Engineering Strategies to Enhance TCR-Based Adoptive T Cell Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Angiogenin Fused to Human CD30 Ligand (Ang-CD30L) Exhibits Specific Cytotoxicity Against CD30-Positive Lymphoma1
[CANCER RESEARCH 61, 8737–8742, December 15, 2001] Human Angiogenin Fused to Human CD30 Ligand (Ang-CD30L) Exhibits Specific Cytotoxicity against CD30-positive Lymphoma1 Michael Huhn, Stephanie Sasse, Mehmet K. Tur, Ba¨rbel Matthey, Timo Schinko¨the, Susanna M. Rybak, Stefan Barth,2 and Andreas Engert Fraunhofer IME, Department of Pharmaceutical Product Development, 52074 Aachen, Germany [M. K. T., M. H., S. B.]; Laboratory of Immunotherapy, Department I of Internal Medicine, University Hospital Cologne, 50931 Cologne, Germany [S. S., B. M., T. S., A. E.]; Developmental Therapeutics Program, Division of Cancer Treatment and Diagnosis, National Cancer Institute-Frederick Cancer Research and Development Center, Frederick, MD 21702 [S. M. R.] ABSTRACT first and then to administer ITs to kill residual H-RS cells. One of the most promising target antigens for immunotherapy of malignant lym- A number of different immunotoxins composed of cell-specific target- phoma such as Hodgkin’s lymphoma or anaplastic large cell lym- ing structures coupled to plant or bacterial toxins have increasingly been phoma is the CD30 receptor. This antigen was originally discovered evaluated for immunotherapy. Because these foreign proteins are highly immunogenic in humans, we have developed a new CD30 ligand-based on cultured H-RS cells using the moab Ki-1 (1). The gene encoding fusion toxin (Ang-CD30L) using the human RNase angiogenin. The com- the CD30 receptor molecule (2) is located on chromosome 1p36. The pletely human fusion gene was inserted into a pET-based expression naturally occurring CD30 ligand has also been identified and cloned plasmid. Transformed Escherichia coli BL21(DE3) were grown under (3). -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Tools for Cell Therapy and Immunoregulation
RnDSy-lu-2945 Tools for Cell Therapy and Immunoregulation Target Cell TIM-4 SLAM/CD150 BTNL8 PD-L2/B7-DC B7-H1/PD-L1 (Human) Unknown PD-1 B7-1/CD80 TIM-1 SLAM/CD150 Receptor TIM Family SLAM Family Butyrophilins B7/CD28 Families T Cell Multiple Co-Signaling Molecules Co-stimulatory Co-inhibitory Ig Superfamily Regulate T Cell Activation Target Cell T Cell Target Cell T Cell B7-1/CD80 B7-H1/PD-L1 T cell activation requires two signals: 1) recognition of the antigenic peptide/ B7-1/CD80 B7-2/CD86 CTLA-4 major histocompatibility complex (MHC) by the T cell receptor (TCR) and 2) CD28 antigen-independent co-stimulation induced by interactions between B7-2/CD86 B7-H1/PD-L1 B7-1/CD80 co-signaling molecules expressed on target cells, such as antigen-presenting PD-L2/B7-DC PD-1 ICOS cells (APCs), and their T cell-expressed receptors. Engagement of the TCR in B7-H2/ICOS L 2Ig B7-H3 (Mouse) the absence of this second co-stimulatory signal typically results in T cell B7-H1/PD-L1 B7/CD28 Families 4Ig B7-H3 (Human) anergy or apoptosis. In addition, T cell activation can be negatively regulated Unknown Receptors by co-inhibitory molecules present on APCs. Therefore, integration of the 2Ig B7-H3 Unknown B7-H4 (Mouse) Receptors signals transduced by co-stimulatory and co-inhibitory molecules following TCR B7-H5 4Ig B7-H3 engagement directs the outcome and magnitude of a T cell response Unknown Ligand (Human) B7-H5 including the enhancement or suppression of T cell proliferation, B7-H7 Unknown Receptor differentiation, and/or cytokine secretion. -

