Atlas Journal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Analysis of Gene Expression Data for Gene Ontology
ANALYSIS OF GENE EXPRESSION DATA FOR GENE ONTOLOGY BASED PROTEIN FUNCTION PREDICTION A Thesis Presented to The Graduate Faculty of The University of Akron In Partial Fulfillment of the Requirements for the Degree Master of Science Robert Daniel Macholan May 2011 ANALYSIS OF GENE EXPRESSION DATA FOR GENE ONTOLOGY BASED PROTEIN FUNCTION PREDICTION Robert Daniel Macholan Thesis Approved: Accepted: _______________________________ _______________________________ Advisor Department Chair Dr. Zhong-Hui Duan Dr. Chien-Chung Chan _______________________________ _______________________________ Committee Member Dean of the College Dr. Chien-Chung Chan Dr. Chand K. Midha _______________________________ _______________________________ Committee Member Dean of the Graduate School Dr. Yingcai Xiao Dr. George R. Newkome _______________________________ Date ii ABSTRACT A tremendous increase in genomic data has encouraged biologists to turn to bioinformatics in order to assist in its interpretation and processing. One of the present challenges that need to be overcome in order to understand this data more completely is the development of a reliable method to accurately predict the function of a protein from its genomic information. This study focuses on developing an effective algorithm for protein function prediction. The algorithm is based on proteins that have similar expression patterns. The similarity of the expression data is determined using a novel measure, the slope matrix. The slope matrix introduces a normalized method for the comparison of expression levels throughout a proteome. The algorithm is tested using real microarray gene expression data. Their functions are characterized using gene ontology annotations. The results of the case study indicate the protein function prediction algorithm developed is comparable to the prediction algorithms that are based on the annotations of homologous proteins. -

Mitochondrial Membrane Binding and Protein Complexing of the Anti-Apoptotic Adaptor Protein Grblo
Mitochondrial membrane binding and protein complexing of the anti-apoptotic adaptor protein GrblO. by Jennifer Hassard Department of Biology McGill University, Montreal A thesis submitted to the Faculty of Graduate Studies and Research in partial fulfillment of the requirements for the degree of Master's of Science August 2001 Supervisor: Dr. David Thomas, Department of Biochemistry © Jennifer Hassard, 2001 .....--. National Library Bibliothèque nationale 1+1 of Canada du Canada Acquisitions and Acquisitions et Bibliographie Services services bibliographiques 395 Wellington Street 395. rue Wellington OttawaON K1A0N4 Ottawa ON K1 A ON4 canada canada Your liIe VoIJ8 rrlfénJnce Our liIe Notre rtifénlncs The author has granted a non L'auteur a accordé une licence non exclusive licence al10wing the exclusive permettant à la National Library ofCanada to Bibliothèque nationale du Canada de reproduce, loan, distribute or sell reproduire, prêter, distribuer ou copies ofthis thesis in microform, vendre des copies de cette thèse sous paper or electronic formats. la forme de microfiche/film, de reproduction sur papier ou sur format électronique. The author retains ownership ofthe L'auteur conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substantial extracts from it Ni la thèse ni des extraits substantiels may be printed or otherwise de celle-ci ne doivent être imprimés reproduced without the autbor's ou autrement reproduits sans son penmsslon. autorisation. 0-612-78889-X Canada ABSTRACT GrblO is a member of the Grb7 family of adaptor proteins that also includes Grb7 and Grb14. These three members contain multiple protein binding domains and lack enzymatic activity. -

Transcriptional Regulation of RKIP in Prostate Cancer Progression
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Sciences Transcriptional Regulation of RKIP in Prostate Cancer Progression Submitted by: Sandra Marie Beach In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Sciences Examination Committee Major Advisor: Kam Yeung, Ph.D. Academic William Maltese, Ph.D. Advisory Committee: Sonia Najjar, Ph.D. Han-Fei Ding, M.D., Ph.D. Manohar Ratnam, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: May 16, 2007 Transcriptional Regulation of RKIP in Prostate Cancer Progression Sandra Beach University of Toledo ACKNOWLDEGMENTS I thank my major advisor, Dr. Kam Yeung, for the opportunity to pursue my degree in his laboratory. I am also indebted to my advisory committee members past and present, Drs. Sonia Najjar, Han-Fei Ding, Manohar Ratnam, James Trempe, and Douglas Pittman for generously and judiciously guiding my studies and sharing reagents and equipment. I owe extended thanks to Dr. William Maltese as a committee member and chairman of my department for supporting my degree progress. The entire Department of Biochemistry and Cancer Biology has been most kind and helpful to me. Drs. Roy Collaco and Hong-Juan Cui have shared their excellent technical and practical advice with me throughout my studies. I thank members of the Yeung laboratory, Dr. Sungdae Park, Hui Hui Tang, Miranda Yeung for their support and collegiality. The data mining studies herein would not have been possible without the helpful advice of Dr. Robert Trumbly. I am also grateful for the exceptional assistance and shared microarray data of Dr. -

