Bats: Important Reservoir Hosts of Emerging Viruses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Phylogeny of the Hubbardochloinae Including Tetrachaete (Poaceae: Chloridoideae: Cynodonteae)
Peterson, P.M., K. Romaschenko, and Y. Herrera Arrieta. 2020. A phylogeny of the Hubbardochloinae including Tetrachaete (Poaceae: Chloridoideae: Cynodonteae). Phytoneuron 2020-81: 1–13. Published 18 November 2020. ISSN 2153 733 A PHYLOGENY OF THE HUBBARDOCHLOINAE INCLUDING TETRACHAETE (CYNODONTEAE: CHLORIDOIDEAE: POACEAE) PAUL M. PETERSON AND KONSTANTIN ROMASCHENKO Department of Botany National Museum of Natural History Smithsonian Institution Washington, D.C. 20013-7012 [email protected]; [email protected] YOLANDA HERRERA ARRIETA Instituto Politécnico Nacional CIIDIR Unidad Durango-COFAA Durango, C.P. 34220, México [email protected] ABSTRACT The phylogeny of subtribe Hubbardochloinae is revisited, here with the inclusion of the monotypic genus Tetrachaete, based on a molecular DNA analysis using ndhA intron, rpl32-trnL, rps16 intron, rps16- trnK, and ITS markers. Tetrachaete elionuroides is aligned within the Hubbardochloinae and is sister to Dignathia. The biogeography of the Hubbardochloinae is discussed, its origin likely in Africa or temperate Asia. In a previous molecular DNA phylogeny (Peterson et al. 2016), the subtribe Hubbardochloinae Auquier [Bewsia Gooss., Dignathia Stapf, Gymnopogon P. Beauv., Hubbardochloa Auquier, Leptocarydion Hochst. ex Stapf, Leptothrium Kunth, and Lophacme Stapf] was found in a clade with moderate support (BS = 75, PP = 1.00) sister to the Farragininae P.M. Peterson et al. In the present study, Tetrachaete elionuroides Chiov. is included in a phylogenetic analysis (using ndhA intron, rpl32- trnL, rps16 intron, rps16-trnK, and ITS DNA markers) in order to test its relationships within the Cynodonteae with heavy sampling of species in the supersubtribe Gouiniodinae P.M. Peterson & Romasch. Chiovenda (1903) described Tetrachaete Chiov. with a with single species, T. -

Synanthropy of Wild Mammals As a Determinant of Emerging Infectious Diseases in the Asian–Australasian Region
EcoHealth 9, 24–35, 2012 DOI: 10.1007/s10393-012-0763-9 Ó 2012 International Association for Ecology and Health Original Contribution Synanthropy of Wild Mammals as a Determinant of Emerging Infectious Diseases in the Asian–Australasian Region Ro McFarlane,1 Adrian Sleigh,1 and Tony McMichael1 National Centre for Epidemiology and Population Health, ANU College of Medicine, Biology and Environment, Australian National University, Canberra, Australia; [email protected]; [email protected] Abstract: Humans create ecologically simplified landscapes that favour some wildlife species, but not others. Here, we explore the possibility that those species that tolerate or do well in human-modified environments, or ‘synanthropic’ species, are predominantly the hosts of zoonotic emerging and re-emerging infectious diseases (EIDs). We do this using global wildlife conservation data and wildlife host information extracted from systematically reviewed emerging infectious disease literature. The evidence for this relationship is examined with special emphasis on the Australasian, South East Asian and East Asian regions. We find that synanthropic wildlife hosts are approximately 15 times more likely than other wildlife in this region to be the source of emerging infectious diseases, and this association is essentially independent of the taxonomy of the species. A significant positive association with EIDs is also evident for those wildlife species of low conservation risk. Since the increase and spread of native and introduced species able to adapt to human-induced landscape change is at the expense of those species most vulnerable to habitat loss, our findings suggest a mechanism linking land conversion, global decline in biodiversity and a rise in EIDs of wildlife origin. -

