Supporting Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -
Characterization of a Novel Mouse Model with Genetic Deletion of CD177
Protein Cell 2015, 6(2):117–126 DOI 10.1007/s13238-014-0109-1 Protein & Cell RESEARCH ARTICLE Characterization of a novel mouse model with genetic deletion of CD177 Qing Xie1,2, Julia Klesney-Tait3, Kathy Keck3, Corey Parlet2, Nicholas Borcherding2, Ryan Kolb2, Wei Li2, & Lorraine Tygrett2, Thomas Waldschmidt2, Alicia Olivier2, Songhai Chen4, Guang-Hui Liu5,6, Xiangrui Li1 , Weizhou Zhang2& 1 College of Veterinary Medicine, Nanjing Agricultural University, Nanjing 210095, China 2 Department of Pathology, Holden Comprehensive Cancer Center, Carver College of Medicine/University of Iowa, Iowa, IA 52242, USA 3 Department of Internal Medicine, Carver College of Medicine/University of Iowa, Iowa, IA 52242, USA 4 Department of Pharmacology, Carver College of Medicine/University of Iowa, Iowa, IA 52242, USA Cell 5 National Laboratory of Biomacromolecules, Institute of Biophysics, Chinese Academy of Sciences, Beijing 100101, China & 6 Beijing Institute for Brain Disorders, Beijing 100069, China & Correspondence: [email protected] (X. Li), [email protected] (W. Zhang) Received September 1, 2014 Accepted September 25, 2014 Protein ABSTRACT neutrophil counts in inflammatory skin caused by S. aureus. Mechanistically we found that CD177 deletion in Neutrophils play an essential role in the innate immune mouse neutrophils has no significant impact in CXCL1/ response to infection. Neutrophils migrate from the KC- or fMLP-induced migration, but led to significant cell vasculature into the tissue in response to infection. death. Herein we established a novel genetic mouse Recently, a neutrophil cell surface receptor, CD177, was model to study the role of CD177 and found that CD177 shown to help mediate neutrophil migration across the plays an important role in neutrophils. -

Uva-DARE (Digital Academic Repository)
UvA-DARE (Digital Academic Repository) Balancing effector lymphocyte formation via CD27-CD70 interactions Arens, R. Publication date 2003 Link to publication Citation for published version (APA): Arens, R. (2003). Balancing effector lymphocyte formation via CD27-CD70 interactions. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:27 Sep 2021 Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens*, Kiki Tesselaar*, Paul A. Baars, Gijs M.W. van Schijndel, Jenny Hendriks, Steven T. Pals, Paul Krimpenfort, Jannie Borst, Marinus H.J. van Oers, and René A.W. van Lier 'These authors contributed equally to this work Immunity 15, 801-812 (2001) Chapter 3 Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNy-mediated B cell depletion Ramon Arens123#, Kiki Tesselaar23", Paul A. -

Dendritic Cell Expression of CD70 in Vivo Potent Cellular Immunity By
Combined TLR/CD40 Stimulation Mediates Potent Cellular Immunity by Regulating Dendritic Cell Expression of CD70 In Vivo This information is current as Phillip J. Sanchez, Jennifer A. McWilliams, Catherine of September 25, 2021. Haluszczak, Hideo Yagita and Ross M. Kedl J Immunol 2007; 178:1564-1572; ; doi: 10.4049/jimmunol.178.3.1564 http://www.jimmunol.org/content/178/3/1564 Downloaded from References This article cites 57 articles, 25 of which you can access for free at: http://www.jimmunol.org/content/178/3/1564.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 25, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Combined TLR/CD40 Stimulation Mediates Potent Cellular Immunity by Regulating Dendritic Cell Expression of CD70 In Vivo1 Phillip J. Sanchez,* Jennifer A. McWilliams,* Catherine Haluszczak,* Hideo Yagita,† and Ross M. Kedl2* We previously showed that immunization with a combination of TLR and CD40 agonists (combined TLR/CD40 agonist immu- nization) resulted in an expansion of Ag-specific CD8 T cells exponentially greater than the expansion observed to immunization with either agonist alone. -
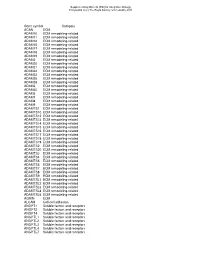
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Belongs to the TNF Family a New Class of Reverse Signaling
A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink This information is current as J Immunol 2007; 179:4307-4312; ; of September 27, 2021. doi: 10.4049/jimmunol.179.7.4307 http://www.jimmunol.org/content/179/7/4307 References This article cites 85 articles, 38 of which you can access for free at: Downloaded from http://www.jimmunol.org/content/179/7/4307.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision http://www.jimmunol.org/ • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: by guest on September 27, 2021 http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. THE JOURNAL OF IMMUNOLOGY BRIEF REVIEWS A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink1 Recent evidence shows that many molecules of the TNF still remains unclear (7). The N-terminal cytoplasmic domains family serve as counter-receptors, inducing costimulation of most TNF family members are conserved across species but through reverse signals in addition to delivering signals not between family members, suggesting that the intracellular through their respective TNF receptors. -

