Skull Fractures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Basic Concepts in Basic Concepts in Dysmorphology
Basic Concepts in Dysmorphology Samia Temtamy* & Mona Aglan** *Professor of Human Genetics **Professor of Clinical Genetics Human Genetics & Genome Research Division National Research Centre, Cairo, Egypt OtliOutline y Definition of dysmorphology y Definition of terms routinely used in the description of birth defects y Impact of malformations y The difference between major & minor anomalies y Approach to a dysmorphic individual: y Suspicion & analysis y Systematic physical examination y CfitifdiConfirmation of diagnos is y Intervention y Summary 2 DfiitiDefinition of fd dysmorph hlology y The term “dysmorphology” was first coined by Dr. DidSithUSAiDavid Smith, USA in 1960s. y It implies study of human congenital defects and abnormalities of body structure that originate before birth. y The term “dysmorphic” is used to describe individuals whose physical fffeatures are not usually found in other individuals with the same age or ethnic background. y “Dys” (Greek)=disordered or abnormal and “Morph”=shape 3 Definition of terms routinely used in the d escri pti on of bi rth d ef ect s y A malformation / anomaly: is a primary defect where there i s a bas ic a ltera tion o f s truc ture, usuall y occurring before 10 weeks of gestation. y Examples: cleft palate, anencephaly, agenesis of limb or part of a limb. 4 Cleft lip & palate Absence of digits (ectrodactyly) y Malformation Sequence: A pattern of multiple defects resulting from a single primary malformation. y For example: talipes and hydrocephalus can result from a lumbar neural tube defect. Lumbar myelomeningeocele 5 y Malformation Syndrome: A pattern of features, often with an underlying cause, that arises from several different errors in morphogenesis. -
New Guidelines Review Evidence on PT, Helmets for Positional Plagiocephaly by Sandi K
Neurologic Disorders, Neurological Surgery, News Articles New guidelines review evidence on PT, helmets for positional plagiocephaly by Sandi K. Lam M.D., M.B.A., FACS; Thomas G. Luerssen M.D., FACS, FAAP Positional plagiocephaly is a common condition encountered by pediatricians and referred to pediatric subspecialty physicians such as neurosurgeons and plastic surgeons. About one in four U.S. infants has some degree of positional plagiocephaly. The incidence has increased since the Academy initiated the Back to Sleep campaign in 1994 to prevent sudden infant death syndrome. Due to practice variation in diagnosis and treatment paradigms for this common condition, the Joint Section on Pediatric Neurosurgery of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons (CNS) sought to develop evidence-based management guidelines. A multidisciplinary task force conducted a systematic review of the literature from 1966 to October 2014 on pediatric plagiocephaly. Nearly 400 abstracts were reviewed yielding 110 articles for full review; 60 were deemed relevant. The task force made 10 recommendations pertaining to imaging diagnosis, repositioning, physical therapy and helmet orthoses. The guidelines are published in CNS' journal Neurosurgery and have been endorsed by the Academy. They are available at http://bit.ly/2d7NzS1. Definition of positional plagiocephaly In the guidelines, the term positional plagiocephaly encompasses both positional occipital plagiocephaly (unilateral flattening of parieto-occipital region, compensatory anterior shift of the ipsilateral ear, bulging of the ipsilateral forehead) and positional brachycephaly (symmetric flattening of the occiput, foreshortened anterior- posterior dimension of the skull, compensatory biparietal widening) and the combination of both of these deformities. -
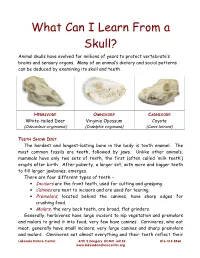
What Can I Learn from a Skull? Animal Skulls Have Evolved for Millions of Years to Protect Vertebrate’S Brains and Sensory Organs