Autologous T Cells Expressing CD30 Chimeric Antigen Receptors For
Published OnlineFirst August 31, 2016; DOI: 10.1158/1078-0432.CCR-16-1365 Cancer Therapy: Clinical Clinical Cancer Research Autologous T Cells Expressing CD30 Chimeric Antigen Receptors for Relapsed or Refractory Hodgkin Lymphoma: An Open-Label Phase I Trial Chun-Meng Wang1, Zhi-Qiang Wu2,YaoWang3, Ye-Lei Guo3,Han-RenDai3, Xiao-Hui Wang2, Xiang Li2, Ya-Jing Zhang1,Wen-YingZhang1, Mei-Xia Chen1, Yan Zhang1, Kai-Chao Feng1,YangLiu4,Su-XiaLi4, Qing-Ming Yang1, and Wei-Dong Han3 Abstract Purpose: Relapsed or refractory Hodgkin lymphoma is a chal- tolerated, with grade 3 toxicities occurring only in two of 18 lenge for medical oncologists because of poor overall survival. We patients. Of 18 patients, seven achieved partial remission and six aimed to assess the feasibility, safety, and efficacy of CD30- achieved stable disease. An inconsistent response of lymphoma targeting CAR T cells in patients with progressive relapsed or was observed: lymph nodes presented a better response than refractory Hodgkin lymphoma. extranodal lesions and the response of lung lesions seemed to Experimental Design: Patients with relapsed or refractory be relatively poor. Lymphocyte recovery accompanied by an Hodgkin lymphoma received a conditioning chemotherapy fol- increase of circulating CAR T cells (peaking between 3 and 9 days lowed by the CART-30 cell infusion. The level of CAR transgenes after infusion) is a probable indictor of clinical response. Analysis in peripheral blood and biopsied tumor tissues was measured of biopsied tissues by qPCR and immunohistochemistry revealed periodically according to an assigned protocol by quantitative the trafficking of CAR T cells into the targeted sites and reduction PCR (qPCR). -
Clinical Trials of CAR-T Cells in China Bingshan Liu1,2, Yongping Song2* and Delong Liu2*
Liu et al. Journal of Hematology & Oncology (2017) 10:166 DOI 10.1186/s13045-017-0535-7 RAPID COMMUNICATION Open Access Clinical trials of CAR-T cells in China Bingshan Liu1,2, Yongping Song2* and Delong Liu2* Abstract Novel immunotherapeutic agents targeting tumor-site microenvironment are revolutionizing cancer therapy. Chimeric antigen receptor (CAR)-engineered T cells are widely studied for cancer immunotherapy. CD19-specific CAR-T cells, tisagenlecleucel, have been recently approved for clinical application. Ongoing clinical trials are testing CAR designs directed at novel targets involved in hematological and solid malignancies. In addition to trials of single-target CAR-T cells, simultaneous and sequential CAR-T cells are being studied for clinical applications. Multi-target CAR-engineered T cells are also entering clinical trials. T cell receptor-engineered CAR-T and universal CAR-T cells represent new frontiers in CAR-T cell development. In this study, we analyzed the characteristics of CAR constructs and registered clinical trials of CAR-T cells in China and provided a quick glimpse of the landscape of CAR-T studies in China. Background “third generation chimeric,” and “fourth generation chimeric”; Novel immunotherapeutic agents targeting CTLA-4, country: China. All relevant trials registered at the Clinical- programmed cell death-1 protein receptor (PD-1), and the Trials.gov prior to July 18, 2017, were included in the analysis. ligand PD-L1 are revolutionizing cancer therapy [1–7]. One trial was excluded (NCT03121625) because the target Cancer immunotherapy by re-igniting T cells through antigen was not disclosed. A search of the PubMed blocking PD-1 and PD-L1 is highly potent in a variety of databasewasalsodonetoincludethosetrialsand malignancies [8–12]. -
