Hydrogen Sulfide Metabolite, Sodium Thiosulfate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oxygen Is Instrumental for Biological Signaling: an Overview
Review Oxygen Is Instrumental for Biological Signaling: An Overview John T. Hancock Department of Applied Sciences, University of the West of England, Bristol BS16 1QY, UK; [email protected]; Tel.: +44-(0)117-328-2475 Abstract: Control of cellular function is extremely complex, being reliant on a wide range of compo- nents. Several of these are small oxygen-based molecules. Although reactive compounds containing oxygen are usually harmful to cells when accumulated to relatively high concentrations, they are also instrumental in the control of the activity of a myriad of proteins, and control both the upregulation and downregulation of gene expression. The formation of one oxygen-based molecule, such as the superoxide anion, can lead to a cascade of downstream generation of others, such as hydrogen · peroxide (H2O2) and the hydroxyl radical ( OH), each with their own reactivity and effect. Nitrogen- based signaling molecules also contain oxygen, and include nitric oxide (NO) and peroxynitrite, both instrumental among the suite of cell signaling components. These molecules do not act alone, but form part of a complex interplay of reactions, including with several sulfur-based compounds, such as glutathione and hydrogen sulfide (H2S). Overaccumulation of oxygen-based reactive compounds may alter the redox status of the cell and lead to programmed cell death, in processes referred to as oxidative stress, or nitrosative stress (for nitrogen-based molecules). Here, an overview of the main oxygen-based molecules involved, and the ramifications of their production, is given. Keywords: carbon monoxide; hydrogen peroxide; hydroxyl radicals; hydrogen sulfide; NADPH oxidase; nitric oxide; peroxynitrite; redox; superoxide Citation: Hancock, J.T. -

Supplementary Materials
Supplementary Materials COMPARATIVE ANALYSIS OF THE TRANSCRIPTOME, PROTEOME AND miRNA PROFILE OF KUPFFER CELLS AND MONOCYTES Andrey Elchaninov1,3*, Anastasiya Lokhonina1,3, Maria Nikitina2, Polina Vishnyakova1,3, Andrey Makarov1, Irina Arutyunyan1, Anastasiya Poltavets1, Evgeniya Kananykhina2, Sergey Kovalchuk4, Evgeny Karpulevich5,6, Galina Bolshakova2, Gennady Sukhikh1, Timur Fatkhudinov2,3 1 Laboratory of Regenerative Medicine, National Medical Research Center for Obstetrics, Gynecology and Perinatology Named after Academician V.I. Kulakov of Ministry of Healthcare of Russian Federation, Moscow, Russia 2 Laboratory of Growth and Development, Scientific Research Institute of Human Morphology, Moscow, Russia 3 Histology Department, Medical Institute, Peoples' Friendship University of Russia, Moscow, Russia 4 Laboratory of Bioinformatic methods for Combinatorial Chemistry and Biology, Shemyakin-Ovchinnikov Institute of Bioorganic Chemistry of the Russian Academy of Sciences, Moscow, Russia 5 Information Systems Department, Ivannikov Institute for System Programming of the Russian Academy of Sciences, Moscow, Russia 6 Genome Engineering Laboratory, Moscow Institute of Physics and Technology, Dolgoprudny, Moscow Region, Russia Figure S1. Flow cytometry analysis of unsorted blood sample. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S2. Flow cytometry analysis of unsorted liver stromal cells. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S3. MiRNAs expression analysis in monocytes and Kupffer cells. Full-length of heatmaps are presented. -

Thiosulfate De Sodium Sterop
Thiosulfate de Sodium Sterop 1. DENOMINATION DU MEDICAMENT THIOSULFATE DE SODIUM STEROP 1g/5ml solution injectable 2. COMPOSITION QUALITATIVE ET QUANTITATIVE Substance active : Une ampoule de 5ml contient 1g de thiosulfate de sodium dans de l’eau pour préparations injectables. 1 ml de solution contient 200mg de thiosulfate de sodium. Pour la liste complète des excipients, voir rubrique 6.1. 3. FORME PHARMACEUTIQUE Solution injectable. 4. DONNEES CLINIQUES 4.1 Indications thérapeutiques - Antidote dans le traitement des intoxications par les cyanures ainsi que par le nitroprussiate de sodium. - Prévention des effets néphrotoxiques du cisplatine. Thiosulfate de Sodium Sterop © Pharma.be Pagina 1 van 6 4.2 Posologie et mode d’administration Mode d'administration Pour voie intraveineuse lente. Posologie Intoxications par les cyanures: Adultes: La posologie habituelle est de 12,5 g de thiosulfate de sodium, administré par voie I.V. sur une période de 5 à 10 minutes. Enfants: La posologie habituelle est de 412,5 mg de thiosulfate de sodium par kg, administré par voie I.V. à la vitesse de 0,625 à 1,25 g/minute sur une période de 5 à 10 minutes. Si les symptômes persistent ou réapparaissent dans la demi-heure ou dans l’heure ayant suivi la première injection, une seconde injection de thiosulfate de sodium est nécessaire avec comme posologie la moitié de celle de la première injection. En prévention des effets néphrotoxiques du cisplatine: Chez l'adulte, la posologie initiale est de 9 g de thiosulfate de sodium par m2 de surface corporelle, administré par voie I.V. Elle est suivie par l'injection de 1,2 g de thiosulfate de sodium par m2 de surface corporelle par heure, en perfusion I.V. -