Molecular Classification Reveals the Diverse Genetic Features and Prognosis
bioRxiv preprint doi: https://doi.org/10.1101/2021.06.07.447364; this version posted June 7, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Molecular classification reveals the diverse genetic features and prognosis of gastric cancer: a multi-omics consensus ensemble clustering 1 Xianyu Hu1#, Zhenglin Wang1#, Qing Wang2#, Ke Chen1, Qijun Han1, Suwen Bai3, 2 Juan Du3,4*, Wei Chen1* 3 1 Department of General Surgery, The First Affiliated Hospital of Anhui Medical 4 University Hefei, Anhui Province 230022, P.R. China 5 2 Department of Biliary-Pancreatic Minimally Invasive Surgery, The First Affiliated 6 Hospital of Shantou University Medical College, Shantou, Guangdong Province 515000, 7 P.R. China 8 3 Longgang District People’s Hospital of Shenzhen & The Third Affiliated Hospital 9 (Provisional) of The Chinese University of Hong Kong, Shenzhen, Shenzhen, 10 Guangdong Province 518172, P.R. China 11 4 School of Medicine, The Chinese University of Hong Kong, Shenzhen, Shenzhen, 12 Guangdong Province 518172, P.R. China 13 14 # These authors contributed equally to the study. 15 Correspondence should be addressed to Wei Chen ([email protected]) 16 17 18 bioRxiv preprint doi: https://doi.org/10.1101/2021.06.07.447364; this version posted June 7, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 19 *Correspondence to: 20 Prof. Juan Du 21 Longgang District People’s Hospital of Shenzhen & The Third Affiliated Hospital 22 (Provisional) of The Chinese University of Hong Kong, Shenzhen, Shenzhen, 23 Guangdong Province 518172, P.R. -

Trajectory and Uniqueness of Mutational Signatures in Yeast Mutators
Trajectory and uniqueness of mutational signatures in yeast mutators Sophie Loeilleta,b, Mareike Herzogc, Fabio Pudduc, Patricia Legoixd, Sylvain Baulanded, Stephen P. Jacksonc, and Alain G. Nicolasa,b,1 aInstitut Curie, Paris Sciences et Lettres Research University, CNRS, UMR3244, 75248 Paris Cedex 05, France; bSorbonne Universités, Université Pierre et Marie Curie Paris 06, CNRS, UMR3244, 75248 Paris Cedex 05, France; cWellcome/Cancer Research UK Gurdon Institute and Department of Biochemistry, Cambridge CB2 1QN, United Kingdom; and dICGex NGS Platform, Institut Curie, 75248 Paris Cedex 05, France Edited by Richard D. Kolodner, Ludwig Institute for Cancer Research, La Jolla, CA, and approved August 24, 2020 (received for review June 2, 2020) The acquisition of mutations plays critical roles in adaptation, evolution, known (5, 15, 16). Here, we conducted a reciprocal functional ap- senescence, and tumorigenesis. Massive genome sequencing has proach to inactivate one or several genes involved in distinct ge- allowed extraction of specific features of many mutational landscapes nome maintenance processes (replication, repair, recombination, but it remains difficult to retrospectively determine the mechanistic oxidative stress response, or cell-cycle progression) in Saccharomy- origin(s), selective forces, and trajectories of transient or persistent ces cerevisiae diploids, establish the genome-wide mutational land- mutations and genome rearrangements. Here, we conducted a pro- scapes of mutation accumulation (MA) lines, explore the underlying spective reciprocal approach to inactivate 13 single or multiple evolu- mechanisms, and characterize the dynamics of mutation accumu- tionary conserved genes involved in distinct genome maintenance lation (and disappearance) along single-cell bottleneck passages. processes and characterize de novo mutations in 274 diploid Saccharo- myces cerevisiae mutation accumulation lines. -