Zoonotic Viruses Discovered and Isolated in Malaysia: Do They Pose Potential Risks of Zoonosis? Kenny Gah Leong Voon
Running title: BIODIVERSITY OF ZOONOTIC VIRUSES IN MALAYSIA IeJSME 2021 15 (2): 1-4 Editorial Zoonotic viruses discovered and isolated in Malaysia: Do they pose potential risks of zoonosis? Kenny Gah Leong Voon Keywords: zoonosis, viral infection, Malaysia, viral which are believed to be the reservoir of most viral zoonotic infection diseases, resulting in high spill over events to the human population. In order to focus and prioritise its efforts under its This paper aims to recapitulate the list of viruses that R&D Blueprint, the World Health Organization in were discovered and isolated in Malaysia and outline the 2018 has developed a list of diseases and pathogens potential threat of zoonosis among these viruses. These that have been prioritised for R&D in public health viruses are divided into two categories: 1) arboviruses, emergency contexts. Disease X was included in this list and 2) non-arboviruses to iterate the transmission route to represent a hypothetical, unknown disease that could of these viruses. cause a future epidemic.1 Besides the pathogen that causes Disease X, several viruses such as Ebola virus, Arboviruses Nipah virus, Influenza virus, Severe Acute Respiratory Many arboviruses are zoonotic, infecting a wide Syndrome coronavirus (SARS-CoV), Middle East variety of arthropods, other animals including birds in Respiratory Syndrome coronavirus (MERS- CoV) and their sylvatic habitats and humans as incidental hosts. others are being listed as potential candidates that may Over many years, arboviruses have evolved balanced be associated with pandemic outbreaks in the future. relationships with these sylvatic hosts. Thus, morbidity Therefore, viral zoonosis that may be caused by one of and mortality are rarely seen in these sylvatic animals these pathogens including Pathogen X in the future, 2 when they are infected by arboviruses. -

2020 Special Issue
Journal Home page : www.jeb.co.in « E-mail : [email protected] Original Research Journal of Environmental Biology TM p-ISSN: 0254-8704 e-ISSN: 2394-0379 JEB CODEN: JEBIDP DOI : http://doi.org/10.22438/jeb/4(SI)/MS_1904 Plagiarism Detector Grammarly New records and present status of bat fauna in Mizoram, North-Eastern India C. Vanlalnghaka Department of Zoology, Govt. Serchhip College, Mizoram–796 181, India *Corresponding Author Email : [email protected] Paper received: 08.12.2019 Revised received: 24.06.2020 Accepted: 10.07.2020 Abstract Aim: The present study aimed to investigate the diversity of bat fauna in Mizoram and prepare a checklist for future references. This study also investigated threats and suggested recommendations for implementing conservation measures for bat fauna in Mizoram. Methodology: The present study was carried out in different parts of Mizoram between January 2012 - October 2019. Bats were trapped by using mist nets and hoop nets. Diagnostic morphological characters of bat were used for species identification. Digital camera and video camera were also used for further identification and documentation of bats. Results: During January 2012 – December 2016, eighteen bat species were identified. Recently, from January 2017 - October 2019 insectivorous bat species, Scotomanes ornatus was first time documented in Serchhip District (23.3 ºN 92.83 ºE), Mizoram. In total nineteen bat species were identified in this study, out of which ten species were first time recorded and nine species were rediscovered from the previous documentation. From the previous and present data, total of thirty-six bat Study the diversity of bat fauna and prepared checklist in species were recorded in Mizoram- nine Mizoram. -

