Cytokine Profiling in Myeloproliferative Neoplasms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Therapeutic and Prophylactic Use of Oral, Low-Dose Ifns in Species of Veterinary Interest: Back to the Future
veterinary sciences Review Therapeutic and Prophylactic Use of Oral, Low-Dose IFNs in Species of Veterinary Interest: Back to the Future Sara Frazzini 1 , Federica Riva 2,* and Massimo Amadori 3 1 Gastroenterology and Endoscopy Unit, Fondazione IRCCS Cà Granda, Ospedale Maggiore Policlinico, 20122 Milan, Italy; [email protected] 2 Dipartimento di Medicina Veterinaria, Università degli Studi di Milano, 26900 Lodi, Italy 3 Rete Nazionale di Immunologia Veterinaria, 25125 Brescia, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-0250334519 Abstract: Cytokines are important molecules that orchestrate the immune response. Given their role, cytokines have been explored as drugs in immunotherapy in the fight against different pathological conditions such as bacterial and viral infections, autoimmune diseases, transplantation and cancer. One of the problems related to their administration consists in the definition of the correct dose to avoid severe side effects. In the 70s and 80s different studies demonstrated the efficacy of cytokines in veterinary medicine, but soon the investigations were abandoned in favor of more profitable drugs such as antibiotics. Recently, the World Health Organization has deeply discouraged the use of antibiotics in order to reduce the spread of multi-drug resistant microorganisms. In this respect, the use of cytokines to prevent or ameliorate infectious diseases has been highlighted, and several studies show the potential of their use in therapy and prophylaxis also in the veterinary field. In this review we aim to review the principles of cytokine treatments, mainly IFNs, and to update the experiences encountered in animals. Keywords: veterinary immunotherapy; cytokines; IFN; low dose treatment; oral treatment Citation: Frazzini, S.; Riva, F.; Amadori, M. -
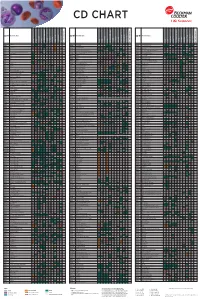
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

IL-11 Induces Encephalitogenic Th17 Cells in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis
IL-11 Induces Encephalitogenic Th17 Cells in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis This information is current as Xin Zhang, Nazanin Kiapour, Sahil Kapoor, Tabish Khan, of September 27, 2021. Madhan Thamilarasan, Yazhong Tao, Stephanie Cohen, Ryan Miller, Raymond A. Sobel and Silva Markovic-Plese J Immunol published online 24 July 2019 http://www.jimmunol.org/content/early/2019/07/23/jimmun ol.1900311 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2019/07/23/jimmunol.190031 Material 1.DCSupplemental http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 27, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Author Choice Freely available online through The Journal of Immunology Author Choice option Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2019 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published July 24, 2019, doi:10.4049/jimmunol.1900311 The Journal of Immunology IL-11 Induces Encephalitogenic Th17 Cells in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis Xin Zhang,* Nazanin Kiapour,* Sahil Kapoor,* Tabish Khan,* Madhan Thamilarasan,* Yazhong Tao,* Stephanie Cohen,† Ryan Miller,‡ Raymond A. -

The Thrombopoietin Receptor : Revisiting the Master Regulator of Platelet Production
This is a repository copy of The thrombopoietin receptor : revisiting the master regulator of platelet production. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/175234/ Version: Published Version Article: Hitchcock, Ian S orcid.org/0000-0001-7170-6703, Hafer, Maximillian, Sangkhae, Veena et al. (1 more author) (2021) The thrombopoietin receptor : revisiting the master regulator of platelet production. Platelets. pp. 1-9. ISSN 0953-7104 https://doi.org/10.1080/09537104.2021.1925102 Reuse This article is distributed under the terms of the Creative Commons Attribution (CC BY) licence. This licence allows you to distribute, remix, tweak, and build upon the work, even commercially, as long as you credit the authors for the original work. More information and the full terms of the licence here: https://creativecommons.org/licenses/ Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Platelets ISSN: (Print) (Online) Journal homepage: https://www.tandfonline.com/loi/iplt20 The thrombopoietin receptor: revisiting the master regulator of platelet production Ian S. Hitchcock, Maximillian Hafer, Veena Sangkhae & Julie A. Tucker To cite this article: Ian S. Hitchcock, Maximillian Hafer, Veena Sangkhae & Julie A. Tucker (2021): The thrombopoietin receptor: revisiting the master regulator of platelet production, Platelets, DOI: 10.1080/09537104.2021.1925102 To link to this article: https://doi.org/10.1080/09537104.2021.1925102 © 2021 The Author(s). -