3256.Full.Pdf
Negative epistasis between natural variants of the Saccharomyces cerevisiae MLH1 and PMS1 genes results in a defect in mismatch repair Julie Akiko Heck, Juan Lucas Argueso, Zekeriyya Gemici, Richard Guy Reeves*, Ann Bernard, Charles F. Aquadro, and Eric Alani† Department of Molecular Biology and Genetics, Cornell University, Ithaca, NY 14853 Communicated by Thomas D. Petes, University of North Carolina, Chapel Hill, NC, December 20, 2005 (received for review June 22, 2005) In budding yeast, the MLH1-PMS1 heterodimer is the major MutL The influences of epistatic interactions on a wide variety of homolog complex that acts to repair mismatches arising during traits and processes have garnered increasing attention (14–17). DNA replication. Using a highly sensitive mutator assay, we ob- Few examples, however, have been characterized in molecular served that Saccharomyces cerevisiae strains bearing the S288c- detail. Here we show that the strain-dependent MMR pheno- strain-derived MLH1 gene and the SK1-strain-derived PMS1 gene types observed previously for site-specific mlh1 mutants were displayed elevated mutation rates that conferred a long-term due in part to an underlying defect between wild-type MMR fitness cost. Dissection of this negative epistatic interaction using genes from S288c and SK1. We identified the specific amino acid S288c-SK1 chimeras revealed that a single amino acid polymor- polymorphisms in MLH1 and PMS1, whose combined effect in phism in each gene accounts for this mismatch repair defect. Were hybrid strains leads to an elevation in mutation rate and a these strains to cross in natural populations, segregation of alleles generalized reduction in long-term fitness. -
Androgen Receptor Interacting Proteins and Coregulators Table
ANDROGEN RECEPTOR INTERACTING PROTEINS AND COREGULATORS TABLE Compiled by: Lenore K. Beitel, Ph.D. Lady Davis Institute for Medical Research 3755 Cote Ste Catherine Rd, Montreal, Quebec H3T 1E2 Canada Telephone: 514-340-8260 Fax: 514-340-7502 E-Mail: [email protected] Internet: http://androgendb.mcgill.ca Date of this version: 2010-08-03 (includes articles published as of 2009-12-31) Table Legend: Gene: Official symbol with hyperlink to NCBI Entrez Gene entry Protein: Protein name Preferred Name: NCBI Entrez Gene preferred name and alternate names Function: General protein function, categorized as in Heemers HV and Tindall DJ. Endocrine Reviews 28: 778-808, 2007. Coregulator: CoA, coactivator; coR, corepressor; -, not reported/no effect Interactn: Type of interaction. Direct, interacts directly with androgen receptor (AR); indirect, indirect interaction; -, not reported Domain: Interacts with specified AR domain. FL-AR, full-length AR; NTD, N-terminal domain; DBD, DNA-binding domain; h, hinge; LBD, ligand-binding domain; C-term, C-terminal; -, not reported References: Selected references with hyperlink to PubMed abstract. Note: Due to space limitations, all references for each AR-interacting protein/coregulator could not be cited. The reader is advised to consult PubMed for additional references. Also known as: Alternate gene names Gene Protein Preferred Name Function Coregulator Interactn Domain References Also known as AATF AATF/Che-1 apoptosis cell cycle coA direct FL-AR Leister P et al. Signal Transduction 3:17-25, 2003 DED; CHE1; antagonizing regulator Burgdorf S et al. J Biol Chem 279:17524-17534, 2004 CHE-1; AATF transcription factor ACTB actin, beta actin, cytoplasmic 1; cytoskeletal coA - - Ting HJ et al. -