CD95 Ligand - Death Factor and Costimulatory Molecule?
Cell Death and Differentiation (2003) 10, 1215–1225 & 2003 Nature Publishing Group All rights reserved 1350-9047/03 $25.00 www.nature.com/cdd Review CD95 ligand - death factor and costimulatory molecule? O Janssen*,1, J Qian1, A Linkermann1 and D Kabelitz1 Tissue and Cellular Expression of CD95L 1 Institute for Immunology, Medical Center Schleswig-Holstein, Campus Kiel, Michaelisstrasse 5, D-24105 Kiel, Germany The CD95 ligand (CD95L, Apo-1L, FasL, CD178) is a 281- * Corresponding author: O Janssen. Tel: þ 49-431-5973377; Fax: þ 49-431- amino-acid-containing type II transmembrane protein of the 5973335; E-mail: [email protected] TNF family of death factors (Figure 1).1 Its death-inducing function is best documented in the context of activation- Received 24.4.03; revised 12.6.03; accepted 20.6.03; published online 1 August 2003 induced cell death (AICD) in T cells.2 CD95L is expressed as a Edited by T Ferguson death factor in cytotoxic T lymphocytes (CTL) to kill virally infected or transformed target cells and in natural killer (NK) cells, where it is upregulated by CD16 engagement and 3 Abstract cytokines including IL-2 and IL-12. Similarly, high levels of intracellular CD95L have been detected in monocytic cells The CD95 ligand is involved as a death factor in the with an inducible release upon activation.4 Under physiologi- regulation of activation-induced cell death, establishment cal conditions, CD95L is implicated in the control of erythroid of immune privilege and tumor cell survival. In addition, differentiation,5 angiogenesis in the eye6 and skin home- 7 CD95L may serve as a costimulatory molecule for T-cell ostasis. -
Immunosenescence: a Key Player in Cancer Development Jingyao Lian1,2†, Ying Yue1,2,3†, Weina Yu1,2† and Yi Zhang1,2*
Lian et al. J Hematol Oncol (2020) 13:151 https://doi.org/10.1186/s13045-020-00986-z REVIEW Open Access Immunosenescence: a key player in cancer development Jingyao Lian1,2†, Ying Yue1,2,3†, Weina Yu1,2† and Yi Zhang1,2* Abstract Immunosenescence is a process of immune dysfunction that occurs with age and includes remodeling of lymphoid organs, leading to changes in the immune function of the elderly, which is closely related to the development of infections, autoimmune diseases, and malignant tumors. T cell–output decline is an important feature of immunose- nescence as well as the production of senescence-associated secretory phenotype, increased glycolysis, and reactive oxygen species. Senescent T cells exhibit abnormal phenotypes, including downregulation of CD27, CD28, and upreg- ulation of CD57, killer cell lectin-like receptor subfamily G, Tim-3, Tight, and cytotoxic T-lymphocyte-associated protein 4, which are tightly related to malignant tumors. The role of immunosenescence in tumors is sophisticated: the many factors involved include cAMP, glucose competition, and oncogenic stress in the tumor microenvironment, which can induce the senescence of T cells, macrophages, natural killer cells, and dendritic cells. Accordingly, these senescent immune cells could also afect tumor progression. In addition, the efect of immunosenescence on the response to immune checkpoint blocking antibody therapy so far is ambiguous due to the low participation of elderly cancer patients in clinical trials. Furthermore, many other senescence-related interventions could be possible with genetic and pharmacological methods, including mTOR inhibition, interleukin-7 recombination, and NAD + activation. Overall, this review aims to highlight the characteristics of immunosenescence and its impact on malignant tumors and immunotherapy, especially the future directions of tumor treatment through senescence-focused strategies. -