The Australasian Bat Society Newsletter, Number 31, Nov 2008
The Australasian Bat Society Newsletter, Number 31, Nov 2008 The Australasian Bat Society Newsletter Number 39 November 2012 ABS Website: http://abs.ausbats.org.au ABS Discussion list - email: [email protected] ISSN 1448-5877 © Copyright The Australasian Bat Society, Inc. (2012) The Australasian Bat Society Newsletter, Number 31, Nov 2008 The Australasian Bat Society Newsletter, Number 39, November 2012 – Instructions for Contributors – The Australasian Bat Society Newsletter will accept contributions under one of the following two sections: Research Papers, and all other articles or notes. There are two deadlines each year: 10th March for the April issue, and 10th October for the November issue. The Editor reserves the right to hold over contributions for subsequent issues of the Newsletter, and meeting the deadline is not a guarantee of immediate publication. Opinions expressed in contributions to the Newsletter are the responsibility of the author, and do not necessarily reflect the views of the Australasian Bat Society, its Executive or members. For consistency, the following guidelines should be followed: Emailed electronic copy of manuscripts or articles, sent as an attachment, is the preferred method of submission. Faxed and hard copy manuscripts will be accepted but reluctantly! Please send all submissions to the Newsletter Editor at the email or postal address below. Electronic copy should be in 11 point Arial font, left and right justified with 16 mm left and right margins. Please use Microsoft Word; any version is acceptable. Manuscripts should be submitted in clear, concise English and free from typographical and spelling errors. Please leave two spaces after each sentence. -

Diversity and Evolution of Viral Pathogen Community in Cave Nectar Bats (Eonycteris Spelaea)
viruses Article Diversity and Evolution of Viral Pathogen Community in Cave Nectar Bats (Eonycteris spelaea) Ian H Mendenhall 1,* , Dolyce Low Hong Wen 1,2, Jayanthi Jayakumar 1, Vithiagaran Gunalan 3, Linfa Wang 1 , Sebastian Mauer-Stroh 3,4 , Yvonne C.F. Su 1 and Gavin J.D. Smith 1,5,6 1 Programme in Emerging Infectious Diseases, Duke-NUS Medical School, Singapore 169857, Singapore; [email protected] (D.L.H.W.); [email protected] (J.J.); [email protected] (L.W.); [email protected] (Y.C.F.S.) [email protected] (G.J.D.S.) 2 NUS Graduate School for Integrative Sciences and Engineering, National University of Singapore, Singapore 119077, Singapore 3 Bioinformatics Institute, Agency for Science, Technology and Research, Singapore 138671, Singapore; [email protected] (V.G.); [email protected] (S.M.-S.) 4 Department of Biological Sciences, National University of Singapore, Singapore 117558, Singapore 5 SingHealth Duke-NUS Global Health Institute, SingHealth Duke-NUS Academic Medical Centre, Singapore 168753, Singapore 6 Duke Global Health Institute, Duke University, Durham, NC 27710, USA * Correspondence: [email protected] Received: 30 January 2019; Accepted: 7 March 2019; Published: 12 March 2019 Abstract: Bats are unique mammals, exhibit distinctive life history traits and have unique immunological approaches to suppression of viral diseases upon infection. High-throughput next-generation sequencing has been used in characterizing the virome of different bat species. The cave nectar bat, Eonycteris spelaea, has a broad geographical range across Southeast Asia, India and southern China, however, little is known about their involvement in virus transmission. -