What Can I Learn From a Skull? Animal skulls have evolved for millions of years to protect vertebrate’s brains and sensory organs. Many of an animal’s dietary and social patterns can be deduced by examining its skull and teeth. HERBIVORE OMNIVORE CARNIVORE White-tailed Deer Virginia Opossum Coyote (Odocoileus virginianus) (Didelphis virginiana) (Canis latrans) TEETH SHOW DIET . The hardest and longest-lasting bone in the body is tooth enamel. The most common fossils are teeth, followed by jaws. Unlike other animals, mammals have only two sets of teeth, the first (often called ‘milk teeth’) erupts after birth. After puberty, a larger set, with more and bigger teeth to fill larger jawbones, emerges. There are four different types of teeth – • Incisors are the front teeth, used for cutting and grasping. • Canines are next to incisors and are used for tearing. • Premolars , located behind the canines, have sharp edges for crushing food. • Molars , the very back teeth, are broad, flat grinders. Generally, herbivores have large incisors to nip vegetation and premolars and molars to grind it into food; very few have canines. Carnivores, who eat meat, generally have small incisors, very large canines and sharp premolars and molars. Omnivores eat almost everything and their teeth reflect their Lakeside Nature Center 4701 E Gregory, KCMO 64132 816-513-8960 www.lakesidenaturecenter.org preferences; they have all four types of teeth. In fact, if you’d like to see an excellent example of an omnivore’s teeth, look in the mirror. EYE PLACEMENT IDENTIFIES PREDATORS . Carnivores generally have large eyes, placed so that the eyes look forward and the areas of vision of the two eyes overlap. -

Direct Sagittal CT in the Evaluation of Temporal Bone Disease
371 Direct Sagittal CT in the Evaluation of Temporal Bone Disease 1 Mahmood F. Mafee The human temporal bone is an extremely complex structure. Direct axial and coronal Arvind Kumar2 CT sections are quite satisfactory for imaging the anatomy of the temporal bone; Christina N. Tahmoressi1 however, many relationships of the normal and pathologic anatomic detail of the Barry C. Levin2 temporal bone are better seen with direct sagittal CT sections. The sagittal projection Charles F. James1 is of interest to surgeons, as it has the advantage of following the plane of surgical approach. This article describes the advantages of using direct sagittal sections for Robert Kriz 1 1 studying various diseases of the temporal bone. The CT sections were obtained with Vlastimil Capek the aid of a new headholder added to our GE CT 9800 scanner. The direct sagittal projection was found to be extremely useful for evaluating diseases involving the vertical segment of the facial nerve canal, vestibular aqueduct, tegmen tympani, sigmoid sinus plate, sinodural angle, carotid canal, jugular fossa, external auditory canal, middle ear cavity, infra- and supra labyrinthine air cells, and temporo mandibular joint. CT has contributed greatly to an understanding of the complex anatomy and spatial relationship of the minute structures of the hearing and balance organs, which are packed into a small pyramid-shaped petrous temporal bone [1 , 2]. In the past 6 years, high-resolution CT scanning has been rapidly replacing standard tomography and has proved to be the diagnostic imaging method of choice for studying the normal and pathologic details of the temporal bone [3-14]. -

Implications to Occipital Headache
The Journal of Neuroscience, March 6, 2019 • 39(10):1867–1880 • 1867 Neurobiology of Disease Non-Trigeminal Nociceptive Innervation of the Posterior Dura: Implications to Occipital Headache X Rodrigo Noseda, Agustin Melo-Carrillo, Rony-Reuven Nir, Andrew M. Strassman, and XRami Burstein Department of Anesthesia, Critical Care and Pain Medicine, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, Massachusetts 02115 Current understanding of the origin of occipital headache falls short of distinguishing between cause and effect. Most preclinical studies involving trigeminovascular neurons sample neurons that are responsive to stimulation of dural areas in the anterior 2/3 of the cranium and the periorbital skin. Hypothesizing that occipital headache may involve activation of meningeal nociceptors that innervate the posterior 1⁄3 of the dura, we sought to map the origin and course of meningeal nociceptors that innervate the posterior dura overlying the cerebellum. Using AAV-GFP tracing and single-unit recording techniques in male rats, we found that neurons in C2–C3 DRGs innervate the dura of the posterior fossa; that nearly half originate in DRG neurons containing CGRP and TRPV1; that nerve bundles traverse suboccipital muscles before entering the cranium through bony canals and large foramens; that central neurons receiving nociceptive information from the posterior dura are located in C2–C4 spinal cord and that their cutaneous and muscle receptive fields are found around the ears, occipital skin and neck muscles; and that administration of inflammatory mediators to their dural receptive field, sensitize their responses to stimulation of the posterior dura, peri-occipital skin and neck muscles. These findings lend rationale for the common practice of attempting to alleviate migraine headaches by targeting the greater and lesser occipital nerves with anesthetics. -

