CD134 (TNFRSF4 or OX40), and CD137 (CD153), CD134 ligand (OX40L), and CD137 li- (TNFRSF9 or 4-1BB) and their ligands CD70 (TNFSF7), gand (4-1BBL) were screened in vivo for their CD153 (TNFSF8), OX40L (TNFSF4), and 4-1BBL (TNFSF9), ability to affect the control of Mycobacterium respectively. avium infection in C57Bl/6 mice. Only the block- CD27/CD70 interactions participate in the early phases of T ing of CD153 led to increased mycobacterial bur- cell responses [2]. Engaging CD27 on T cells activates these dens. We then used CD30-deficient mice and found cells, leading to cytokine secretion and proliferation, and po- an increase in the proliferation of two strains of M. tentiates the activity of other accessory molecules [3]. Mice avium in these mice as compared with control an- deficient in CD27 have impaired responses to influenza virus imals. The increased mycobacterial growth was as- and reduced T cell memory generation [4]. Conversely, chronic sociated with decreased T cell expansion and re- in vivo triggering of CD27 by expression of a CD70 transgene duced interferon-␥ (IFN-␥) responses as a result of led to massive activation and proliferation of T cells with reduced polarization of the antigen-specific, IFN- conversion of naı¨ve cells into cells with an activated/memory ␥-producing T cells.