Journal of Translational Medicine Biomed Central
Journal of Translational Medicine BioMed Central Review Open Access CD177: A member of the Ly-6 gene superfamily involved with neutrophil proliferation and polycythemia vera David F Stroncek*, Lorraine Caruccio and Maria Bettinotti Address: From the Department of Transfusion Medicine, Warren G. Magnuson Clinical Center, National Institutes of Health, Bethesda, MD, USA Email: David F Stroncek* - [email protected]; Lorraine Caruccio - [email protected]; Maria Bettinotti - [email protected] * Corresponding author Published: 29 March 2004 Received: 22 December 2003 Accepted: 29 March 2004 Journal of Translational Medicine 2004, 2:8 This article is available from: http://www.translational-medicine.com/content/2/1/8 © 2004 Stroncek et al; licensee BioMed Central Ltd. This is an Open Access article: verbatim copying and redistribution of this article are permitted in all media for any purpose, provided this notice is preserved along with the article's original URL. CD177PRV-1NB1neutrophilspolycythemia veramyelopoiesis Abstract Genes in the Leukocyte Antigen 6 (Ly-6) superfamily encode glycosyl-phosphatidylinositol (GPI) anchored glycoproteins (gp) with conserved domains of 70 to 100 amino acids and 8 to 10 cysteine residues. Murine Ly-6 genes encode important lymphocyte and hematopoietic stem cell antigens. Recently, a new member of the human Ly-6 gene superfamily has been described, CD177. CD177 is polymorphic and has at least two alleles, PRV-1 and NB1. CD177 was first described as PRV-1, a gene that is overexpressed in neutrophils from approximately 95% of patients with polycythemia vera and from about half of patients with essential thrombocythemia. CD177 encodes NB1 gp, a 58–64 kD GPI gp that is expressed by neutrophils and neutrophil precursors. -

Organization, Evolution and Functions of the Human and Mouse Ly6/Upar Family Genes Chelsea L
Loughner et al. Human Genomics (2016) 10:10 DOI 10.1186/s40246-016-0074-2 GENE FAMILY UPDATE Open Access Organization, evolution and functions of the human and mouse Ly6/uPAR family genes Chelsea L. Loughner1, Elspeth A. Bruford2, Monica S. McAndrews3, Emili E. Delp1, Sudha Swamynathan1 and Shivalingappa K. Swamynathan1,4,5,6,7* Abstract Members of the lymphocyte antigen-6 (Ly6)/urokinase-type plasminogen activator receptor (uPAR) superfamily of proteins are cysteine-rich proteins characterized by a distinct disulfide bridge pattern that creates the three-finger Ly6/uPAR (LU) domain. Although the Ly6/uPAR family proteins share a common structure, their expression patterns and functions vary. To date, 35 human and 61 mouse Ly6/uPAR family members have been identified. Based on their subcellular localization, these proteins are further classified as GPI-anchored on the cell membrane, or secreted. The genes encoding Ly6/uPAR family proteins are conserved across different species and are clustered in syntenic regions on human chromosomes 8, 19, 6 and 11, and mouse Chromosomes 15, 7, 17, and 9, respectively. Here, we review the human and mouse Ly6/uPAR family gene and protein structure and genomic organization, expression, functions, and evolution, and introduce new names for novel family members. Keywords: Ly6/uPAR family, LU domain, Three-finger domain, uPAR, Lymphocytes, Neutrophils Introduction an overview of the Ly6/uPAR gene family and their gen- The lymphocyte antigen-6 (Ly6)/urokinase-type plas- omic organization, evolution, as well as functions, and minogen activator receptor (uPAR) superfamily of struc- provide a nomenclature system for the newly identified turally related proteins is characterized by the LU members of this family. -

