Update on Australian Rickettsial Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Evidence of Novel Spotted Fever Group Rickettsia
pathogens Article Molecular Evidence of Novel Spotted Fever Group Rickettsia Species in Amblyomma albolimbatum Ticks from the Shingleback Skink (Tiliqua rugosa) in Southern Western Australia Mythili Tadepalli 1, Gemma Vincent 1, Sze Fui Hii 1, Simon Watharow 2, Stephen Graves 1,3 and John Stenos 1,* 1 Australian Rickettsial Reference Laboratory, University Hospital Geelong, Geelong 3220, Australia; [email protected] (M.T.); [email protected] (G.V.); [email protected] (S.F.H.); [email protected] (S.G.) 2 Reptile Victoria Inc., Melbourne 3035, Australia; [email protected] 3 Department of Microbiology and Infectious Diseases, Nepean Hospital, NSW Health Pathology, Penrith 2747, Australia * Correspondence: [email protected] Abstract: Tick-borne infectious diseases caused by obligate intracellular bacteria of the genus Rick- ettsia are a growing global problem to human and animal health. Surveillance of these pathogens at the wildlife interface is critical to informing public health strategies to limit their impact. In Australia, reptile-associated ticks such as Bothriocroton hydrosauri are the reservoirs for Rickettsia honei, the causative agent of Flinders Island spotted fever. In an effort to gain further insight into the potential for reptile-associated ticks to act as reservoirs for rickettsial infection, Rickettsia-specific PCR screening was performed on 64 Ambylomma albolimbatum ticks taken from shingleback skinks (Tiliqua rugosa) lo- cated in southern Western Australia. PCR screening revealed 92% positivity for rickettsial DNA. PCR Citation: Tadepalli, M.; Vincent, G.; amplification and sequencing of phylogenetically informative rickettsial genes (ompA, ompB, gltA, Hii, S.F.; Watharow, S.; Graves, S.; Stenos, J. -
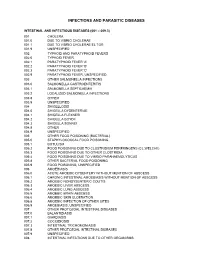
Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

CD Alert Monthly Newsletter of National Centre for Disease Control, Directorate General of Health Services, Government of India
CD Alert Monthly Newsletter of National Centre for Disease Control, Directorate General of Health Services, Government of India May - July 2009 Vol. 13 : No. 1 SCRUB TYPHUS & OTHER RICKETTSIOSES it lacks lipopolysaccharide and peptidoglycan RICKETTSIAL DISEASES and does not have an outer slime layer. It is These are the diseases caused by rickettsiae endowed with a major surface protein (56kDa) which are small, gram negative bacilli adapted and some minor surface protein (110, 80, 46, to obligate intracellular parasitism, and 43, 39, 35, 25 and 25kDa). There are transmitted by arthropod vectors. These considerable differences in virulence and organisms are primarily parasites of arthropods antigen composition among individual strains such as lice, fleas, ticks and mites, in which of O.tsutsugamushi. O.tsutsugamushi has they are found in the alimentary canal. In many serotypes (Karp, Gillian, Kato and vertebrates, including humans, they infect the Kawazaki). vascular endothelium and reticuloendothelial GLOBAL SCENARIO cells. Commonly known rickettsial disease is Scrub Typhus. Geographic distribution of the disease occurs within an area of about 13 million km2 including- The family Rickettsiaeceae currently comprises Afghanistan and Pakistan to the west; Russia of three genera – Rickettsia, Orientia and to the north; Korea and Japan to the northeast; Ehrlichia which appear to have descended Indonesia, Papua New Guinea, and northern from a common ancestor. Former members Australia to the south; and some smaller of the family, Coxiella burnetii, which causes islands in the western Pacific. It was Q fever and Rochalimaea quintana causing first observed in Japan where it was found to trench fever have been excluded because the be transmitted by mites. -

