Herbalism, Phytochemistry and Ethnopharmacology Herbalism, Phytochemistry and Ethnopharmacology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Developmental Biology and Population Studies on the Citrus Psylla Trioza Erytreae (Del Guercio) (Hemiptera : Triozidae)
Frets - vol. 47, n°5 . 1992 58 3 Developmental Biology and Population Studies on the Citrus Psylla Trioza erytreae (Del Guercio) (Hemiptera : Triozidae) M.A . VAN DEN BERG and Valerie E . DEACON * Biologie du développement et études des populations du psylle des Developmental Biology and Population Studies on the Citrus Psyll a agtines Trioza erytreae (Del Guercio) (Hemiptera : Triozidae). Trioza erytreae (Del Guercio) (Hemiptera : Triozidae). M .A. VAN DEN BERG and Valerie E. DEACO N M .A . VAN I)EN BERG and Valerie E . DEACO N Fruit, vol . 47, n° 5, p . 583-589 . Fruits, vol . 47, n° 5, p . 583-589. RESUME - A une température journalière moyenne de 20,8 °C, les oeufs ABSTRACT - At a daily mean temperature of 20.8°C, Citrus psylla egg s de Trio_a erytreae, le psylle africain des agrumes, éclosent au bout d e hatched after 7 days and the nymphal stage was completed within 18 t o 7 jours et le déroulement du cycle larvaire s ' effectue en 18 à 23 jours . Les 23 days . Field populations in the Hazyview area were either rising or taux d ' abondance de population au champ dans la région de Hazyvie w declining when the egg/nymph/adult ratios increased above or decline d augmentent ou diminuent quand les rapports de pullulation entre les oeufs, below about 15 :13 :1 respectively . The K-value between the egg and les larves et les adultes augmentent ou diminuent dans des proportions nymph counts was 0.55 and between the nymph and adult counts 0.63 . A 15 :13 :1 . -

The Effects of an Aqueous Leaf Extract of Clausena Anisata (Willd.) Hook.F.Ex Benth
Vol. 10(28), pp. 425-434, 25 July, 2016 DOI: 10.5897/JMPR2016.6135 Article Number: 14ED35759651 ISSN 1996-0875 Journal of Medicinal Plants Research Copyright © 2016 Author(s) retain the copyright of this article http://www.academicjournals.org/JMPR Full Length Research Paper The effects of an aqueous leaf extract of Clausena anisata (Willd.) Hook.f.ex Benth. on blood pressure, urine output, angiotensin II levels and cardiac parameters in spontaneously hypertensive rats Ntamo MacDonald Tshepo Lechaba, Paul Jacobus Schutte*, Leon Hay, Linde Böhmer and Melvin Megandran Govender Department of Human Physiology, Sefako Makgatho Health Sciences University,P. O. Box 130, Medunsa, 0204, South Africa. Received 26 April, 2016; Accepted 11 July, 2016 Clausena anisata (Willd.) Hook.f. ex Benth (Rutaceae) is a medicinal plant indigenous to Southern Africa and scientific studies report on its biomedical activities and possible antihypertensive property by demonstrating in vitro angiotensin converting enzyme inhibition. This study investigated the antihypertensive effects of an aqueous leaf extract of Clausena anisata in a spontaneously hypertensive rat model, and determined whether these blood pressure lowering effects could be attributed to diuresis, the inhibition of the renin-angiotensin-aldosterone blood pressure control system and/or possible negative inotropic or chronotropic cardiac effects. Aqueous extracts were prepared from ground leaves of Clausena anisata. Four groups of ten rats each received 50, 100, 200 or 400 mg/kg.bw of aqueous extracts intra-arterially respectively to obtain a dose response relationship. Another two groups of fifteen rats each received either plain water (control group) or the plant extract added to their drinking water (experimental group) for 40 days. -
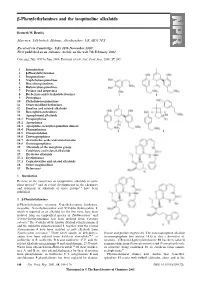
Β-Phenylethylamines and the Isoquinoline Alkaloids