Electronic Supplementary Material (ESI) for Metallomics
Electronic Supplementary Material (ESI) for Metallomics. This journal is © The Royal Society of Chemistry 2018 Uniprot Entry name Gene names Protein names Predicted Pattern Number of Iron role EC number Subcellular Membrane Involvement in disease Gene ontology (biological process) Id iron ions location associated 1 P46952 3HAO_HUMAN HAAO 3-hydroxyanthranilate 3,4- H47-E53-H91 1 Fe cation Catalytic 1.13.11.6 Cytoplasm No NAD biosynthetic process [GO:0009435]; neuron cellular homeostasis dioxygenase (EC 1.13.11.6) (3- [GO:0070050]; quinolinate biosynthetic process [GO:0019805]; response to hydroxyanthranilate oxygenase) cadmium ion [GO:0046686]; response to zinc ion [GO:0010043]; tryptophan (3-HAO) (3-hydroxyanthranilic catabolic process [GO:0006569] acid dioxygenase) (HAD) 2 O00767 ACOD_HUMAN SCD Acyl-CoA desaturase (EC H120-H125-H157-H161; 2 Fe cations Catalytic 1.14.19.1 Endoplasmic Yes long-chain fatty-acyl-CoA biosynthetic process [GO:0035338]; unsaturated fatty 1.14.19.1) (Delta(9)-desaturase) H160-H269-H298-H302 reticulum acid biosynthetic process [GO:0006636] (Delta-9 desaturase) (Fatty acid desaturase) (Stearoyl-CoA desaturase) (hSCD1) 3 Q6ZNF0 ACP7_HUMAN ACP7 PAPL PAPL1 Acid phosphatase type 7 (EC D141-D170-Y173-H335 1 Fe cation Catalytic 3.1.3.2 Extracellular No 3.1.3.2) (Purple acid space phosphatase long form) 4 Q96SZ5 AEDO_HUMAN ADO C10orf22 2-aminoethanethiol dioxygenase H112-H114-H193 1 Fe cation Catalytic 1.13.11.19 Unknown No oxidation-reduction process [GO:0055114]; sulfur amino acid catabolic process (EC 1.13.11.19) (Cysteamine -

Adult BLS Standing Orders • Ensure EMS Provider Safety, Consider HAZMAT Activation
Imperial County Public Health Department Emergency Medical Services Agency Policy/Procedure/Protocol Manual Treatment Protocols Date: 07/01/2021 Poisoning/Intoxication/Envenomation - Adult Policy #9160A Adult BLS Standing Orders • Ensure EMS provider safety, consider HAZMAT activation. Recognize, Notify, Isolate • Universal Patient Protocol • Do not approach patient or location if scene safety is in question • Obtain accurate history of incident: o Name of product or substance o Quantity ingested, and/or duration of exposure o Time elapsed since exposure o If safe and accessible, bring medications or bottles to hospital • Move victim(s) to safe environment • Externally decontaminate - PRN • Continuously monitor ECG, blood pressure, pulse oximetry, and capnography (if ALS present) PRN • Give oxygen and provide airway support per Airway Policy • Contact Poison Control Center as needed 1 (800) 222-1222 Suspected Opioid Overdose with Respirations <12 RPM • If possible, avoid the use of a supraglottic device prior to the administration of naloxone • Administer naloxone 0.1 mg/kg, max of 2 mg IN. May repeat up to three (3) times, q5min • May assist family/friends on-scene with administration of patient’s own naloxone • NOTE - Use with caution in opioid dependent pain management patients • Assess vitals, with specific attention to respiratory rate and respiratory drive • Note pupil exam • Note drug paraphernalia or medication bottles near patient Suspected Stimulant Overdose with Sudden Hypoventilation, Oxygen Desaturation, or Apnea • High flow -