Ohio Department of Health, Bureau of Infectious Diseases Disease Name Class A, Requires Immediate Phone Call to Local Health
Ohio Department of Health, Bureau of Infectious Diseases Reporting specifics for select diseases reportable by ELR Class A, requires immediate phone Susceptibilities specimen type Reportable test name (can change if Disease Name other specifics+ call to local health required* specifics~ state/federal case definition or department reporting requirements change) Culture independent diagnostic tests' (CIDT), like BioFire panel or BD MAX, E. histolytica Stain specimen = stool, bile results should be sent as E. histolytica DNA fluid, duodenal fluid, 260373001^DETECTED^SCT with E. histolytica Antigen Amebiasis (Entamoeba histolytica) No No tissue large intestine, disease/organism-specific DNA LOINC E. histolytica Antibody tissue small intestine codes OR a generic CIDT-LOINC code E. histolytica IgM with organism-specific DNA SNOMED E. histolytica IgG codes E. histolytica Total Antibody Ova and Parasite Anthrax Antibody Anthrax Antigen Anthrax EITB Acute Anthrax EITB Convalescent Anthrax Yes No Culture ELISA PCR Stain/microscopy Stain/spore ID Eastern Equine Encephalitis virus Antibody Eastern Equine Encephalitis virus IgG Antibody Eastern Equine Encephalitis virus IgM Arboviral neuroinvasive and non- Eastern Equine Encephalitis virus RNA neuroinvasive disease: Eastern equine California serogroup virus Antibody encephalitis virus disease; LaCrosse Equivocal results are accepted for all California serogroup virus IgG Antibody virus disease (other California arborviral diseases; California serogroup virus IgM Antibody specimen = blood, serum, serogroup -

Mechanisms of Rickettsia Parkeri Invasion of Host Cells and Early Actin-Based Motility
Mechanisms of Rickettsia parkeri invasion of host cells and early actin-based motility By Shawna Reed A dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Philosophy in Microbiology in the Graduate Division of the University of California, Berkeley Committee in charge: Professor Matthew D. Welch, Chair Professor David G. Drubin Professor Daniel Portnoy Professor Kathleen R. Ryan Fall 2012 Mechanisms of Rickettsia parkeri invasion of host cells and early actin-based motility © 2012 By Shawna Reed ABSTRACT Mechanisms of Rickettsia parkeri invasion of host cells and early actin-based motility by Shawna Reed Doctor of Philosophy in Microbiology University of California, Berkeley Professor Matthew D. Welch, Chair Rickettsiae are obligate intracellular pathogens that are transmitted to humans by arthropod vectors and cause diseases such as spotted fever and typhus. Spotted fever group (SFG) Rickettsia hijack the host actin cytoskeleton to invade, move within, and spread between eukaryotic host cells during their obligate intracellular life cycle. Rickettsia express two bacterial proteins that can activate actin polymerization: RickA activates the host actin-nucleating Arp2/3 complex while Sca2 directly nucleates actin filaments. In this thesis, I aimed to resolve which host proteins were required for invasion and intracellular motility, and to determine how the bacterial proteins RickA and Sca2 contribute to these processes. Although rickettsiae require the host cell actin cytoskeleton for invasion, the cytoskeletal proteins that mediate this process have not been completely described. To identify the host factors important during cell invasion by Rickettsia parkeri, a member of the SFG, I performed an RNAi screen targeting 105 proteins in Drosophila melanogaster S2R+ cells. -