De Novo, Systemic, Deleterious Amino Acid Substitutions Are Common in Large Cytoskeleton‑Related Protein Coding Regions
BIOMEDICAL REPORTS 6: 211-216, 2017 De novo, systemic, deleterious amino acid substitutions are common in large cytoskeleton‑related protein coding regions REBECCA J. STOLL1, GRACE R. THOMPSON1, MOHAMMAD D. SAMY1 and GEORGE BLANCK1,2 1Department of Molecular Medicine, Morsani College of Medicine, University of South Florida; 2Immunology Program, H. Lee Moffitt Cancer Center and Research Institute, Tampa, FL 33612, USA Received June 13, 2016; Accepted October 31, 2016 DOI: 10.3892/br.2016.826 Abstract. Human mutagenesis is largely random, thus large Introduction coding regions, simply on the basis of probability, represent relatively large mutagenesis targets. Thus, we considered Genetic damage is largely random and therefore tends to the possibility that large cytoskeletal-protein related coding affect the larger, functional regions of the human genome regions (CPCRs), including extra-cellular matrix (ECM) more frequently than the smaller regions (1). For example, coding regions, would have systemic nucleotide variants that a systematic study has revealed that cancer fusion genes, on are not present in common SNP databases. Presumably, such average, are statistically, significantly larger than other human variants arose recently in development or in recent, preceding genes (2,3). The large introns of potential cancer fusion genes generations. Using matched breast cancer and blood-derived presumably allow for many different productive recombina- normal datasets from the cancer genome atlas, CPCR single tion opportunities, i.e., many recombinations that would allow nucleotide variants (SNVs) not present in the All SNPs(142) for exon juxtaposition and the generation of hybrid proteins. or 1000 Genomes databases were identified. Using the Protein Smaller cancer fusion genes tend to be associated with the rare Variation Effect Analyzer internet-based tool, it was discov- types of cancer, for example EWS RNA binding protein 1 in ered that apparent, systemic mutations (not shared among Ewing's sarcoma. -
Primepcr™Assay Validation Report
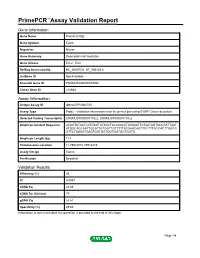
PrimePCR™Assay Validation Report Gene Information Gene Name Protein EVI2B Gene Symbol Evi2b Organism Mouse Gene Summary Description Not Available Gene Aliases Evi-2, Evi2 RefSeq Accession No. NC_000077.6, NT_096135.6 UniGene ID Not Available Ensembl Gene ID ENSMUSG00000093938 Entrez Gene ID 216984 Assay Information Unique Assay ID qMmuCEP0062720 Assay Type Probe - Validation information is for the primer pair using SYBR® Green detection Detected Coding Transcript(s) ENSMUST00000179322, ENSMUST00000170422 Amplicon Context Sequence ACAGTATAATCATGAGTATAGCTACCAACATAGAAATTATAATAGTACCGATTAAT ATGGCAGCAATTGCATTGTGGTTGTTTTTATGAGCAGTTCCTTTGCCACTTGGTG GTTCTGAAGTGAGTGGTGGTGGTGGTGGTGGTG Amplicon Length (bp) 114 Chromosome Location 11:79516072-79516215 Assay Design Exonic Purification Desalted Validation Results Efficiency (%) 95 R2 0.9997 cDNA Cq 22.69 cDNA Tm (Celsius) 79 gDNA Cq 24.61 Specificity (%) 49.93 Information to assist with data interpretation is provided at the end of this report. Page 1/4 PrimePCR™Assay Validation Report Evi2b, Mouse Amplification Plot Amplification of cDNA generated from 25 ng of universal reference RNA Melt Peak Melt curve analysis of above amplification Standard Curve Standard curve generated using 20 million copies of template diluted 10-fold to 20 copies Page 2/4 PrimePCR™Assay Validation Report Products used to generate validation data Real-Time PCR Instrument CFX384 Real-Time PCR Detection System Reverse Transcription Reagent iScript™ Advanced cDNA Synthesis Kit for RT-qPCR Real-Time PCR Supermix SsoAdvanced™ SYBR® Green Supermix Experimental Sample qPCR Mouse Reference Total RNA Data Interpretation Unique Assay ID This is a unique identifier that can be used to identify the assay in the literature and online. Detected Coding Transcript(s) This is a list of the Ensembl transcript ID(s) that this assay will detect. -

RCHY1 Antibody
Efficient Professional Protein and Antibody Platforms RCHY1 Antibody Basic information: Catalog No.: UMA60398 Source: Mouse Size: 50ul/100ul Clonality: Monoclonal Concentration: 1mg/ml Isotype: Mouse IgG1 Purification: Protein A affinity purified Useful Information: WB:1:500-1:1000 ICC:1:50-1:200 Applications: IHC:1:50-1:200 FC:1:100-1:200 Reactivity: Human, Rat Specificity: This antibody recognizes RCHY1 protein. Immunogen: Recombinant protein Pirh2, also known as Androgen receptor N-terminal-interacting protein (ARNIP), ZN363 or CHIMP, has p53-induced ubiquitin-protein ligase activity, promoting p53 degradation. The protein physically interacts with p53 and the resulting degradation of p53 renders Pirh2 an oncogenic protein as the loss of p53 function contributes to malignant tumor development. The gene Description: encoding for the protein maps to chromosome 4q21.1 and transcription of this gene is regulated by p53. Pirh2 expression decreases the level of p53 and a decrease of endogenous Pirh2 expression ups p53 levels. Pirh2 is therefore considered, together with MDM2, to be acting as a negative reg- ulator of p53 function. Uniprot: Q96PM5(Human) BiowMW: 30 kDa Buffer: 1*TBS (pH7.4), 1%BSA, 40%Glycerol. Preservative: 0.05% Sodium Azide. Storage: Store at 4°C short term and -20°C long term. Avoid freeze-thaw cycles. Note: For research use only, not for use in diagnostic procedure. Data: Western blot analysis of Pirh2 on different cell lysate using anti-Pirh2 antibody at 1/1,000 dilu- tion. Positive control: Line1: HelaLine2: A549 Line3: MCF-7 Line4: PC-12 Gene Universal Technology Co. Ltd www.universalbiol.com Tel: 0550-3121009 E-mail: [email protected] Efficient Professional Protein and Antibody Platforms ICC staining Pirh2 (green) and Actin filaments (red) in Hela cells. -

