The Prevalence of Nelson Bay Virus in Humans and Bats and Its Significance Within the Rf Amework of Conservation Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Diversity of the Chaerephon Leucogaster/Pumilus Complex From
Genetic diversity of the Chaerephon leucogaster/pumilus complex from mainland Africa and the western Indian Ocean islands Theshnie Naidoo 202513500 Submitted in fulfillment of the academic Requirements for the degree of Doctor of Philosophy in the School of Life Sciences, Westville Campus, University of KwaZulu – Natal, Durban. NOVEMBER 2013 Supervisory Committee Prof. JM. Lamb Dr. MC. Schoeman Dr. PJ. Taylor Dr. SM. Goodman i ABSTRACT Chaerephon (Dobson, 1874), an Old World genus belonging to the family Molossidae, is part of the suborder Vespertilioniformes. Members of this genus are distributed across mainland Africa (sample sites; Tanzania, Yemen, Kenya, Botswana, South Africa and Swaziland), its offshore islands (Zanzibar, Pemba and Mozambique Island), Madagascar and the surrounding western Indian Ocean islands (Anjouan, Mayotte, Moheli, Grande Comore, Aldabra and La Reunion). A multifaceted approach was used to elucidate the phylogenetic and population genetic relationships at varying levels amongst these different taxa. Working at the subspecific level, I analysed the phylogenetics and phylogeography of Chaerephon leucogaster from Madagascar, based on mitochondrial cytochrome b and control region sequences. Cytochrome b genetic distances among C. leucogaster samples were low (maximum 0.35 %). Genetic distances between C. leucogaster and C. atsinanana ranged from 1.77 % to 2.62 %. Together, phylogenetic and distance analyses supported the classification of C. leucogaster as a separate species. D-loop data for C. leucogaster samples revealed significant but shallow phylogeographic structuring into three latitudinal groups (13º S, 15 - 17º S, 22 - 23º S) showing exclusive haplotypes which correlated with regions of suitable habitat defined by ecological niche modelling. Population genetic analysis of D-loop sequences indicated that populations from Madagascar have been expanding since 5 842 - 11 143 years BP. -

African Bat Conservation News
Volume 35 African Bat Conservation News August 2014 ISSN 1812-1268 © ECJ Seamark, 2009 (AfricanBats) Above: A male Cape Serotine Bat (Neoromicia capensis) caught in the Chitabi area, Okavango Delta, Botswana. Inside this issue: Research and Conservation Activities Presence of paramyxo and coronaviruses in Limpopo caves, South Africa 2 Observations, Discussions and Updates Recent changes in African Bat Taxonomy (2013-2014). Part II 3 Voucher specimen details for Bakwo Fils et al. (2014) 4 African Chiroptera Report 2014 4 Scientific contributions Documented record of Triaenops menamena (Family Hipposideridae) in the Central Highlands of 6 Madagascar Download and subscribe to African Bat Conservation News published by AfricanBats at: www.africanbats.org The views and opinions expressed in articles are no necessarily those of the editor or publisher. Articles and news items appearing in African Bat Conservation News may be reprinted, provided the author’s and newsletter refer- ence are given. African Bat Conservation News August 2014 vol. 35 2 ISSN 1812-1268 Inside this issue Continued: Recent Literature Conferences 7 Published Books / Reports 7 Papers 7 Notice Board Conferences 13 Call for Contributions 13 Research and Conservation Activities Presence of paramyxo- and coronaviruses in Limpopo caves, South Africa By Carmen Fensham Department of Microbiology and Plant Pathology, Faculty of Natural and Agricultural Sciences, University of Pretoria, 0001, Republic of South Africa. Correspondence: Prof. Wanda Markotter: [email protected] Carmen Fensham is a honours excrement are excised and used to isolate any viral RNA that student in the research group of may be present. The identity of the RNA is then determined Prof. -