Expansion of Tick-Borne Rickettsioses in the World
microorganisms Review Expansion of Tick-Borne Rickettsioses in the World Mariusz Piotrowski * and Anna Rymaszewska Institute of Biology, University of Szczecin, 70-453 Szczecin, Poland; [email protected] * Correspondence: [email protected] Received: 24 September 2020; Accepted: 25 November 2020; Published: 30 November 2020 Abstract: Tick-borne rickettsioses are caused by obligate intracellular bacteria belonging to the spotted fever group of the genus Rickettsia. These infections are among the oldest known diseases transmitted by vectors. In the last three decades there has been a rapid increase in the recognition of this disease complex. This unusual expansion of information was mainly caused by the development of molecular diagnostic techniques that have facilitated the identification of new and previously recognized rickettsiae. A lot of currently known bacteria of the genus Rickettsia have been considered nonpathogenic for years, and moreover, many new species have been identified with unknown pathogenicity. The genus Rickettsia is distributed all over the world. Many Rickettsia species are present on several continents. The geographical distribution of rickettsiae is related to their vectors. New cases of rickettsioses and new locations, where the presence of these bacteria is recognized, are still being identified. The variety and rapid evolution of the distribution and density of ticks and diseases which they transmit shows us the scale of the problem. This review article presents a comparison of the current understanding of the geographic distribution of pathogenic Rickettsia species to that of the beginning of the century. Keywords: Tick-borne rickettsioses; Tick-borne diseases; Rickettsiales 1. Introduction Tick-borne rickettsioses are caused by obligate intracellular Gram-negative bacteria belonging to the spotted fever group (SFG) of the genus Rickettsia. -

Scrub Typhus and Molecular Characterization of Orientia Tsutsugamushi from Central Nepal
pathogens Article Scrub Typhus and Molecular Characterization of Orientia tsutsugamushi from Central Nepal Rajendra Gautam 1, Keshab Parajuli 1, Mythili Tadepalli 2, Stephen Graves 2, John Stenos 2,* and Jeevan Bahadur Sherchand 1 1 Department of Microbiology, Maharajgunj Medical Campus, Institute of Medicine, Kathmandu 44600, Nepal; [email protected] (R.G.); [email protected] (K.P.); [email protected] (J.B.S.) 2 Australian Rickettsial Reference Laboratory, Geelong, VIC 3220, Australia; [email protected] (M.T.); [email protected] (S.G.) * Correspondence: [email protected]; Tel.: +61-342151357 Abstract: Scrub typhus is a vector-borne, acute febrile illness caused by Orientia tsutsugamushi. Scrub typhus continues to be an important but neglected tropical disease in Nepal. Information on this pathogen in Nepal is limited to serological surveys with little information available on molecular methods to detect O. tsutsugamushi. Limited information exists on the genetic diversity of this pathogen. A total of 282 blood samples were obtained from patients with suspected scrub typhus from central Nepal and 84 (30%) were positive for O. tsutsugamushi by 16S rRNA qPCR. Positive samples were further subjected to 56 kDa and 47 kDa molecular typing and molecularly compared to other O. tsutsugamushi strains. Phylogenetic analysis revealed that Nepalese O. tsutsugamushi strains largely cluster together and cluster away from other O. tsutsugamushi strains from Asia and elsewhere. One exception was the sample of Nepal_1, with its partial 56 kDa sequence clustering Citation: Gautam, R.; Parajuli, K.; more closely with non-Nepalese O. tsutsugamushi 56 kDa sequences, potentially indicating that Tadepalli, M.; Graves, S.; Stenos, J.; homologous recombination may influence the genetic diversity of strains in this region. -