-Phenylethylamines and the isoquinoline alkaloids Kenneth W. Bentley Marrview, Tillybirloch, Midmar, Aberdeenshire, UK AB51 7PS Received (in Cambridge, UK) 28th November 2000 First published as an Advance Article on the web 7th February 2001 Covering: July 1999 to June 2000. Previous review: Nat. Prod. Rep., 2000, 17, 247. 1 Introduction 2 -Phenylethylamines 3 Isoquinolines 4 Naphthylisoquinolines 5 Benzylisoquinolines 6 Bisbenzylisoquinolines 7 Pavines and isopavines 8 Berberines and tetrahydoberberines 9 Protopines 10 Phthalide-isoquinolines 11 Other modified berberines 12 Emetine and related alkaloids 13 Benzophenanthridines 14 Aporphinoid alkaloids 14.1 Proaporphines 14.2 Aporphines 14.3 Aporphine–benzylisoquinoline dimers 14.4 Phenanthrenes 14.5 Oxoaporphines 14.6 Dioxoaporphines 14.7 Aristolochic acids and aristolactams 14.8 Oxoisoaporphines 15 Alkaloids of the morphine group 16 Colchicine and related alkaloids 17 Erythrina alkaloids 17.1 Erythrinanes 17.2 Cephalotaxine and related alkaloids 18 Other isoquinolines 19 References 1 Introduction Reviews of the occurrence of isoquinoline alkaloids in some plant species 1,2 and of recent developments in the chemistry and synthesis of alkaloids of these groups 3–6 have been published. 2 -Phenylethylamines β-Phenylethylamine, tyramine, N-methyltyramine, hordenine, mescaline, N-methylmescaline and N,N-dimethylmescaline 1, which is reported as an alkaloid for the first time, have been isolated from an unspecified species of Turbinocarpus 7 and N-trans-feruloyltyramine has been isolated from Cananga odorata.8 The N-oxides of the known alkaloid culantraramine 2 and the unknown culantraraminol 3, together with the related avicennamine 4 have been isolated as new alkaloids from Zanthoxylum avicennae.9 Three novel amides of dehydrotyr- leucine and proline respectively. -

Treatment Protocol Copyright © 2018 Kostoff Et Al
Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al PREVENTION AND REVERSAL OF ALZHEIMER'S DISEASE: TREATMENT PROTOCOL by Ronald N. Kostoffa, Alan L. Porterb, Henry. A. Buchtelc (a) Research Affiliate, School of Public Policy, Georgia Institute of Technology, USA (b) Professor Emeritus, School of Public Policy, Georgia Institute of Technology, USA (c) Associate Professor, Department of Psychiatry, University of Michigan, USA KEYWORDS Alzheimer's Disease; Dementia; Text Mining; Literature-Based Discovery; Information Technology; Treatments Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al CITATION TO MONOGRAPH Kostoff RN, Porter AL, Buchtel HA. Prevention and reversal of Alzheimer's disease: treatment protocol. Georgia Institute of Technology. 2018. PDF. https://smartech.gatech.edu/handle/1853/59311 COPYRIGHT AND CREATIVE COMMONS LICENSE COPYRIGHT Copyright © 2018 by Ronald N. Kostoff, Alan L. Porter, Henry A. Buchtel Printed in the United States of America; First Printing, 2018 CREATIVE COMMONS LICENSE This work can be copied and redistributed in any medium or format provided that credit is given to the original author. For more details on the CC BY license, see: http://creativecommons.org/licenses/by/4.0/ This work is licensed under a Creative Commons Attribution 4.0 International License<http://creativecommons.org/licenses/by/4.0/>. DISCLAIMERS The views in this monograph are solely those of the authors, and do not represent the views of the Georgia Institute of Technology or the University of Michigan. This monograph is not intended as a substitute for the medical advice of physicians. The reader should regularly consult a physician in matters relating to his/her health and particularly with respect to any symptoms that may require diagnosis or medical attention. -

Mixed Antagonistic Effects of the Ginkgolides at Recombinant Human R1 GABAC Receptors