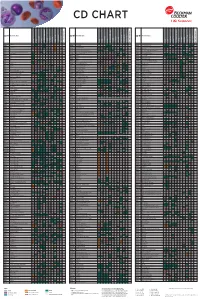
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

CD134/OX40 Code No
D125-3 For Research Use Only. Page 1 of 2 Not for use in diagnostic procedures. MONOCLONAL ANTIBODY CD134/OX40 Code No. Clone Subclass Quantity Concentration D125-3 W4-3 Rat IgG2a 100 L 1 mg/mL BACKGROUND: OX40 (CD134/TNFRSF4/ACT35) is SPECIES CROSS REACTIVITY: a 50 kDa of cell surface glycoprotein. OX40, a member of Species Human Mouse Rat the tumor necrosis factor (TNF) superfamily, is expressed primarily on activated CD4+ T cells. OX40 interacts with Cells MT2, HPB-MLT Not Tested Not Tested OX40 ligand antigen (OX40L, also known as CD252/gp34/CD134L) expressed on activated B cells and Reactivity on FCM + antigen presenting cells results in enhanced T cell proliferation and induction of IL-2 production. REFERENCES: OX40/OX40L interaction provides a costimulatory signal, 1) Kawamata, S., et al., J. Biol. Chem. 273, 5808-5814 (1998) resulting in enhanced T cell proliferation and cytokine 2) Latza, U., et al., Europ. J. Immun. 24, 677-683 (1994) production. Then, cell proliferation and immunoglobulin secretion in activated B cells are enhanced. OX40/OX40L system mediates the adhesion of activated or HTLV-I-transformed T cells to vascular endothelial cells. TRAF2 and TRAF5 binding to OX40 led to NF-B activation, and TRAF3 binding appeared to inhibit NF-B activation SOURCE: This antibody was purified from C.B-17 SCID mice ascites fluid using protein A agarose. This hybridoma (clone W4-3) was established by fusion of mouse myeloma cell SP2/0 with WKA/H rat splenocyte immunized with the human OX40 transfectant. Flow cytometric analysis of CD134 expression on HPB-MLT (left) and PM1 FORMULATION: 100 g IgG in 100 L volume of (right). -

The Thrombopoietin Receptor : Revisiting the Master Regulator of Platelet Production
This is a repository copy of The thrombopoietin receptor : revisiting the master regulator of platelet production. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/175234/ Version: Published Version Article: Hitchcock, Ian S orcid.org/0000-0001-7170-6703, Hafer, Maximillian, Sangkhae, Veena et al. (1 more author) (2021) The thrombopoietin receptor : revisiting the master regulator of platelet production. Platelets. pp. 1-9. ISSN 0953-7104 https://doi.org/10.1080/09537104.2021.1925102 Reuse This article is distributed under the terms of the Creative Commons Attribution (CC BY) licence. This licence allows you to distribute, remix, tweak, and build upon the work, even commercially, as long as you credit the authors for the original work. More information and the full terms of the licence here: https://creativecommons.org/licenses/ Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Platelets ISSN: (Print) (Online) Journal homepage: https://www.tandfonline.com/loi/iplt20 The thrombopoietin receptor: revisiting the master regulator of platelet production Ian S. Hitchcock, Maximillian Hafer, Veena Sangkhae & Julie A. Tucker To cite this article: Ian S. Hitchcock, Maximillian Hafer, Veena Sangkhae & Julie A. Tucker (2021): The thrombopoietin receptor: revisiting the master regulator of platelet production, Platelets, DOI: 10.1080/09537104.2021.1925102 To link to this article: https://doi.org/10.1080/09537104.2021.1925102 © 2021 The Author(s). -

Cytokine Profiling in Myeloproliferative Neoplasms