Optimizing Noninvasive Sampling of a Zoonotic Bat Virus
Received: 2 November 2020 | Revised: 14 May 2021 | Accepted: 17 May 2021 DOI: 10.1002/ece3.7830 ORIGINAL RESEARCH Optimizing noninvasive sampling of a zoonotic bat virus John R. Giles1,2 | Alison J. Peel2 | Konstans Wells3 | Raina K. Plowright4 | Hamish McCallum2 | Olivier Restif5 1Department of Epidemiology, Johns Hopkins University Bloomberg School of Abstract Public Health, Baltimore, MD, USA Outbreaks of infectious viruses resulting from spillover events from bats have 2 Environmental Futures Research Institute, brought much attention to bat- borne zoonoses, which has motivated increased Griffith University, Brisbane, Qld, Australia 3Department of Biosciences, Swansea ecological and epidemiological studies on bat populations. Field sampling methods University, Swansea, UK often collect pooled samples of bat excreta from plastic sheets placed under- roosts. 4 Department of Microbiology and However, positive bias is introduced because multiple individuals may contribute to Immunology, Montana State University, Bozeman, MT, USA pooled samples, making studies of viral dynamics difficult. Here, we explore the gen- 5Disease Dynamics Unit, Department eral issue of bias in spatial sample pooling using Hendra virus in Australian bats as of Veterinary Medicine, University of a case study. We assessed the accuracy of different under- roost sampling designs Cambridge, Cambridge, UK using generalized additive models and field data from individually captured bats and Correspondence pooled urine samples. We then used theoretical simulation models of bat density John R. Giles, Department of Epidemiology, Johns Hopkins University Bloomberg School and under- roost sampling to understand the mechanistic drivers of bias. The most of Public Health, Baltimore, MD 21205, commonly used sampling design estimated viral prevalence 3.2 times higher than USA. -

Annex I: Mammal & Bird Species of the NNT Area
Annex H: Forest & VegetationEAMP Annexes Types Annex I: Mammal & Bird Species of the NNT Area his annex lists all species of mammals and birds that have Francis, C.M., A. Guillén and M. F. Robinson 1999b. Order Chiri- been found either certainly or provisionally, on the Nakai optera: bats. Pp. 225-235 in Duckworth et al. (q.v.). Plateau and in the NNT NBCA. Many more species are T Ounekham, K. and S. Inthapatha, 2003. Important Bird Areas in Lao likely to occur, but there is insufficient local ecological informa- PDR. Vientiane: DoF/BirdLife International/WCS. tion available for many of those recorded in adjacent parts of Lao PDR to predict whether or not they would be likely to occur on the Robichaud, W. and Stuart, B. L. 1999. Summary of Saola, herpeto- plateau and/or in the NBCA. logical and wildlife trade studies in Nakai--Nam Theun NBCA and the proposed Nam Theun Extension. Unpublished WCS report to IUCN. List of Species (Code R) Robinson, M. F., Jenkins, P. D., Francis, C. M. and Fulford, A. The list of species is based on the following references, assigned a J. C. 2003. A new species of the Hipposideros pra�i group (Chiroptera, single-le�er code for use in the table indicating presence in Nakai- Hipposideridae) from Lao PDR and Vietnam. Acta chiropodologica 5: -Nam Theun NBCA (NNT) or the Nakai Plateau (NP). One source 31-48. (Code F) only is cited for each site; provisional identifications are bracketed Thewlis, R. M., Timmins, R. J., Evans, T. D. and Duckworth, J. -
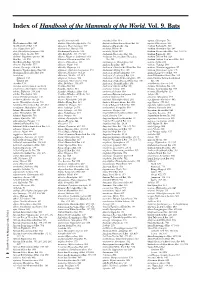
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -

A Checklist of the Mammals of South-East Asia
A Checklist of the Mammals of South-east Asia A Checklist of the Mammals of South-east Asia PHOLIDOTA Pangolin (Manidae) 1 Sunda Pangolin (Manis javanica) 2 Chinese Pangolin (Manis pentadactyla) INSECTIVORA Gymnures (Erinaceidae) 3 Moonrat (Echinosorex gymnurus) 4 Short-tailed Gymnure (Hylomys suillus) 5 Chinese Gymnure (Hylomys sinensis) 6 Large-eared Gymnure (Hylomys megalotis) Moles (Talpidae) 7 Slender Shrew-mole (Uropsilus gracilis) 8 Kloss's Mole (Euroscaptor klossi) 9 Large Chinese Mole (Euroscaptor grandis) 10 Long-nosed Chinese Mole (Euroscaptor longirostris) 11 Small-toothed Mole (Euroscaptor parvidens) 12 Blyth's Mole (Parascaptor leucura) 13 Long-tailed Mole (Scaptonyx fuscicauda) Shrews (Soricidae) 14 Lesser Stripe-backed Shrew (Sorex bedfordiae) 15 Myanmar Short-tailed Shrew (Blarinella wardi) 16 Indochinese Short-tailed Shrew (Blarinella griselda) 17 Hodgson's Brown-toothed Shrew (Episoriculus caudatus) 18 Bailey's Brown-toothed Shrew (Episoriculus baileyi) 19 Long-taied Brown-toothed Shrew (Episoriculus macrurus) 20 Lowe's Brown-toothed Shrew (Chodsigoa parca) 21 Van Sung's Shrew (Chodsigoa caovansunga) 22 Mole Shrew (Anourosorex squamipes) 23 Himalayan Water Shrew (Chimarrogale himalayica) 24 Styan's Water Shrew (Chimarrogale styani) Page 1 of 17 Database: Gehan de Silva Wijeyeratne, www.jetwingeco.com A Checklist of the Mammals of South-east Asia 25 Malayan Water Shrew (Chimarrogale hantu) 26 Web-footed Water Shrew (Nectogale elegans) 27 House Shrew (Suncus murinus) 28 Pygmy White-toothed Shrew (Suncus etruscus) 29 South-east -

ICTV Code Assigned: 2011.001Ag Officers)
This form should be used for all taxonomic proposals. Please complete all those modules that are applicable (and then delete the unwanted sections). For guidance, see the notes written in blue and the separate document “Help with completing a taxonomic proposal” Please try to keep related proposals within a single document; you can copy the modules to create more than one genus within a new family, for example. MODULE 1: TITLE, AUTHORS, etc (to be completed by ICTV Code assigned: 2011.001aG officers) Short title: Change existing virus species names to non-Latinized binomials (e.g. 6 new species in the genus Zetavirus) Modules attached 1 2 3 4 5 (modules 1 and 9 are required) 6 7 8 9 Author(s) with e-mail address(es) of the proposer: Van Regenmortel Marc, [email protected] Burke Donald, [email protected] Calisher Charles, [email protected] Dietzgen Ralf, [email protected] Fauquet Claude, [email protected] Ghabrial Said, [email protected] Jahrling Peter, [email protected] Johnson Karl, [email protected] Holbrook Michael, [email protected] Horzinek Marian, [email protected] Keil Guenther, [email protected] Kuhn Jens, [email protected] Mahy Brian, [email protected] Martelli Giovanni, [email protected] Pringle Craig, [email protected] Rybicki Ed, [email protected] Skern Tim, [email protected] Tesh Robert, [email protected] Wahl-Jensen Victoria, [email protected] Walker Peter, [email protected] Weaver Scott, [email protected] List the ICTV study group(s) that have seen this proposal: A list of study groups and contacts is provided at http://www.ictvonline.org/subcommittees.asp . -

Investigating the Role of Bats in Emerging Zoonoses
12 ISSN 1810-1119 FAO ANIMAL PRODUCTION AND HEALTH manual INVESTIGATING THE ROLE OF BATS IN EMERGING ZOONOSES Balancing ecology, conservation and public health interest Cover photographs: Left: © Jon Epstein. EcoHealth Alliance Center: © Jon Epstein. EcoHealth Alliance Right: © Samuel Castro. Bureau of Animal Industry Philippines 12 FAO ANIMAL PRODUCTION AND HEALTH manual INVESTIGATING THE ROLE OF BATS IN EMERGING ZOONOSES Balancing ecology, conservation and public health interest Edited by Scott H. Newman, Hume Field, Jon Epstein and Carol de Jong FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2011 Recommended Citation Food and Agriculture Organisation of the United Nations. 2011. Investigating the role of bats in emerging zoonoses: Balancing ecology, conservation and public health interests. Edited by S.H. Newman, H.E. Field, C.E. de Jong and J.H. Epstein. FAO Animal Production and Health Manual No. 12. Rome. The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. The views expressed in this information product are those of the author(s) and do not necessarily reflect the views of FAO.