Typhus Fever, Organism Inapparently
Rickettsia Importance Rickettsia prowazekii is a prokaryotic organism that is primarily maintained in prowazekii human populations, and spreads between people via human body lice. Infected people develop an acute, mild to severe illness that is sometimes complicated by neurological Infections signs, shock, gangrene of the fingers and toes, and other serious signs. Approximately 10-30% of untreated clinical cases are fatal, with even higher mortality rates in Epidemic typhus, debilitated populations and the elderly. People who recover can continue to harbor the Typhus fever, organism inapparently. It may re-emerge years later and cause a similar, though Louse–borne typhus fever, generally milder, illness called Brill-Zinsser disease. At one time, R. prowazekii Typhus exanthematicus, regularly caused extensive outbreaks, killing thousands or even millions of people. This gave rise to the most common name for the disease, epidemic typhus. Epidemic typhus Classical typhus fever, no longer occurs in developed countries, except as a sporadic illness in people who Sylvatic typhus, have acquired it while traveling, or who have carried the organism for years without European typhus, clinical signs. In North America, R. prowazekii is also maintained in southern flying Brill–Zinsser disease, Jail fever squirrels (Glaucomys volans), resulting in sporadic zoonotic cases. However, serious outbreaks still occur in some resource-poor countries, especially where people are in close contact under conditions of poor hygiene. Epidemics have the potential to emerge anywhere social conditions disintegrate and human body lice spread unchecked. Last Updated: February 2017 Etiology Rickettsia prowazekii is a pleomorphic, obligate intracellular, Gram negative coccobacillus in the family Rickettsiaceae and order Rickettsiales of the α- Proteobacteria. -

Leptospirosis and Coinfection: Should We Be Concerned?
International Journal of Environmental Research and Public Health Review Leptospirosis and Coinfection: Should We Be Concerned? Asmalia Md-Lasim 1,2, Farah Shafawati Mohd-Taib 1,* , Mardani Abdul-Halim 3 , Ahmad Mohiddin Mohd-Ngesom 4 , Sheila Nathan 1 and Shukor Md-Nor 1 1 Department of Biological Sciences and Biotechnology, Faculty of Science and Technology, Universiti Kebangsaan Malaysia, UKM, Bangi 43600, Selangor, Malaysia; [email protected] (A.M.-L.); [email protected] (S.N.); [email protected] (S.M.-N.) 2 Herbal Medicine Research Centre (HMRC), Institute for Medical Research (IMR), National Institue of Health (NIH), Ministry of Health, Shah Alam 40170, Selangor, Malaysia 3 Biotechnology Research Institute, Universiti Malaysia Sabah, Jalan UMS, Kota Kinabalu 88400, Sabah, Malaysia; [email protected] 4 Center for Toxicology and Health Risk, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur 50300, Federal Territory of Kuala Lumpur, Malaysia; [email protected] * Correspondence: [email protected]; Tel.: +60-12-3807701 Abstract: Pathogenic Leptospira is the causative agent of leptospirosis, an emerging zoonotic disease affecting animals and humans worldwide. The risk of host infection following interaction with environmental sources depends on the ability of Leptospira to persist, survive, and infect the new host to continue the transmission chain. Leptospira may coexist with other pathogens, thus providing a suitable condition for the development of other pathogens, resulting in multi-pathogen infection in humans. Therefore, it is important to better understand the dynamics of transmission by these pathogens. We conducted Boolean searches of several databases, including Google Scholar, PubMed, Citation: Md-Lasim, A.; Mohd-Taib, SciELO, and ScienceDirect, to identify relevant published data on Leptospira and coinfection with F.S.; Abdul-Halim, M.; Mohd-Ngesom, other pathogenic bacteria. -