Ingestions, Intoxications, and the Critically Ill Child Poisoning in Children
Ingestions, Intoxications, and the Critically Ill Child Poisoning in Children • 1 million cases of exposure to toxins in children younger than 6 years reported in the U.S. In 1993 • estimated that another 1 million exposures to toxins not reported • 1% have moderate or major life-threatening symptoms • 60-100 deaths annually in the U.S Poisoning in Children Less Than 5 Years Old • accounts for 85-90% of pediatric poisoning • is generally accidental • secondary to exploratory behavior and lack of supervision • tend to involve single agent ingestions Poisoning in Children Over 5 Years Old • accounts for 10-15% of pediatric poisoning • is generally intentional • secondary to suicide attempts or gestures, or to intoxications and inadvertent overdose • tend to involve multiple agent ingestions General Concepts for Pediatric Poisoning • Prevention • Initial Stabilization • Diagnosis • Specific Antidotes Management of the Poisoned Child • Treat the Patient, Not the Poison --patient-specific treatment is safer, less expensive, and more effective Management of the Poisoned Child • Stabilization --Airway --Breathing --Circulation --Disability (neurologic) Management of the Poisoned Child • Respiratory Failure --airway obstruction from secretions, refluxed gastric contents, airway muscle relaxation --respiratory muscle rigidity --loss of respiratory drive --pulmonary edema Management of the Poisoned Child • Cardiovascular Collapse --arteriolar dilation --venous dilation --myocardial depression --dysrhythmias Management of the Poisoned Child • Neurologic -
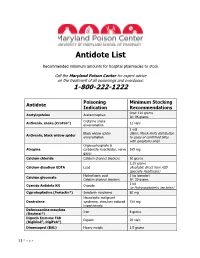
Antidote List
Antidote List Recommended minimum amounts for hospital pharmacies to stock Call the Maryland Poison Center for expert advice on the treatment of all poisonings and overdoses: 1-800-222-1222 Poisoning Minimum Stocking Antidote Indication Recommendations Oral: 120 grams Acetylcysteine Acetaminophen IV: 96 grams Crotaline snake Antivenin, snake (CroFab®) 12 vials envenomation 1 vial Black widow spider (Note: Merck limits distribution Antivenin, black widow spider envenomation to cases of confirmed bites with symptoms only) Organophosphate & Atropine carbamate insecticides, nerve 165 mg gases Calcium chloride Calcium channel blockers 10 grams 2.25 grams Calcium disodium EDTA Lead (Available direct from ASD Specialty Healthcare) Hydrofluoric acid 1 kg (powder) Calcium gluconate Calcium channel blockers IV: 30 grams 1 kit Cyanide Antidote Kit Cyanide (or Hydroxocobalamin, see below) Cyproheptadine (Periactin®) Serotonin syndrome 80 mg Neuroleptic malignant Dantrolene syndrome, stimulant-induced 720 mg hyperthermia Deferoxamine mesylate Iron 8 grams (Desferal®) Digoxin Immune FAB Digoxin 20 vials (Digibind®, DigiFab®) Dimercaprol (BAL) Heavy metals 1.5 grams 1 | P a g e Maryland Poison Center Antidote List – continued Poisoning Minimum Stocking Antidote Indication Recommendations DMSA (Succimer, Chemet®) Heavy metals 2000 mg Folic acid Methanol IV: 150 mg Flumazenil (Romazicon®) Benzodiazepines 10 mg Fomepizole (Antizol®) Ethylene glycol, methanol 12 grams Beta blockers, Glucagon 50 mg calcium channel blockers Hydroxocobalamin (Cyanokit®) Cyanide -
Springer Handbook of Enzymes
Dietmar Schomburg and Ida Schomburg (Eds.) Springer Handbook of Enzymes Volume 25 Class 1 • Oxidoreductases X EC 1.9-1.13 co edited by Antje Chang Second Edition 4y Springer Index of Recommended Enzyme Names EC-No. Recommended Name Page 1.13.11.50 acetylacetone-cleaving enzyme 673 1.10.3.4 o-aminophenol oxidase 149 1.13.12.12 apo-/?-carotenoid-14',13'-dioxygenase 732 1.13.11.34 arachidonate 5-lipoxygenase 591 1.13.11.40 arachidonate 8-lipoxygenase 627 1.13.11.31 arachidonate 12-lipoxygenase 568 1.13.11.33 arachidonate 15-lipoxygenase 585 1.13.12.1 arginine 2-monooxygenase 675 1.13.11.13 ascorbate 2,3-dioxygenase 491 1.10.2.1 L-ascorbate-cytochrome-b5 reductase 79 1.10.3.3 L-ascorbate oxidase 134 1.11.1.11 L-ascorbate peroxidase 257 1.13.99.2 benzoate 1,2-dioxygenase (transferred to EC 1.14.12.10) 740 1.13.11.39 biphenyl-2,3-diol 1,2-dioxygenase 618 1.13.11.22 caffeate 3,4-dioxygenase 531 1.13.11.16 3-carboxyethylcatechol 2,3-dioxygenase 505 1.13.11.21 p-carotene 15,15'-dioxygenase (transferred to EC 1.14.99.36) 530 1.11.1.6 catalase 194 1.13.11.1 catechol 1,2-dioxygenase 382 1.13.11.2 catechol 2,3-dioxygenase 395 1.10.3.1 catechol oxidase 105 1.13.11.36 chloridazon-catechol dioxygenase 607 1.11.1.10 chloride peroxidase 245 1.13.11.49 chlorite O2-lyase 670 1.13.99.4 4-chlorophenylacetate 3,4-dioxygenase (transferred to EC 1.14.12.9) . -