Neuropharmacology 63 (2012) 1127e1139 Contents lists available at SciVerse ScienceDirect Neuropharmacology journal homepage: www.elsevier.com/locate/neuropharm Mixed antagonistic effects of the ginkgolides at recombinant human r1 GABAC receptors Shelley H. Huang a, Trevor M. Lewis b, Sarah C.R. Lummis c, Andrew J. Thompson c, Mary Chebib d, Graham A.R. Johnston a, Rujee K. Duke a,* a Discipline of Pharmacology, School of Medical Sciences, Faculty of Medicine, University of Sydney, Australia b School of Medical Sciences, University of New South Wales, Australia c Department of Biochemistry, University of Cambridge, Cambridge, United Kingdom d Faculty of Pharmacy, University of Sydney, Australia article info abstract Article history: The diterpene lactones of Ginkgo biloba, ginkgolides A, B and C are antagonists at a range of Cys-loop Received 11 July 2011 receptors. This study examined the effects of the ginkgolides at recombinant human r1 GABAC recep- Received in revised form tors expressed in Xenopus oocytes using two-electrode voltage clamp. The ginkgolides were moderately 18 June 2012 potent antagonists with IC sinthemM range. At 10 mM, 30 mM and 100 mM, the ginkgolides caused Accepted 24 June 2012 50 rightward shifts of GABA doseeresponse curves and reduced maximal GABA responses, characteristic of noncompetitive antagonists, while the potencies showed a clear dependence on GABA concentration, Keywords: indicating apparent competitive antagonism. This suggests that the ginkgolides exert a mixed-type Ginkgolide Bilobalide antagonism at the r1 GABAC receptors. The ginkgolides did not exhibit any obvious use-dependent Mixed-antagonism inhibition. Fitting of the data to a number of kinetic schemes suggests an allosteric inhibition as Use-dependent a possible mechanism of action of the ginkgolides which accounts for their inhibition of the responses GABAr receptor without channel block or use-dependent inhibition. -

World Journal of Pharmaceutical Research Vangalapati Et Al
World Journal of Pharmaceutical ReseaRch Vangalapati et al. World Journal of Pharmaceutical SJIF Research Impact Factor 5.045 Volume 3, Issue 6, 2127-2139. Review Article ISSN 2277 – 7105 A REVIEW ON CHEBULINIC ACID FROM MEDICINAL HERBS Surya Prakash DV1 and Meena Vangalapati2* 1 Research scholar, Centre for Biotechnology, Department of Chemical Engineering, Andhra University, Visakhapatnam-530003, Andhra Pradesh, India. 2* Associate Professor, Centre for Biotechnology, Department of Chemical Engineering, Andhra University, Visakhapatnam-530003, Andhra Pradesh, India. Article Received on ABSTRACT 30 June 2014, Chebulinic acid is a phenolic compound found in the fruits of Revised on 25 July 2014, Accepted on 20 August 2014 Terminalia chebula (Haritaki), Phyllanthus emblica (Amla) and seeds of Dimocarpus longan (Longan) species etc. It’s also known as 1,3,6- *Correspondence for Tri-O-galloyl-2,4-chebuloyl-β-D-glucopyranoside. Chebulinic acid is Author extracted from the medicinal herbs using soxhlet extractor, column Dr. Meena Vangalapati chromatography and high pressure liquid chromatography (HPLC) etc. Associate Professor, Centre for It showed many pharmacological activities including inhibition of Biotechnology, Department of cancer cell growth like human leukemia K562 cells, colon Chemical Engineering, Andhra University, adenocarcinoma HT-29 cell lines, anti-neisseria gonorrhoeae activity, Visakhapatnam-530003, inhibiting the contractile responses of cardiovascular muscles activities Andhra Pradesh, India. etc. KEY WORDS: Chebulinic acid, Terminalia chebula, Dimocarpus longan, Phyllanthus emblica, Anticancer activity, HPLC, Astringency. INTRODUCTION Chebulinic acid is a phenolic compound [1,2] commonly found in the fruits of Terminalia chebula, leaves and fruits of Phyllanthus emblica and seeds of Dimocarpus longan species, which has many potential uses in medicine. -