Synanthropy of Wild Mammals As a Determinant of Emerging Infectious Diseases in the Asian–Australasian Region
EcoHealth 9, 24–35, 2012 DOI: 10.1007/s10393-012-0763-9 Ó 2012 International Association for Ecology and Health Original Contribution Synanthropy of Wild Mammals as a Determinant of Emerging Infectious Diseases in the Asian–Australasian Region Ro McFarlane,1 Adrian Sleigh,1 and Tony McMichael1 National Centre for Epidemiology and Population Health, ANU College of Medicine, Biology and Environment, Australian National University, Canberra, Australia; [email protected]; [email protected] Abstract: Humans create ecologically simplified landscapes that favour some wildlife species, but not others. Here, we explore the possibility that those species that tolerate or do well in human-modified environments, or ‘synanthropic’ species, are predominantly the hosts of zoonotic emerging and re-emerging infectious diseases (EIDs). We do this using global wildlife conservation data and wildlife host information extracted from systematically reviewed emerging infectious disease literature. The evidence for this relationship is examined with special emphasis on the Australasian, South East Asian and East Asian regions. We find that synanthropic wildlife hosts are approximately 15 times more likely than other wildlife in this region to be the source of emerging infectious diseases, and this association is essentially independent of the taxonomy of the species. A significant positive association with EIDs is also evident for those wildlife species of low conservation risk. Since the increase and spread of native and introduced species able to adapt to human-induced landscape change is at the expense of those species most vulnerable to habitat loss, our findings suggest a mechanism linking land conversion, global decline in biodiversity and a rise in EIDs of wildlife origin. -

Escherichia Coli Saccharomyces Cerevisiae Bacillus Subtilis はB
研究開発等に係る遺伝子組換え生物等の第二種使用等に当たって執るべき拡散防止措 置等を定める省令の規定に基づき認定宿主ベクター系等を定める件 (平成十六年一月二十九日文部科学省告示第七号) 最終改正:令和三年二月十五日文部科学省告示第十三号 (認定宿主ベクター系) 第一条 研究開発等に係る遺伝子組換え生物等の第二種使用等に当たって執るべき拡散防止 措置等を定める省令(以下「省令」という。)第二条第十三号の文部科学大臣が定める認 定宿主ベクター系は、別表第一に掲げるとおりとする。 (実験分類の区分ごとの微生物等) 第二条 省令第三条の表第一号から第四号までの文部科学大臣が定める微生物等は、別表第 二の上欄に掲げる区分について、それぞれ同表の下欄に掲げるとおりとする。 (特定認定宿主ベクター系) 第三条 省令第五条第一号ロの文部科学大臣が定める特定認定宿主ベクター系は、別表第一 の2の項に掲げる認定宿主ベクター系とする。 (自立的な増殖力及び感染力を保持したウイルス及びウイロイド) 第四条 省令別表第一第一号ヘの文部科学大臣が定めるウイルス及びウイロイドは、別表第 三に掲げるとおりとする。 別表第1(第1条関係) 区 分 名 称 宿主及びベクターの組合せ 1 B1 (1) EK1 Escherichia coli K12株、B株、C株及びW株又は これら各株の誘導体を宿主とし、プラスミド又は バクテリオファージの核酸であって、接合等によ り宿主以外の細菌に伝達されないものをベクター とするもの(次項(1)のEK2に該当するものを除 く。) (2) SC1 Saccharomyces cerevisiae又はこれと交雑可能な 分類学上の種に属する酵母を宿主とし、これらの 宿主のプラスミド、ミニクロモソーム又はこれら の誘導体をベクターとするもの(次項(2)のSC2 に該当するものを除く。) (3) BS1 Bacillus subtilis Marburg168株、この誘導体又 はB. licheniformis全株のうち、アミノ酸若しく は核酸塩基に対する複数の栄養要求性突然変異を 有する株又は胞子を形成しない株を宿主とし、こ れらの宿主のプラスミド(接合による伝達性のな いものに限る。)又はバクテリオファージの核酸 をベクターとするもの(次項(3)のBS2に該当す るものを除く。) (4) Thermus属細菌 Thermus属細菌(T. thermophilus、T. aquaticus、 T. flavus、T. caldophilus及びT. ruberに限る。) を宿主とし、これらの宿主のプラスミド又はこの 誘導体をベクターとするもの (5) Rhizobium属細菌 Rhizobium属細菌(R. radiobacter(別名Agroba- cterium tumefaciens)及びR. rhizogenes(別名 Agrobacterium rhizogenes)に限る。)を宿主と し、これらの宿主のプラスミド又はRK2系のプラ スミドをベクターとするもの (6) Pseudomonas putida Pseudomonas putida KT2440株又はこの誘導体を 宿主とし、これら宿主への依存性が高く、宿主以 外の細胞に伝達されないものをベクターとするも の (7) Streptomyces属細菌 Streptomyces属細菌(S. avermitilis、S. coel- icolor [S. violaceoruberとして分類されるS. coelicolor A3(2)株を含む]、S. lividans、S. p- arvulus、S. griseus及びS. -