cells Review Cytokine Profiling in Myeloproliferative Neoplasms: Overview on Phenotype Correlation, Outcome Prediction, and Role of Genetic Variants 1,2, , 1, 1 3 3 Elena Masselli * y , Giulia Pozzi y, Giuliana Gobbi , Stefania Merighi , Stefania Gessi , Marco Vitale 1,2,* and Cecilia Carubbi 1 1 Department of Medicine and Surgery, Anatomy Unit, University of Parma, Via Gramsci 14, 43126 Parma, Italy; [email protected] (G.P.); [email protected] (G.G.); [email protected] (C.C.) 2 University Hospital of Parma, AOU-PR, Via Gramsci 14, 43126 Parma, Italy 3 Department of Morphology, Surgery and Experimental Medicine, University of Ferrara, 44121 Ferrara, Italy; [email protected] (S.M.); [email protected] (S.G.) * Correspondence: [email protected] (E.M.); [email protected] (M.V.); Tel.: +39-052-190-6655 (E.M.); +39-052-103-3032 (M.V.) These authors contributed equally to this work. y Received: 1 September 2020; Accepted: 19 September 2020; Published: 21 September 2020 Abstract: Among hematologic malignancies, the classic Philadelphia-negative chronic myeloproliferative neoplasms (MPNs) are considered a model of inflammation-related cancer development. In this context, the use of immune-modulating agents has recently expanded the MPN therapeutic scenario. Cytokines are key mediators of an auto-amplifying, detrimental cross-talk between the MPN clone and the tumor microenvironment represented by immune, stromal, and endothelial cells. This review focuses on recent advances in cytokine-profiling of MPN patients, analyzing different expression patterns among the three main Philadelphia-negative (Ph-negative) MPNs, as well as correlations with disease molecular profile, phenotype, progression, and outcome. -

CLINICAL RESEARCH PROJECT Protocol #11-H-0134 Drug Name: Eltrombopag (Promacta®) IND Number: 104,877 IND Holder: NHLBI OCD Date: January 2, 2019
CLINICAL RESEARCH PROJECT Protocol #11-H-0134 Drug Name: eltrombopag (Promacta®) IND number: 104,877 IND holder: NHLBI OCD Date: January 2, 2019 Title: A Pilot Study of a Thrombopoietin-receptor Agonist (TPO-R agonist), Eltrombopag, in Moderate Aplastic Anemia Patients Other Identifying Words: Hematopoiesis, autoimmunity, thrombocytopenia, neutropenia, anemia, stem cells, cytokine, Promacta® (eltrombopag) Protocol Principal Investigator: *Cynthia E. Dunbar, M.D., TSCBB, NHLBI (E) Medically and Scientifically Responsible Investigator: *Cynthia E. Dunbar, M.D., TSCBB, NHLBI (E) Associate Investigators: *Georg Aue, M.D., OCD, NHLBI (E) *Neal S. Young, M.D., Chief, HB, NHLBI (E) *André Larochelle, M.D., Ph.D., CMTB, NHLBI (E) David Young, M.D., TSCBB, NHLBI (E) Susan Soto, M.S.N., R.N., Research Nurse, OCD, NHLBI(E) Olga Rios, RN, Research Nurse, OCD, NHLBI (E) Evette Barranta, R.N, Research Nurse, OCD, NHLBI (E) Jennifer Jo Kyte, DNP, Research Nurse, OCD, NHLBI (E) Colin Wu, PhD, Biostatistician, OBR, NHLBI (E) Xin Tian, PhD, Biostatistician, OBR/NHLBI (E) *Janet Valdez, MS, PAC, OCD, NHLBI (E) *Jennifer Lotter, MSHS, PA-C., OCD, NHLBI (E) Qian Sun, Ph.D., DLM, CC (F) Xing Fan, M.D., HB, NHLBI (F) Non-NIH, Non-Enrolling Engaged Investigators: Thomas Winkler, M.D., NHLBI, HB (V)# # Covered under the NIH FWA Independent Medical Monitor: John Tisdale, MD, NHLBI, OSD 402-6497 Bldg. 10, 9N116 * asterisk denotes who can obtain informed consent on this protocol Subjects of Study: Number Sex Age-range 38 Either ≥ 2 years and weight >12 kg Project Involves Ionizing Radiation? No (only when medically indicated) Off-Site Project? No Multi center trial? No DSMB Involvement? Yes 11-H-0134 1 Cynthia E. -