CALIFORNIA STATE UNIVERSITY, NORTHRIDGE Bioinformatic
CALIFORNIA STATE UNIVERSITY, NORTHRIDGE Bioinformatic Comparison of the EVI2A Promoter and Coding Regions A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science in Biology By Max Weinstein May 2020 The thesis of Max Weinstein is approved: Professor Rheem D. Medh Date Professor Virginia Oberholzer Vandergon Date Professor Cindy Malone, Chair Date California State University Northridge ii Table of Contents Signature Page ii List of Figures v Abstract vi Introduction 1 Ecotropic Viral Integration Site 2A, a Gene within a Gene 7 Materials and Methods 11 PCR and Cloning of Recombinant Plasmid 11 Transformation and Cell Culture 13 Generation of Deletion Constructs 15 Transfection and Luciferase Assay 16 Identification of Transcription Factor Binding Sites 17 Determination of Region for Analysis 17 Multiple Sequence Alignment (MSA) 17 Model Testing 18 Tree Construction 18 Promoter and CDS Conserved Motif Search 19 Results and Discussion 20 Choice of Species for Analysis 20 Mapping of Potential Transcription Factor Binding Sites 20 Confirmation of Plasmid Generation through Gel Electrophoresis 21 Analysis of Deletion Constructs by Transient Transfection 22 EVI2A Coding DNA Sequence Phylogenetics 23 EVI2A Promoter Phylogenetics 23 EVI2A Conserved Leucine Zipper 25 iii EVI2A Conserved Casein kinase II phosphorylation site 26 EVI2A Conserved Sox-5 Binding Site 26 EVI2A Conserved HLF Binding Site 27 EVI2A Conserved cREL Binding Site 28 EVI2A Conserved CREB Binding Site 28 Summary 29 Appendix: Figures 30 Literature Cited 44 iv List of Figures Figure 1. EVI2A is nested within the gene NF1 30 Figure 2 Putative Transcriptions Start Site 31 Figure 3. Gel Electrophoresis of pGC Blue cloned, Restriction Digested Plasmid 32 Figure 4. -

RNA-Seq Transcriptome Analysis Of
on: Sequ ati en er c Le Luyer et al, Next Generat Sequenc & Applic 2015, 2:1 n in e g G & t x A DOI: 10.4172/2469-9853.1000112 e p Journal of p N l f i c o a l t a i o n r ISSN: 2469-9853n u s o J Next Generation Sequencing & Applications Research Article Open Access RNA-Seq Transcriptome Analysis of Pronounced Biconcave Vertebrae: A Common Abnormality in Rainbow Trout (Oncorhynchus mykiss, Walbaum) Fed a Low-Phosphorus Diet Le Luyer J1, Deschamps MH1, Proulx E1, Poirier Stewart N1, Droit A2, Sire JY3, Robert C1 and Vandenberg GW1* 1Département of des sciences animales, Pavillon Paul-Comtois, Université Laval, Québec, QC, Canada G1V 0A6, Canada 2Department of Molecular Medicine, Centre de Recherche du CHU de Québec, Université Laval, Québec, QC, G1V 4G2 Canada 3Institut de Biologie Paris-Seine, UMR 7138-Evolution Paris-Seine, Université Pierre et Marie Curie, Paris, France Abstract The prevalence of bone deformities, particularly linked with mineral deficiency, is an important issue for fish production. Juvenile triploid rainbow trout (Oncorhynchus mykiss) were fed a low-phosphorus (P) diet for 27 weeks (60 to 630 g body mass). At study termination, 24.9% of the fish fed the low-P diet displayed homogeneous biconcave vertebrae (deformed vertebrae phenotype), while 5.5% displayed normal vertebral phenotypes for the entire experiment. The aim of our study was to characterize the deformed phenotype and identify the putative genes involved in the appearance of P deficiency-induced deformities. Both P status and biomechanical measurements showed that deformed vertebrae were significantly less mineralized (55.0 ± 0.4 and 59.4 ± 0.5,% ash DM, for deformed and normal vertebrae, respectively) resulting in a lower stiffness (80.3 ± 9.0 and 140.2 ± 6.3 N/mm, for deformed and normal phenotypes, respectively).