Zoonotic Viruses Discovered and Isolated in Malaysia: Do They Pose Potential Risks of Zoonosis? Kenny Gah Leong Voon
Running title: BIODIVERSITY OF ZOONOTIC VIRUSES IN MALAYSIA IeJSME 2021 15 (2): 1-4 Editorial Zoonotic viruses discovered and isolated in Malaysia: Do they pose potential risks of zoonosis? Kenny Gah Leong Voon Keywords: zoonosis, viral infection, Malaysia, viral which are believed to be the reservoir of most viral zoonotic infection diseases, resulting in high spill over events to the human population. In order to focus and prioritise its efforts under its This paper aims to recapitulate the list of viruses that R&D Blueprint, the World Health Organization in were discovered and isolated in Malaysia and outline the 2018 has developed a list of diseases and pathogens potential threat of zoonosis among these viruses. These that have been prioritised for R&D in public health viruses are divided into two categories: 1) arboviruses, emergency contexts. Disease X was included in this list and 2) non-arboviruses to iterate the transmission route to represent a hypothetical, unknown disease that could of these viruses. cause a future epidemic.1 Besides the pathogen that causes Disease X, several viruses such as Ebola virus, Arboviruses Nipah virus, Influenza virus, Severe Acute Respiratory Many arboviruses are zoonotic, infecting a wide Syndrome coronavirus (SARS-CoV), Middle East variety of arthropods, other animals including birds in Respiratory Syndrome coronavirus (MERS- CoV) and their sylvatic habitats and humans as incidental hosts. others are being listed as potential candidates that may Over many years, arboviruses have evolved balanced be associated with pandemic outbreaks in the future. relationships with these sylvatic hosts. Thus, morbidity Therefore, viral zoonosis that may be caused by one of and mortality are rarely seen in these sylvatic animals these pathogens including Pathogen X in the future, 2 when they are infected by arboviruses. -

Tap Chi Sinh Hoc 2014, 36(4): 479-486 Taxonomic And
TAP CHI SINH HOC 2014, 36(4): 479-486 DOI 10.15625/0866-7160/v36n4-5980 TAXONOMIC AND DISTRIBUTIONAL ASSESSMENTS OF Chaerephonpttcatus (Chiroptera: Molossidae) FROM VIETNAM Vu Dinh Thong Institute of Ecology and Biological Resources, VAST, [email protected] ABSTRACT: To date. Wrinkle-lipped Bai (Chaerephon plicatus) is the only species ofthe family Molossidae in Vietnam. It is found throu^out much of Asia but rarely recorded in the country. Every pubhshed record of this species from Vietnam was only resulted from a single individual with little data tm morphology. Particularly, the previous publications did not mclude any information about either colony size or roosting site ofthe species within Vietnam. Between 2001 and 2014, a series of field surve)« was conducted throughout the country with an intensive search for free-tailed bat species. The obtained results indicate that Wrinkle-lipped Bat is a widespread bat species but its known roosting sites in Vietnam are quite distjunct Its colony size is in both seasonal and geographical variations ranging from several hundreds to over three million individuals. The species inhabits seasonally and permanently in northem and southem regions, respectively. This paper provides taxonomic and ecological assessments with an emphasis on morphological measurements, colony size, roosting habitats and national distributional range of Wrinkle-lipped Bat within Vietnam. Keywords: Asia, behavior, free-tailed bat, habitat. Mammalia, seasonal variation. INTRODUCTION tnolossid bats frora Virtnam was included in Wrinkle-lipped Bat (Chaerephon plicatus) Total (1974) [17] with record of one specimen is a free-tailed species, which was originally identified as Tadarida plicata. Since then, records described as Vespertilio plicatus (Buchannan of Tadarida plicata from the country has been 1800). -
Diversity, Host Specialization, and Geographic Structure of Filarial Nematodes Infecting Malagasy Bats
RESEARCH ARTICLE Diversity, Host Specialization, and Geographic Structure of Filarial Nematodes Infecting Malagasy Bats Beza Ramasindrazana1,2,3*, Koussay Dellagi1,2, Erwan Lagadec1,2, Milijaona Randrianarivelojosia4, Steven M. Goodman3,5, Pablo Tortosa1,2 1 Centre de Recherche et de Veille sur les maladies émergentes dans l’Océan Indien, Plateforme de Recherche CYROI, Sainte Clotilde, La Réunion, France, 2 Université de La Réunion, UMR PIMIT "Processus Infectieux en Milieu Insulaire Tropical", INSERM U 1187, CNRS 9192, IRD 249. Plateforme de Recherche CYROI, 97490 Sainte Clotilde, Saint-Denis, La Réunion, France, 3 Association Vahatra, Antananarivo, Madagascar, 4 Institut Pasteur de Madagascar, Antananarivo, Madagascar, 5 The Field Museum of Natural History, Chicago, Illinois, United States of America * [email protected] OPEN ACCESS Abstract Citation: Ramasindrazana B, Dellagi K, Lagadec E, We investigated filarial infection in Malagasy bats to gain insights into the diversity of these Randrianarivelojosia M, Goodman SM, Tortosa P (2016) Diversity, Host Specialization, and Geographic parasites and explore the factors shaping their distribution. Samples were obtained from Structure of Filarial Nematodes Infecting Malagasy 947 individual bats collected from 52 sites on Madagascar and representing 31 of the 44 Bats. PLoS ONE 11(1): e0145709. doi:10.1371/ species currently recognized on the island. Samples were screened for the presence of journal.pone.0145709 micro- and macro-parasites through both molecular and morphological approaches. Phylo- Editor: Karen E. Samonds, Northern Illinois genetic analyses showed that filarial diversity in Malagasy bats formed three main groups, University, UNITED STATES the most common represented by Litomosa spp. infecting Miniopterus spp. (Miniopteridae); Received: April 30, 2015 a second group infecting Pipistrellus cf. -