Sulfur Oxygenase Reductases - a Structural and Biochemical Perspective
Sulfur Oxygenase Reductases - A Structural and Biochemical Perspective vom Fachbereich Biologie der Technischen Universität Darmstadt zur Erlangung des akademischen Grades eines Doctor rerum naturalium genehmigte Dissertation vorgelegt von Dipl. Biol. Andreas Veith aus Seeheim-Jugenheim 1. Referent: Dr. habil. Arnulf Kletzin 2. Referent: Prof. Dr. Felicitas Pfeifer Eingereicht am 21.07.2011 Tag der mündlichen Prüfung: 16.09.2011 Darmstadt 2011 D 17 "Trying to determine the structure of a protein by UV spectroscopy was like trying to determine the structure of a piano by listening to the sound it made while being dropped down a flight of stairs." -- Francis Crick Die vorliegende Arbeit wurde als Promotionsarbeit am Institut für Mikrobiologie und Genetik des Fachbereichs Biologie der Technischen Universität Darmstadt unter Leitung von Herrn Dr. Arnulf Kletzin in der Abteilung von Frau Prof. Felicitas Pfeifer im Zeitraum von Mai 2007 bis Juli 2011 angefertigt. Ein Teil der vorliegenden Arbeit wurde in Portugal am Instituto de Tecnologia Químicia e Biológica, Universidade Nova de Lisboa (ITQB/UNL), Oeiras, Portugal in der Arbeitsgruppe von Dr. Carlos Frazão, Dr. Cláudio M. Gomes und Prof. Miguel Teixeira im Rahmen einer Kooperation durchgeführt. Ehrenwörtliche Erklärung Ich erkläre hiermit ehrenwörtlich, dass ich die vorliegende Arbeit selbstständig angefertigt habe. Sämtliche aus fremden Quellen direkt oder indirekt übernommenen Gedanken sind als solche kenntlich gemacht. Die Arbeit wurde bisher keiner anderen Prüfungsbehörde vorgelegt und noch nicht veröffentlicht. Darmstadt, den 21.07.2011 Andreas Veith Acknowledgements First and foremost I would like to thank my supervisor Dr. Arnulf Kletzin for giving me the opportunity to step into the fascinating world of proteins. -

(Riscs) in Acidithiobacillus Thiooxidans
ARTICLE Stoichiometric Modeling of Oxidation of Reduced Inorganic Sulfur Compounds (Riscs) in Acidithiobacillus thiooxidans Roberto A. Bobadilla Fazzini,1 Maria Paz Corte´s,2,3 Leandro Padilla,1 Daniel Maturana,2,3 Marko Budinich,2,3 Alejandro Maass,3,4 Pilar Parada1 1 BioSigma ‘S.A.’, Loteo Los Libertadores, Lote 106, Colina, Chile; telephone: 56-2-437 9030; fax: 56-2-460 0416; e-mail: [email protected], [email protected] 2 Laboratory of Bioinformatics and Mathematics of the Genome, Center for Mathematical Modeling (UMI2807-CNRS) and FONDAP Center for Genome Regulation, Santiago, Chile 3 Faculty of Mathematical and Physical Sciences, University of Chile, Santiago, Chile 4 Department of Mathematical Engineering, Center for Mathematical Modeling (UMI2807-CNRS) and FONDAP Center for Genome Regulation, Santiago, Chile dioxygenase as the main catalyzer and a moderate function ABSTRACT: The prokaryotic oxidation of reduced inorgan- of tetrathionate hydrolase in elemental sulfur catabolism, ic sulfur compounds (RISCs) is a topic of utmost impor- demonstrating that this model constitutes an advanced tance from a biogeochemical and industrial perspective. instrument for the optimization of At. thiooxidans biomass Despite sulfur oxidizing bacterial activity is largely known, production with potential use in biohydrometallurgical and no quantitative approaches to biological RISCs oxidation environmental applications. have been made, gathering all the complex abiotic and Biotechnol. Bioeng. 2013;110: 2242–2251. enzymatic stoichiometry involved. Even though in the ß 2013 Wiley Periodicals, Inc. case of neutrophilic bacteria such as Paracoccus and Beggia- KEYWORDS: At. thiooxidans; reduced Inorganic sulfur toa species the RISCs oxidation systems are well described, compounds (RISCs); chemolithoautotrophic oxidation there is a lack of knowledge for acidophilic microorganisms. -