Molecular Docking Studies of Medicinal Compounds Against Aldose Reductase Drug Target for Treatment of Type 2 Diabetes Pratistha Singh*1, Preeti Yadav2, V.K
Intl. J. Bioinformatics and Biological Sci.: (V. 5 n.2, p. 91-116): December 2017 ©2017 New Delhi Publishers. All rights reserved DOI: 10.5958/2321-7111.2017.00012.9 Molecular Docking Studies of Medicinal Compounds against Aldose reductase Drug Target for Treatment of Type 2 Diabetes Pratistha Singh*1, Preeti Yadav2, V.K. Singh3 and A.K. Singh1 1Department of Dravyaguna, Faculty of Ayurveda, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India 2School of Biotechnology, Institute of Science, Banaras Hindu University, Varanasi, India 3Centre for Bioinformatics, School of Biotechnology, Institute of Science, Banaras Hindu University, Varanasi, India *Corresponding author: [email protected] ABSTRACT Type 2 Diabetes is a disease that manifests from combined effect of genetic and environmental stress on multiple tissues over a period of time. An enzyme, Aldose Reductase play an important role in oxidative stress and Diabetic Mellitus was selected as a target protein for in silico screening of suitable herbal inhibitors using molecular docking. In the present work best screened ligands Ajoene, 3-O-methyl-D-chiro-inositol (D-pinitol), Butein, Leucopelargonidin, Nimbidinin, Tolbutamide and Coumarin were used for docking calculation and isolated from Allium sativum, Glycine max, Butea monosperma, Thepsia populena, Ficus benghalensis, Azardirachta indica, Nelumbo nucifera, Aegle marmelos respectively. Herbacetin and Quercetin from Thepsia populena. The residues Gly18, Thr19, Trp20, Lys21, Asp43,Val47, Tyr48, Gln49, Asn50, Lys77, His110, Trp111, Thr113, Ser159, Asn160, Asn162, His163, Gln183, Tyr209, Ser210, Pro211, Leu212, Gly213, Ser214, Pro215, Asp216, Ala245, Ile260, Val264, Thr265, Arg268, Glu261, Asn262, Cys298, Ala299 and Leu300 were found conserved with binding site 1, which is major active site involved in interaction. -

Photodynamic Therapy for Cancer Role of Natural Products
Photodiagnosis and Photodynamic Therapy 26 (2019) 395–404 Contents lists available at ScienceDirect Photodiagnosis and Photodynamic Therapy journal homepage: www.elsevier.com/locate/pdpdt Review Photodynamic therapy for cancer: Role of natural products T Behzad Mansooria,b,d, Ali Mohammadia,d, Mohammad Amin Doustvandia, ⁎ Fatemeh Mohammadnejada, Farzin Kamaric, Morten F. Gjerstorffd, Behzad Baradarana, , ⁎⁎ Michael R. Hambline,f,g, a Immunology Research Center, Tabriz University of Medical Sciences, Tabriz, Iran b Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran c Neurosciences Research Center, Tabriz University of Medical Sciences, Tabriz, Iran d Department of Cancer and Inflammation Research, Institute for Molecular Medicine, University of Southern Denmark, 5000, Odense, Denmark e Wellman Center for Photomedicine, Massachusetts General Hospital, Boston, MA 02114, USA f Department of Dermatology, Harvard Medical School, Boston, MA 02115, USA g Harvard-MIT Division of Health Sciences and Technology, Cambridge, MA 02139, USA ARTICLE INFO ABSTRACT Keywords: Photodynamic therapy (PDT) is a promising modality for the treatment of cancer. PDT involves administering a Photodynamic therapy photosensitizing dye, i.e. photosensitizer, that selectively accumulates in tumors, and shining a light source on Photosensitizers the lesion with a wavelength matching the absorption spectrum of the photosensitizer, that exerts a cytotoxic Herbal medicine effect after excitation. The reactive oxygen species produced during PDT are responsible for the oxidation of Natural products biomolecules, which in turn cause cell death and the necrosis of malignant tissue. PDT is a multi-factorial process that generally involves apoptotic death of the tumor cells, degeneration of the tumor vasculature, stimulation of anti-tumor immune response, and induction of inflammatory reactions in the illuminated lesion. -