Frontosphenoidal Synostosis: a Rare Cause of Unilateral Anterior Plagiocephaly
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library Childs Nerv Syst (2007) 23:1431–1438 DOI 10.1007/s00381-007-0469-4 ORIGINAL PAPER Frontosphenoidal synostosis: a rare cause of unilateral anterior plagiocephaly Sandrine de Ribaupierre & Alain Czorny & Brigitte Pittet & Bertrand Jacques & Benedict Rilliet Received: 30 March 2007 /Published online: 22 September 2007 # Springer-Verlag 2007 Abstract Conclusion Frontosphenoidal synostosis must be searched Introduction When a child walks in the clinic with a in the absence of a coronal synostosis in a child with unilateral frontal flattening, it is usually associated in our anterior unilateral plagiocephaly, and treated surgically. minds with unilateral coronal synostosis. While the latter might be the most common cause of anterior plagiocephaly, Keywords Craniosynostosis . Pediatric neurosurgery. it is not the only one. A patent coronal suture will force us Anterior plagiocephaly to consider other etiologies, such as deformational plagio- cephaly, or synostosis of another suture. To understand the mechanisms underlying this malformation, the development Introduction and growth of the skull base must be considered. Materials and methods There have been few reports in the Harmonious cranial growth is dependent on patent sutures, literature of isolated frontosphenoidal suture fusion, and and any craniosynostosis might lead to an asymmetrical we would like to report a series of five cases, as the shape of the skull. The anterior skull base is formed of recognition of this entity is important for its treatment. different bones, connected by sutures, fusing at different ages. The frontosphenoidal suture extends from the end of Presented at the Consensus Conference on Pediatric Neurosurgery, the frontoparietal suture, anteriorly and inferiorly in the Rome, 1–2 December 2006. -

Imaging in Craniosynostosis: When and What?
Child's Nervous System (2019) 35:2055–2069 https://doi.org/10.1007/s00381-019-04278-x REVIEW ARTICLE Imaging in craniosynostosis: when and what? L. Massimi1,2 & F. Bianchi1 & P. Frassanito1 & R. Calandrelli3 & G. Tamburrini1,2 & M. Caldarelli1,2 Received: 17 May 2019 /Accepted: 25 June 2019 /Published online: 9 September 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose Currently, the interest on craniosynostosis in the clinical practice is raised by their increased frequency and their genetic implications other than by the still existing search of less invasive surgical techniques. These reasons, together with the problem of legal issues, make the need of a definite diagnosis for a crucial problem, even in single-suture craniosynostosis (SSC). Although the diagnosis of craniosynostosis is primarily the result of physical examination, craniometrics measuring, and obser- vation of the skull deformity, the radiological assessment currently plays an important role in the confirmation of the diagnosis, the surgical planning, and even the postoperative follow-up. On the other hand, in infants, the use of radiation or the need of sedation/anesthesia raises the problem to reduce them to minimum to preserve such a delicate category of patient from their adverse effects. Methods, results and conclusions This review aims at summarizing the state of the art of the role of radiology in craniosynostosis, mainly focusing on indications and techniques, to provide an update not only to pediatric neurosurgeons or maxillofacial surgeons but also to all the other specialists involved in their management, like neonatologists, pediatricians, clinical geneticists, and pediatric neurologists. Keywords Craniosynostosis . -

PE2812 Breaking Arm Bones a Second Time