Engineering Strategies to Enhance TCR-Based Adoptive T Cell Therapy
cells Review Engineering Strategies to Enhance TCR-Based Adoptive T Cell Therapy Jan A. Rath and Caroline Arber * Department of oncology UNIL CHUV, Ludwig Institute for Cancer Research Lausanne, Lausanne University Hospital and University of Lausanne, 1015 Lausanne, Switzerland * Correspondence: [email protected] Received: 18 May 2020; Accepted: 16 June 2020; Published: 18 June 2020 Abstract: T cell receptor (TCR)-based adoptive T cell therapies (ACT) hold great promise for the treatment of cancer, as TCRs can cover a broad range of target antigens. Here we summarize basic, translational and clinical results that provide insight into the challenges and opportunities of TCR-based ACT. We review the characteristics of target antigens and conventional αβ-TCRs, and provide a summary of published clinical trials with TCR-transgenic T cell therapies. We discuss how synthetic biology and innovative engineering strategies are poised to provide solutions for overcoming current limitations, that include functional avidity, MHC restriction, and most importantly, the tumor microenvironment. We also highlight the impact of precision genome editing on the next iteration of TCR-transgenic T cell therapies, and the discovery of novel immune engineering targets. We are convinced that some of these innovations will enable the field to move TCR gene therapy to the next level. Keywords: adoptive T cell therapy; transgenic TCR; engineered T cells; avidity; chimeric receptors; chimeric antigen receptor; cancer immunotherapy; CRISPR; gene editing; tumor microenvironment 1. Introduction Adoptive T cell therapy (ACT) with T cells expressing native or transgenic αβ-T cell receptors (TCRs) is a promising treatment for cancer, as TCRs cover a wide range of potential target antigens [1]. -

CLINICAL RESEARCH PROJECT Protocol #11-H-0134 Drug Name: Eltrombopag (Promacta®) IND Number: 104,877 IND Holder: NHLBI OCD Date: January 2, 2019
CLINICAL RESEARCH PROJECT Protocol #11-H-0134 Drug Name: eltrombopag (Promacta®) IND number: 104,877 IND holder: NHLBI OCD Date: January 2, 2019 Title: A Pilot Study of a Thrombopoietin-receptor Agonist (TPO-R agonist), Eltrombopag, in Moderate Aplastic Anemia Patients Other Identifying Words: Hematopoiesis, autoimmunity, thrombocytopenia, neutropenia, anemia, stem cells, cytokine, Promacta® (eltrombopag) Protocol Principal Investigator: *Cynthia E. Dunbar, M.D., TSCBB, NHLBI (E) Medically and Scientifically Responsible Investigator: *Cynthia E. Dunbar, M.D., TSCBB, NHLBI (E) Associate Investigators: *Georg Aue, M.D., OCD, NHLBI (E) *Neal S. Young, M.D., Chief, HB, NHLBI (E) *André Larochelle, M.D., Ph.D., CMTB, NHLBI (E) David Young, M.D., TSCBB, NHLBI (E) Susan Soto, M.S.N., R.N., Research Nurse, OCD, NHLBI(E) Olga Rios, RN, Research Nurse, OCD, NHLBI (E) Evette Barranta, R.N, Research Nurse, OCD, NHLBI (E) Jennifer Jo Kyte, DNP, Research Nurse, OCD, NHLBI (E) Colin Wu, PhD, Biostatistician, OBR, NHLBI (E) Xin Tian, PhD, Biostatistician, OBR/NHLBI (E) *Janet Valdez, MS, PAC, OCD, NHLBI (E) *Jennifer Lotter, MSHS, PA-C., OCD, NHLBI (E) Qian Sun, Ph.D., DLM, CC (F) Xing Fan, M.D., HB, NHLBI (F) Non-NIH, Non-Enrolling Engaged Investigators: Thomas Winkler, M.D., NHLBI, HB (V)# # Covered under the NIH FWA Independent Medical Monitor: John Tisdale, MD, NHLBI, OSD 402-6497 Bldg. 10, 9N116 * asterisk denotes who can obtain informed consent on this protocol Subjects of Study: Number Sex Age-range 38 Either ≥ 2 years and weight >12 kg Project Involves Ionizing Radiation? No (only when medically indicated) Off-Site Project? No Multi center trial? No DSMB Involvement? Yes 11-H-0134 1 Cynthia E. -