Diversity and Evolution of Viral Pathogen Community in Cave Nectar Bats (Eonycteris Spelaea)
viruses Article Diversity and Evolution of Viral Pathogen Community in Cave Nectar Bats (Eonycteris spelaea) Ian H Mendenhall 1,* , Dolyce Low Hong Wen 1,2, Jayanthi Jayakumar 1, Vithiagaran Gunalan 3, Linfa Wang 1 , Sebastian Mauer-Stroh 3,4 , Yvonne C.F. Su 1 and Gavin J.D. Smith 1,5,6 1 Programme in Emerging Infectious Diseases, Duke-NUS Medical School, Singapore 169857, Singapore; [email protected] (D.L.H.W.); [email protected] (J.J.); [email protected] (L.W.); [email protected] (Y.C.F.S.) [email protected] (G.J.D.S.) 2 NUS Graduate School for Integrative Sciences and Engineering, National University of Singapore, Singapore 119077, Singapore 3 Bioinformatics Institute, Agency for Science, Technology and Research, Singapore 138671, Singapore; [email protected] (V.G.); [email protected] (S.M.-S.) 4 Department of Biological Sciences, National University of Singapore, Singapore 117558, Singapore 5 SingHealth Duke-NUS Global Health Institute, SingHealth Duke-NUS Academic Medical Centre, Singapore 168753, Singapore 6 Duke Global Health Institute, Duke University, Durham, NC 27710, USA * Correspondence: [email protected] Received: 30 January 2019; Accepted: 7 March 2019; Published: 12 March 2019 Abstract: Bats are unique mammals, exhibit distinctive life history traits and have unique immunological approaches to suppression of viral diseases upon infection. High-throughput next-generation sequencing has been used in characterizing the virome of different bat species. The cave nectar bat, Eonycteris spelaea, has a broad geographical range across Southeast Asia, India and southern China, however, little is known about their involvement in virus transmission. -