Breaking Arm Bones a Second Time Children who have broken arm bones are at higher risk for breaking the same arm bones again if they do not go through the right treatment, for the right amount of time. How likely is it that There is up to a 5% chance (1 out of every 20 cases) of breaking forearm my child’s arm bones a second time, in the same place. There is a higher risk to break these bones again if the first fracture is in the middle of the forearm bones (as bones will break seen in the pictures below). There is a lower risk if the fracture is closer to again? the hand. Most repeat fractures tend to happen within six months after the first injury heals. First fracture Same fracture after healing for about 6 weeks 1 of 2 To Learn More Free Interpreter Services • Orthopedics and Sports Medicine • In the hospital, ask your nurse. 206-987-2109 • From outside the hospital, call the • Ask your child’s healthcare provider toll-free Family Interpreting Line, 1-866-583-1527. Tell the interpreter • seattlechildrens.org the name or extension you need. Breaking Arm Bones a Second Time How can I help my Wearing a cast for at least six weeks lowers the risk of breaking the same child lower the risk arm bones again. After wearing a cast, we recommend your child wear a brace for 4 weeks in order to protect the injured area and start improving of having a wrist movement. While your child wears a brace, we recommend they do repeated bone not participate in contact sports (e.g., soccer, football or dodge ball). -

Neurocranial Histomorphometrics
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 5-2012 Neurocranial Histomorphometrics Lindsay Hines Trammell University of Tennessee-Knoxville, [email protected] Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Biological and Physical Anthropology Commons Recommended Citation Trammell, Lindsay Hines, "Neurocranial Histomorphometrics. " PhD diss., University of Tennessee, 2012. https://trace.tennessee.edu/utk_graddiss/1359 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Lindsay Hines Trammell entitled "Neurocranial Histomorphometrics." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the requirements for the degree of Doctor of Philosophy, with a major in Anthropology. Murray K. Marks, Major Professor We have read this dissertation and recommend its acceptance: Joanne L. Devlin, David A. Gerard, Walter E. Klippel, David G. Anderson (courtesy member) Accepted for the Council: Carolyn R. Hodges Vice Provost and Dean of the Graduate School (Original signatures are on file with official studentecor r ds.) University of Tennessee, Knoxville Trace: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 5-2012 Neurocranial Histomorphometrics Lindsay Hines Trammell University of Tennessee-Knoxville, [email protected] This Dissertation is brought to you for free and open access by the Graduate School at Trace: Tennessee Research and Creative Exchange. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Mutations Within Or Upstream of the Basic Helixð Loopð Helix Domain of the TWIST Gene Are Specific to Saethre-Chotzen Syndrome
European Journal of Human Genetics (1999) 7, 27–33 © 1999 Stockton Press All rights reserved 1018–4813/99 $12.00 t http://www.stockton-press.co.uk/ejhg ARTICLES Mutations within or upstream of the basic helix–loop–helix domain of the TWIST gene are specific to Saethre-Chotzen syndrome Vincent El Ghouzzi, Elisabeth Lajeunie, Martine Le Merrer, Val´erie Cormier-Daire, Dominique Renier, Arnold Munnich and Jacky Bonaventure Unit´e de Recherches sur les Handicaps G´en´etiques de l’Enfant, Institut Necker, Paris, France Saethre-Chotzen syndrome (ACS III) is an autosomal dominant craniosynostosis syndrome recently ascribed to mutations in the TWIST gene, a basic helix–loop–helix (b-HLH) transcription factor regulating head mesenchyme cell development during cranial neural tube formation in mouse. Studying a series of 22 unrelated ACS III patients, we have found TWIST mutations in 16/22 cases. Interestingly, these mutations consistently involved the b-HLH domain of the protein. Indeed, mutant genotypes included frameshift deletions/insertions, nonsense and missense mutations, either truncating or disrupting the b-HLH motif of the protein. This observation gives additional support to the view that most ACS III cases result from loss-of-function mutations at the TWIST locus. The P250R recurrent FGFR 3 mutation was found in 2/22 cases presenting mild clinical manifestations of the disease but 4/22 cases failed to harbour TWIST or FGFR 3 mutations. Clinical re-examination of patients carrying TWIST mutations failed to reveal correlations between the mutant genotype and severity of the phenotype. Finally, since no TWIST mutations were detected in 40 cases of isolated coronal craniosynostosis, the present study suggests that TWIST mutations are specific to Saethre- Chotzen syndrome. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V.