Effects of the Putative Antipsychotic Alstonine on Glutamate Uptake in Acute Hippocampal Slices ⇑ Ana P
Neurochemistry International 61 (2012) 1144–1150 Contents lists available at SciVerse ScienceDirect Neurochemistry International journal homepage: www.elsevier.com/locate/nci Effects of the putative antipsychotic alstonine on glutamate uptake in acute hippocampal slices ⇑ Ana P. Herrmann a,b, , Paula Lunardi b, Luísa Klaus Pilz a, Ana C. Tramontina b, Viviane M. Linck a,b, Christopher O. Okunji c, Carlos A. Gonçalves b, Elaine Elisabetsky a,b a Laboratório de Etnofarmacologia, Departamento de Farmacologia, Instituto de Ciências Básicas da Saúde, Universidade Federal do Rio Grande do Sul, Rua Sarmento Leite, 500, 90050-170 Porto Alegre, RS, Brazil b Programa de Pós-graduação em Ciências Biológicas: Bioquímica, Instituto de Ciências Básicas da Saúde, Universidade Federal do Rio Grande do Sul, Rua Ramiro Barcelos, 2600, 90035-000 Porto Alegre, RS, Brazil c International Centre for Ethnomedicine and Drug Development (InterCEDD), Nsukka, Enugu State, Nigeria article info abstract Article history: A dysfunctional glutamatergic system is thought to be central to the negative symptoms and cognitive Received 8 March 2012 deficits recognized as determinant to the poor quality of life of people with schizophrenia. Modulating Received in revised form 13 August 2012 glutamate uptake has, thus, been suggested as a novel target for antipsychotics. Alstonine is an indole Accepted 15 August 2012 alkaloid sharing with atypical antipsychotics the profile in animal models relevant to schizophrenia, Available online 25 August 2012 though divergent in its mechanism of action. The aim of this study was to evaluate the effects of alstonine on glutamate uptake. Additionally, the effects on glutathione content and extracellular S100B levels were Keywords: assessed. -

An in Silico Study of the Ligand Binding to Human Cytochrome P450 2D6
AN IN SILICO STUDY OF THE LIGAND BINDING TO HUMAN CYTOCHROME P450 2D6 Sui-Lin Mo (Doctor of Philosophy) Discipline of Chinese Medicine School of Health Sciences RMIT University, Victoria, Australia January 2011 i Declaration I hereby declare that this submission is my own work and to the best of my knowledge it contains no materials previously published or written by another person, or substantial proportions of material which have been accepted for the award of any other degree or diploma at RMIT university or any other educational institution, except where due acknowledgment is made in the thesis. Any contribution made to the research by others, with whom I have worked at RMIT university or elsewhere, is explicitly acknowledged in the thesis. I also declare that the intellectual content of this thesis is the product of my own work, except to the extent that assistance from others in the project‘s design and conception or in style, presentation and linguistic expression is acknowledged. PhD Candidate: Sui-Lin Mo Date: January 2011 ii Acknowledgements I would like to take this opportunity to express my gratitude to my supervisor, Professor Shu-Feng Zhou, for his excellent supervision. I thank him for his kindness, encouragement, patience, enthusiasm, ideas, and comments and for the opportunity that he has given me. I thank my co-supervisor, A/Prof. Chun-Guang Li, for his valuable support, suggestions, comments, which have contributed towards the success of this thesis. I express my great respect to Prof. Min Huang, Dean of School of Pharmaceutical Sciences at Sun Yat-sen University in P.R.China, for his valuable support. -