Evolutionary Divergence and Functions of the Human Interleukin (IL) Gene Family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W
UPDATE ON GENE COMPLETIONS AND ANNOTATIONS Evolutionary divergence and functions of the human interleukin (IL) gene family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W. Nebert3* and Vasilis Vasiliou1 1Molecular Toxicology and Environmental Health Sciences Program, Department of Pharmaceutical Sciences, University of Colorado Denver, Aurora, CO 80045, USA 2Department of Clinical Pharmacy, University of Colorado Denver, Aurora, CO 80045, USA 3Department of Environmental Health and Center for Environmental Genetics (CEG), University of Cincinnati Medical Center, Cincinnati, OH 45267–0056, USA *Correspondence to: Tel: þ1 513 821 4664; Fax: þ1 513 558 0925; E-mail: [email protected]; [email protected] Date received (in revised form): 22nd September 2010 Abstract Cytokines play a very important role in nearly all aspects of inflammation and immunity. The term ‘interleukin’ (IL) has been used to describe a group of cytokines with complex immunomodulatory functions — including cell proliferation, maturation, migration and adhesion. These cytokines also play an important role in immune cell differentiation and activation. Determining the exact function of a particular cytokine is complicated by the influence of the producing cell type, the responding cell type and the phase of the immune response. ILs can also have pro- and anti-inflammatory effects, further complicating their characterisation. These molecules are under constant pressure to evolve due to continual competition between the host’s immune system and infecting organisms; as such, ILs have undergone significant evolution. This has resulted in little amino acid conservation between orthologous proteins, which further complicates the gene family organisation. Within the literature there are a number of overlapping nomenclature and classification systems derived from biological function, receptor-binding properties and originating cell type. -

Cellular Vaccines Modified with Hyper IL6 Or Hyper IL11 Combined with Docetaxel in an Orthotopic Prostate Cancer Model
ANTICANCER RESEARCH 35: 3275-3288 (2015) Cellular Vaccines Modified with Hyper IL6 or Hyper IL11 Combined with Docetaxel in an Orthotopic Prostate Cancer Model JACEK MACKIEWICZ1,2.3, URSZULA KAZIMIERCZAK1, MAREK KOTLARSKI1, EWELINA DONDAJEWSKA1, ANNA KOZŁOWSKA1, ELIZA KWIATKOWSKA1,2, ANITA NOWICKA-KOTLARSKA1, HANNA DAMS-KOZŁOWSKA1,2, PIOTR JAN WYSOCKI1 and ANDRZEJ MACKIEWICZ1,2,4 1Medical Biotechnology, University of Medical Sciences, Poznan, Poland; 2Department of Diagnostics and Cancer Immunology, Greater Poland Cancer Centre, Poznan, Poland; 3Department of Medical and Experimental Oncology, Clinical Hospital of Poznan University of Medical Sciences, Poznan, Poland; 4BioContract Sp z o.o., Poznan, Poland Abstract. Background: Whole-cell-based vaccines modified present them in the context of major histocompatibility with Hyper-IL-6 (H6) and Hyper-IL-11 (H11) have complex (MHC) class I and II molecules into T-cells (3). demonstrated high activity in murine melanoma and renal Modification of vaccine cells with genes encoding cancer models. Materials and Methods: H6 and H11 cDNA immunostimulatory molecules, including cytokines, increases was transduced into TRAMP cells (TRAMP-H6 and TRAMP- their immunogenicity. H11). An orthotopic TRAMP model was employed. The Interleukin (IL) 6 and IL11 act on cells through IL6 efficacy of TRAMP-H6 and TRAMP-H11 in combination with receptor (IL6R) and IL11R complex, respectively. These docetaxel was evaluated. Immune cells infiltrating tumors receptors have similar structures. They consist of two were assessed. Results: Immunization with TRAMP-H6 and membrane-bound subunits, α, specific for IL6 or IL11, and β TRAMP-H11 vaccines extended OS of mice. Addition of (GP130) common for both. The β subunit is expressed on docetaxel to TRAMP-H6 and TRAMP-H11 vaccines further every human or animal cell (4), in contrast to α subunits, extended OS of the animals. -