CD30-Redirected Chimeric Antigen Receptor T Cells Target CD30 And
Published OnlineFirst August 7, 2018; DOI: 10.1158/2326-6066.CIR-18-0065 Research Article Cancer Immunology Research CD30-Redirected Chimeric Antigen Receptor T Cells Target CD30þ and CD30– Embryonal Carcinoma via Antigen-Dependent and Fas/FasL Interactions Lee K. Hong1, Yuhui Chen2, Christof C. Smith1, Stephanie A. Montgomery3, Benjamin G. Vincent2, Gianpietro Dotti1,2, and Barbara Savoldo2,4 Abstract Tumor antigen heterogeneity limits success of chimeric (NSG) mouse model of metastatic EC. We observed that CD30. þ antigen receptor (CAR) T-cell therapies. Embryonal carcino- CAR T cells, while targeting CD30 EC tumor cells through mas (EC) and mixed testicular germ cell tumors (TGCT) the CAR (i.e., antigen-dependent targeting), also eliminated – containing EC, which are the most aggressive TGCT subtypes, surrounding CD30 EC cells in an antigen-independent man- are useful for dissecting this issue as ECs express the CD30 ner, via a cell–cell contact-dependent Fas/FasL interaction. In – þ – antigen but also contain CD30 /dim cells. We found that CD30- addition, ectopic Fas (CD95) expression in CD30 Fas EC was redirected CAR T cells (CD30.CAR T cells) exhibit antitumor sufficient to improve CD30.CAR T-cell antitumor activity. activity in vitro against the human EC cell lines Tera-1, Tera-2, Overall, these data suggest that CD30.CAR T cells might be and NCCIT and putative EC stem cells identified by Hoechst useful as an immunotherapy for ECs. Additionally, Fas/FasL dye staining. Cytolytic activity of CD30.CAR T cells was com- interaction between tumor cells and CAR T cells can be plemented by their sustained proliferation and proinflamma- exploited to reduce tumor escape due to heterogeneous antigen tory cytokine production. -

CD30 Induction of Human Immunodeficiency Virus Gene Transcription Is Mediated by TRAF2
Proc. Natl. Acad. Sci. USA Vol. 94, pp. 1390–1395, February 1997 Immunology CD30 induction of human immunodeficiency virus gene transcription is mediated by TRAF2 ERDYNI N. TSITSIKOV,DOWAIN A. WRIGHT, AND RAIF S. GEHA* Division of Immunology, Children’s Hospital, and Department of Pediatrics, Harvard Medical School, Boston, MA 02115 Communicated by Louis Kunkel, Harvard Medical School, Boston, MA, December 17, 1996 (received for review September 4, 1996) ABSTRACT CD30 is a member of the tumor necrosis TRAF3, TRAF4 (CART1), and TRAF5 (17–21). TRAF-1 factor receptor (TNFR) superfamily expressed on activated T and TRAF-2 were found to associate with the intracellular and B lymphocytes and natural killer cells. Ligation of CD30 domain of TNFR2 (16). However, TRAF1 is indirectly asso- was previously shown to induce NF-kB activation and HIV ciated with TNFR2 via dimerization with TRAF2, whereas expression in chronically infected T lymphocytes. In this TRAF2 and TRAF3 bind directly to CD40 (18–20, 22). study, we report that two members of the TNFR-associated TRAF3 is also associated with the lymphotoxin-b receptor and factor (TRAF) family of proteins, TRAF1 and TRAF2, inde- TNFR2 (20). Recently, it was shown that TRAF5 binds to the pendently bind to the intracellular domain of CD30 (CD30IC). lymphotoxin-b receptor (21). TRAF4 was cloned from a breast Transient overexpression of TRAF2, but not TRAF1, induced carcinoma cell line and is the only TRAF that has been NF-kB activation and HIV-1-long terminal repeat-driven localized to the nucleus and may not be associated with a transcription in the T cell line, KT3.