Natural Hydroxyanthraquinoid Pigments As Potent Food Grade Colorants: an Overview
Review Nat. Prod. Bioprospect. 2012, 2, 174–193 DOI 10.1007/s13659-012-0086-0 Natural hydroxyanthraquinoid pigments as potent food grade colorants: an overview a,b, a,b a,b b,c b,c Yanis CARO, * Linda ANAMALE, Mireille FOUILLAUD, Philippe LAURENT, Thomas PETIT, and a,b Laurent DUFOSSE aDépartement Agroalimentaire, ESIROI, Université de La Réunion, Sainte-Clotilde, Ile de la Réunion, France b LCSNSA, Faculté des Sciences et des Technologies, Université de La Réunion, Sainte-Clotilde, Ile de la Réunion, France c Département Génie Biologique, IUT, Université de La Réunion, Saint-Pierre, Ile de la Réunion, France Received 24 October 2012; Accepted 12 November 2012 © The Author(s) 2012. This article is published with open access at Springerlink.com Abstract: Natural pigments and colorants are widely used in the world in many industries such as textile dying, food processing or cosmetic manufacturing. Among the natural products of interest are various compounds belonging to carotenoids, anthocyanins, chlorophylls, melanins, betalains… The review emphasizes pigments with anthraquinoid skeleton and gives an overview on hydroxyanthraquinoids described in Nature, the first one ever published. Trends in consumption, production and regulation of natural food grade colorants are given, in the current global market. The second part focuses on the description of the chemical structures of the main anthraquinoid colouring compounds, their properties and their biosynthetic pathways. Main natural sources of such pigments are summarized, followed by discussion about toxicity and carcinogenicity observed in some cases. As a conclusion, current industrial applications of natural hydroxyanthraquinoids are described with two examples, carminic acid from an insect and Arpink red™ from a filamentous fungus. -

(12) United States Patent (10) Patent No.: US 9,687,864 B2 Fulton Et Al
USOO9687864B2 (12) United States Patent (10) Patent No.: US 9,687,864 B2 Fulton et al. (45) Date of Patent: Jun. 27, 2017 (54) SYSTEMAND METHOD FOR ENHANCED 428/25 (2015.01); Y10T 428/31504 (2015.04); ELECTROSTATIC DEPOSITION AND Y10T 428/31507 (2015.04); SURFACE COATINGS (Continued) (58) Field of Classification Search (71) Applicant: Battelle Memorial Institute, USPC .......... 118/620–640; 23.9/690 708; 427/458, Columbus, OH (US) 427/475 4.86 (72) Inventors: John L. Fulton, Richland, WA (US); See application file for complete search history. George S. Deverman, Richland, WA (US); Dean W. Matson, Kennewick, (56) References Cited CA (US); Clement R. Yonker, Kennewick, WA (US); C. Douglas U.S. PATENT DOCUMENTS Taylor, Franklinton, NC (US); James 3,087,860 A 4, 1963 Endicott B. McClain, Raleigh, NC (US); Joseph 3,123,077 A 3, 1964 Alcamo M. Crowley, Cambria, CA (US) (Continued) (73) Assignee: Battelle Memorial Institute, Columbus, OH (US) FOREIGN PATENT DOCUMENTS CA 2589761 12, 2004 (*) Notice: Subject to any disclaimer, the term of this CN 1465410 1, 2004 patent is extended or adjusted under 35 (Continued) U.S.C. 154(b) by 0 days. (21) Appl. No.: 14/310,960 OTHER PUBLICATIONS Abreu Filho et al., “Influence of metal alloy and the profile of (22) Filed: Jun. 20, 2014 coronary stents in patients with multi-vessel coronary disease.” Clinics 66(6):985-989 (2011). (65) Prior Publication Data (Continued) US 2015/OO40827 A1 Feb. 12, 2015 Related U.S. Application Data Primary Examiner — Yewebdar Tadesse (74) Attorney, Agent, or Firm — Lerner, David, (62) Division of application No.