Development and Validation of a Protein-Based Risk Score for Cardiovascular Outcomes Among Patients with Stable Coronary Heart Disease
Supplementary Online Content Ganz P, Heidecker B, Hveem K, et al. Development and validation of a protein-based risk score for cardiovascular outcomes among patients with stable coronary heart disease. JAMA. doi: 10.1001/jama.2016.5951 eTable 1. List of 1130 Proteins Measured by Somalogic’s Modified Aptamer-Based Proteomic Assay eTable 2. Coefficients for Weibull Recalibration Model Applied to 9-Protein Model eFigure 1. Median Protein Levels in Derivation and Validation Cohort eTable 3. Coefficients for the Recalibration Model Applied to Refit Framingham eFigure 2. Calibration Plots for the Refit Framingham Model eTable 4. List of 200 Proteins Associated With the Risk of MI, Stroke, Heart Failure, and Death eFigure 3. Hazard Ratios of Lasso Selected Proteins for Primary End Point of MI, Stroke, Heart Failure, and Death eFigure 4. 9-Protein Prognostic Model Hazard Ratios Adjusted for Framingham Variables eFigure 5. 9-Protein Risk Scores by Event Type This supplementary material has been provided by the authors to give readers additional information about their work. Downloaded From: https://jamanetwork.com/ on 10/02/2021 Supplemental Material Table of Contents 1 Study Design and Data Processing ......................................................................................................... 3 2 Table of 1130 Proteins Measured .......................................................................................................... 4 3 Variable Selection and Statistical Modeling ........................................................................................ -
Techniques for Immune Function Analysis Application Handbook 1St Edition
Techniques for Immune Function Analysis Application Handbook 1st Edition BD Biosciences For additional information please access the Immune Function Homepage at www.bdbiosciences.com/immune_function For Research Use Only. Not for use in diagnostic or therapeutic procedures. Purchase does not include or carry any right to resell or transfer this product either as a stand-alone product or as a component of another product. Any use of this product other than the permitted use without the express written authorization of Becton Dickinson and Company is strictly prohibited. All applications are either tested in-house or reported in the literature. See Technical Data Sheets for details. BD, BD Logo and all other trademarks are the property of Becton, Dickinson and Company. ©2003 BD Table of Contents Preface . 4 Chapter 1: Immunofluorescent Staining of Cell Surface Molecules for Flow Cytometric Analysis . 9 Chapter 2: BD™ Cytometric Bead Array (CBA) Multiplexing Assays . 35 Chapter 3: BD™ DimerX MHC:Ig Proteins for the Analysis of Antigen-specific T Cells. 51 Chapter 4: Immunofluorescent Staining of Intracellular Molecules for Flow Cytometric Analysis . 61 Chapter 5: BD FastImmune™ Cytokine Flow Cytometry. 85 Chapter 6: BD™ ELISPOT Assays for Cells That Secrete Biological Response Modifiers . 109 Chapter 7: ELISA for Specifically Measuring the Levels of Cytokines, Chemokines, Inflammatory Mediators and their Receptors . 125 Chapter 8: BD OptEIA™ ELISA Sets and Kits for Quantitation of Analytes in Serum, Plasma, and Cell Culture Supernatants. 143 Chapter 9: BrdU Staining and Multiparameter Flow Cytometric Analysis of the Cell Cycle . 155 Chapter 10: Cell-based Assays for Biological Response Modifiers . 177 Chapter 11: BD RiboQuant™ Multi-Probe RNase Protection Assay System . -

Tumor Microenvironment State of the Science Advances in Experimental Medicine and Biology
Advances in Experimental Medicine and Biology 1263 Alexander Birbrair Editor Tumor Microenvironment State of the Science Advances in Experimental Medicine and Biology Volume 1263 Series Editors Wim E. Crusio, Institut de Neurosciences Cognitives et Intégratives d’Aquitaine, CNRS and University of Bordeaux UMR 5287, Pessac Cedex, France John D. Lambris, University of Pennsylvania, Philadelphia, PA, USA Heinfried H. Radeke, Institute of Pharmacology & Toxicology, Clinic of the Goethe University Frankfurt Main, Frankfurt am Main, Germany Nima Rezaei, Research Center for Immunodeficiencies, Children's Medical Center, Tehran University of Medical Sciences, Tehran, Iran Advances in Experimental Medicine and Biology provides a platform for scientific contributions in the main disciplines of the biomedicine and the life sciences. This book series publishes thematic volumes on contemporary research in the areas of microbiology, immunology, neurosciences, biochemistry, biomedical engineering, genetics, physiology, and cancer research. Covering emerging topics and techniques in basic and clinical science, it brings together clinicians and researchers from various fields. Advances in Experimental Medicine and Biology has been publishing exceptional works in the field for over 40 years, and is indexed in SCOPUS, Medline (PubMed), Journal Citation Reports/Science Edition, Science Citation Index Expanded (SciSearch, Web of Science), EMBASE, BIOSIS, Reaxys, EMBiology, the Chemical Abstracts Service (CAS), and Pathway Studio. 2018 Impact Factor: 2.126.