Drought and Epidemic Typhus, Central Mexico, 1655–1918 Jordan N
HISTORICAL REVIEW Drought and Epidemic Typhus, Central Mexico, 1655–1918 Jordan N. Burns, Rudofo Acuna-Soto, and David W. Stahle Epidemic typhus is an infectious disease caused by the Mexican revolution. Mexico’s rich historical record the bacterium Rickettsia prowazekii and transmitted by of epidemic disease is documented in archives of demo- body lice (Pediculus humanus corporis). This disease oc- graphic data that include census records, health records, curs where conditions are crowded and unsanitary. This dis- death certificates, and accounts of physicians. Mexico ease accompanied war, famine, and poverty for centuries. City and the high, densely populated valleys of central Historical and proxy climate data indicate that drought was Mexico were particularly susceptible to smallpox, chol- a major factor in the development of typhus epidemics in Mexico during 1655–1918. Evidence was found for 22 large era, and typhus epidemics because of crowding and poor typhus epidemics in central Mexico, and tree-ring chronolo- sanitation (4). Numerous epidemics, some identified as gies were used to reconstruct moisture levels over central typhus, occurred during the colonial and early modern Mexico for the past 500 years. Below-average tree growth, eras. We have compiled a record of 22 typhus epidemics reconstructed drought, and low crop yields occurred during in Mexico during 1655–1918. We compared the timing 19 of these 22 typhus epidemics. Historical documents de- of these typhus epidemics with tree-ring reconstructions scribe how drought created large numbers of environmental of growing-season moisture conditions to assess the re- refugees that fled the famine-stricken countryside for food lationship between climate and typhus during this period. -
A Streamlined Method for Transposon Mutagenesis of Rickettsia Parkeri
bioRxiv preprint doi: https://doi.org/10.1101/277160; this version posted March 8, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 A streamlined method for transposon mutagenesis of 2 Rickettsia parkeri yields numerous mutations that 3 impact infection 4 5 Rebecca L. Lamason1,#a,*, Natasha M. Kafai1,#b, and Matthew D. Welch1* 6 7 8 1 Department of Molecular and Cell Biology, University of California, Berkeley, Berkeley, 9 CA 10 #a Current address: Department of Biology, Massachusetts Institute of Technology, 11 Cambridge, MA 12 #b Current address: Medical Scientist Training Program, Washington University in St. 13 Louis School of Medicine, St. Louis, MO 14 15 16 17 18 * Co-corresponding authors 19 E-mail: [email protected], [email protected] 20 1 bioRxiv preprint doi: https://doi.org/10.1101/277160; this version posted March 8, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 21 Abstract 22 The rickettsiae are obligate intracellular alphaproteobacteria that exhibit a complex 23 infectious life cycle in both arthropod and mammalian hosts. As obligate intracellular 24 bacteria, Rickettsia are highly adapted to living inside a variety of host cells, including 25 vascular endothelial cells during mammalian infection. Although it is assumed that the 26 rickettsiae produce numerous virulence factors that usurp or disrupt various host cell 27 pathways, they have been challenging to genetically manipulate to identify the key 28 bacterial factors that contribute to infection. -

Volume - I Ii Issue - Xxviii Jul / Aug 2008
VOLUME - I II ISSUE - XXVIII JUL / AUG 2008 With a worldwide footprint, Rickettsiosis are diseases that are gaining increasing significance as important causes of morbidity and to an extent mortality too. Encompassed within these are two main groups, viz., Rickettsia spotted fever group and the Typhus group (they differ in their surface exposed protein and lipopolysaccharide antigens). A unique thing about these organisms is that, though they are gram-negative bacilli, they 1 Editorial cannot be cultured in the traditional ways that we employ to culture regular bacteria. They Disease need viable eukaryotic host cells and they require a vector too to complete their run up to 2 Diagnosis the human host. Asia can boast of harbouring Epidemic typhus, Scrub typhus, Boutonneuse fever, North Asia Tick typhus, Oriental spotted fever and Q fever. The Interpretation pathological feature in most of these fevers is involvement of the microvasculature 6 (vasculitis/ perivasculitis at various locations). Most often, the clinical presentation initially Trouble is like Pyrexia of Unknown Origin. As they can't be cultured by the routine methods, the 7 Shooting diagnostic approach left is serological assays. A simple to perform investigation is the Weil-Felix reaction that is based on the cross-reactive antigens of OX-19 and OX-2 strains 7 Bouquet of Proteus vulgaris. Diagnosed early, Rickettsiae can be effectively treated by the most basic antibiotics like tetracyclines/ doxycycline and chloramphenicol. Epidemiologically almost omnipresent, the DISEASE DIAGNOSIS segment of this issue comprehensively 8 Tulip News discusses Rickettsiae. Vector and reservoir control, however, is the best approach in any case.