Structural Enzymology of Sulfide Oxidation by Persulfide Dioxygenase and Rhodanese
Structural Enzymology of Sulfide Oxidation by Persulfide Dioxygenase and Rhodanese by Nicole A. Motl A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Biological Chemistry) in the University of Michigan 2017 Doctoral Committee Professor Ruma Banerjee, Chair Assistant Professor Uhn-Soo Cho Professor Nicolai Lehnert Professor Stephen W. Ragsdale Professor Janet L. Smith Nicole A. Motl [email protected] ORCID iD: 0000-0001-6009-2988 © Nicole A. Motl 2017 ACKNOWLEDGEMENTS I would like to take this opportunity to acknowledge the many people who have provided me with guidance and support during my doctoral studies. First I would like to express my appreciation and gratitude to my advisor Dr. Ruma Banerjee for the mentorship, guidance, support and encouragement she has provided. I would like to thank my committee members Dr. Uhn-Soo Cho, Dr. Nicolai Lehnert, Dr. Stephen Ragsdale and Dr. Janet Smith for their advice, assistance and support. I would like to thank Dr. Janet Smith and members of Dr. Smith’s lab, especially Meredith Skiba, for sharing their expertise in crystallography. I would like to thank Dr. Omer Kabil for his help, suggestions and discussions in various aspects of my study. I would also like to thank members of Dr. Banerjee’s lab for their suggestions and discussions. Additionally, I would like to thank my friends and family for their support. ii TABLE OF CONTENTS ACKNOWLEDGEMENTS ii LIST OF TABLES viii LIST OF FIGURES ix ABBREVIATIONS xi ABSTRACT xii CHAPTER I. Introduction: -

Mitochondrial Peroxynitrite Generation Is Mainly Driven by Superoxide Steady-State Concentration Rather Than by Nitric Oxide Steady-State Concentration
International Journal of Molecular Biology: Open Access Review Article Open Access Mitochondrial peroxynitrite generation is mainly driven by superoxide steady-state concentration rather than by nitric oxide steady-state concentration Abstract Volume 3 Issue 2 - 2018 - - In biological systems, ONOO production depends on production rates of NO and O2 , and on the reactions of these two free radicals with other biological components, which Laura B Valdez,1,2 Silvina S Bombicino,1 Darío limit the local concentrations of NO and O -. In mitochondria, O - is generated through 2 2 E Iglesias,1,2 Ivana Rukavina Mikusic A,1,2 the auto oxidation of semiquinones at Complexes I and III, and it may suffer the SOD- 1,2 catalyzed dismutation reaction to produce H O or react with NO in a classical termination Alberto Boveris 2 2 1 reaction between free radicals. These diffusion-controlled reactions kinetically compete for University of Buenos Aires, Physical Chemistry Division, Argentina O - degradation. Results from our laboratory have shown that even in physiopathological 2 2 situations in which NO production is reduced, such as the mitochondrial dysfunction University of Buenos Aires, Institute of Biochemistry and Molecular Medicine (IBIMOL), Argentina associated to stunned heart, mitochondrial ONOO- production rate may be slightly - - increased if the steady-state concentration of O2 is augmented. The enhancement in O2 concentration leads to an increase in its degradation by reaction with NO, decreasing NO Correspondence: Laura B Valdez, Cátedra de Fisicoquímica, bioavailability and increasing ONOO- production rate. Therefore, mitochondrial ONOO- Facultad de Farmacia y Bioquímica, Universidad de Buenos Aires, Junín 956, C1113AAD, Buenos Aires, Argentina, Tel+ 54-11-5287- generation is mainly driven by O - rather than by NO steady-state concentrations.