Suppressive Myeloid Cells Are a Hallmark of Severe COVID-19
medRxiv preprint doi: https://doi.org/10.1101/2020.06.03.20119818; this version posted June 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . 1 Suppressive myeloid cells are a hallmark of 2 severe COVID-19 3 Jonas Schulte-Schrepping1*, Nico Reusch1*, Daniela Paclik2*, Kevin Baßler1*, Stephan 4 Schlickeiser3*, Bowen Zhang4*, Benjamin Krämer5*, Tobias Krammer6*, Sophia Brumhard7*, 5 Lorenzo Bonaguro1*, Elena De Domenico8*, Daniel Wendisch7*, Martin Grasshoff4, Theodore S. 6 Kapellos1, Michael Beckstette4, Tal Pecht1, Adem Saglam8, Oliver Dietrich6, Henrik E. Mei9, Axel 7 R. Schulz9, Claudia Conrad7, Désirée Kunkel10, Ehsan Vafadarnejad6, Cheng-Jian Xu4,11, Arik 8 Horne1, Miriam Herbert1, Anna Drews8, Charlotte Thibeault7, Moritz Pfeiffer7, Stefan 9 Hippenstiel7,12, Andreas Hocke7,12, Holger Müller-Redetzky7, Katrin-Moira Heim7, Felix Machleidt7, 10 Alexander Uhrig7, Laure Bousquillon de Jarcy7, Linda Jürgens7, Miriam Stegemann7, Christoph 11 R. Glösenkamp7, Hans-Dieter Volk2,3,13, Christine Goffinet14,15, Jan Raabe5, Kim Melanie Kaiser5, 12 Michael To Vinh5, Gereon Rieke5, Christian Meisel14, Thomas Ulas8, Matthias Becker8, Robert 13 Geffers16, Martin Witzenrath7,12, Christian Drosten14,19, Norbert Suttorp7,12, Christof von Kalle17, 14 Florian Kurth7,18, Kristian Händler8, Joachim L. Schultze1,8,#,$, Anna C Aschenbrenner20,#, Yang 15 Li4,#, -

Snapshot: Cytokines III Cristina M
SnapShot: Cytokines III Cristina M. Tato and Daniel J. Cua Schering-Plough Biopharma (Formerly DNAX Research), Palo Alto, CA 94304, USA Cytokine Receptor Source Targets Major Function Disease Association TNFα Murine: Macrophages, Neutrophils, Inflammatory; ↓ = disregulated fever; increased TNFR,p55; TNFR,p75 monocytes, T cells, macrophages, promotes activation susceptibility to bacterial infection; others monocytes, and production of enhanced resistance to LPS-induced septic Human: endothelial cells acute-phase proteins shock TNFR,p60; TNFR,p80 ↑ = exacerbation of arthritis and colitis LTα Murine: T cells, B cells Many cell types Promotes activation ↓ = defective response to bacterial TNFR,p55; TNFR,p75 and cytotoxicity; pathogens; absence of peripheral lymph development of lymph nodes and Peyer’s patches Human: nodes and Peyer’s TNFR,p60; TNFR,p80 patches LTβ LTβR T cells, B cells Myeloid cells, other Peripheral lymph ↓ = increased susceptibility to bacterial cell types node development; infection; absence of lymph nodes and proinflammatory Peyer’s patches ↑ = ectopic lymph node formation LIGHTa LTβR, DcR3, HVEM Activated T cells, B cells, NK cells, Costimulatory; ↓ = defective CD8 T cell costimulation monocytes, DCs DCs, other tissue promotes CTL activity TWEAK Fn14 Monocytes, Tissue progenitors, Proinflammatory; macrophages, epithelial, promotes cell growth endothelial endothelial for tissue repair and remodeling APRIL TACI, BAFF-R, BCMA Macrophages, DCs B cell subsets Promotes T cell- ↓ = impaired class switching to IgA independent