Optimizing Noninvasive Sampling of a Zoonotic Bat Virus
Received: 2 November 2020 | Revised: 14 May 2021 | Accepted: 17 May 2021 DOI: 10.1002/ece3.7830 ORIGINAL RESEARCH Optimizing noninvasive sampling of a zoonotic bat virus John R. Giles1,2 | Alison J. Peel2 | Konstans Wells3 | Raina K. Plowright4 | Hamish McCallum2 | Olivier Restif5 1Department of Epidemiology, Johns Hopkins University Bloomberg School of Abstract Public Health, Baltimore, MD, USA Outbreaks of infectious viruses resulting from spillover events from bats have 2 Environmental Futures Research Institute, brought much attention to bat- borne zoonoses, which has motivated increased Griffith University, Brisbane, Qld, Australia 3Department of Biosciences, Swansea ecological and epidemiological studies on bat populations. Field sampling methods University, Swansea, UK often collect pooled samples of bat excreta from plastic sheets placed under- roosts. 4 Department of Microbiology and However, positive bias is introduced because multiple individuals may contribute to Immunology, Montana State University, Bozeman, MT, USA pooled samples, making studies of viral dynamics difficult. Here, we explore the gen- 5Disease Dynamics Unit, Department eral issue of bias in spatial sample pooling using Hendra virus in Australian bats as of Veterinary Medicine, University of a case study. We assessed the accuracy of different under- roost sampling designs Cambridge, Cambridge, UK using generalized additive models and field data from individually captured bats and Correspondence pooled urine samples. We then used theoretical simulation models of bat density John R. Giles, Department of Epidemiology, Johns Hopkins University Bloomberg School and under- roost sampling to understand the mechanistic drivers of bias. The most of Public Health, Baltimore, MD 21205, commonly used sampling design estimated viral prevalence 3.2 times higher than USA. -

A New Species of Chaerephon (Molossidae) from Madagascar with Notes on Other Members of the Family
A New Species of Chaerephon (Molossidae) from Madagascar with Notes on Other Members of the Family Authors: Goodman, Steven M., and Cardiff, Scott G. Source: Acta Chiropterologica, 6(2) : 227-248 Published By: Museum and Institute of Zoology, Polish Academy of Sciences URL: https://doi.org/10.3161/001.006.0204 BioOne Complete (complete.BioOne.org) is a full-text database of 200 subscribed and open-access titles in the biological, ecological, and environmental sciences published by nonprofit societies, associations, museums, institutions, and presses. Your use of this PDF, the BioOne Complete website, and all posted and associated content indicates your acceptance of BioOne’s Terms of Use, available at www.bioone.org/terms-of-use. Usage of BioOne Complete content is strictly limited to personal, educational, and non - commercial use. Commercial inquiries or rights and permissions requests should be directed to the individual publisher as copyright holder. BioOne sees sustainable scholarly publishing as an inherently collaborative enterprise connecting authors, nonprofit publishers, academic institutions, research libraries, and research funders in the common goal of maximizing access to critical research. Downloaded From: https://bioone.org/journals/Acta-Chiropterologica on 13 Jul 2020 Terms of Use: https://bioone.org/terms-of-use Acta Chiropterologica, 6(2): 227–248, 2004 PL ISSN 1508-1109 © Museum and Institute of Zoology PAS A new species of Chaerephon (Molossidae) from Madagascar with notes on other members of the family STEVEN M. -
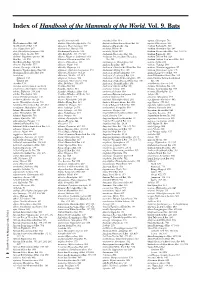
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -

Chiropterology Division BC Arizona Trial Event 1 1. DESCRIPTION: Participants Will Be Assessed on Their Knowledge of Bats, With
Chiropterology Division BC Arizona Trial Event 1. DESCRIPTION: Participants will be assessed on their knowledge of bats, with an emphasis on North American Bats, South American Microbats, and African MegaBats. A TEAM OF UP TO: 2 APPROXIMATE TIME: 50 minutes 2. EVENT PARAMETERS: a. Each team may bring one 2” or smaller three-ring binder, as measured by the interior diameter of the rings, containing information in any form and from any source. Sheet protectors, lamination, tabs and labels are permitted in the binder. b. If the event features a rotation through a series of stations where the participants interact with samples, specimens or displays; no material may be removed from the binder throughout the event. c. In addition to the binder, each team may bring one unmodified and unannotated copy of either the National Bat List or an Official State Bat list which does not have to be secured in the binder. 3. THE COMPETITION: a. The competition may be run as timed stations and/or as timed slides/PowerPoint presentation. b. Specimens/Pictures will be lettered or numbered at each station. The event may include preserved specimens, skeletal material, and slides or pictures of specimens. c. Each team will be given an answer sheet on which they will record answers to each question. d. No more than 50% of the competition will require giving common or scientific names. e. Participants should be able to do a basic identification to the level indicated on the Official List. States may have a modified or regional list. See your state website.