Dietary Intake of Children Aged 1 Year To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

S Ection 2 S Ection 2 Finding S on Th E External Env Ironments Env
S ECTION 2 FINDING S ON TH E EXTERNAL ENV IRONMENTS AND EV ERYDAY FOOD P RACPRACRACTICESRACTICESTICESTICES INTRODUCTION This first section on the findings contains Chapters 4 and 5. In Chapter 4 the external environments of the participants are described. This includes not only an account of the geographical location and physical environment of Mmotla but also refers to important aspects of the socio-cultural environment of the participants. In Chapter 5 the everyday food practices of the participants are contextualised by giving a description of how they view and use food. The contemporary eating patterns as they are followed on weekdays and over weekends are reported on and interpreted. This section comprises two chapters entitled: Chapter 4: External environments of the participants Chapter 5: Everyday food practices CH AP TER 4 EXTERNAL ENV IRONMEIRONMENTSNTS OF TH E P ARTICIP ANTS 4.1 INTRODUCTION Human food choice always takes place within the boundaries of what food is available, accessible and acceptable to people and is primarily determined by the external environments in which they live as described in Chapter 2 (see 2.2.1). Each of these environments, namely the physical, economic, political and socio-cultural, provides both opportunities and constraints for human food consumption (Bryant et al., 2003:10). This exemplifies the contention that where people live contributes to their potential food choices (Kittler & Sucher, 2008:12; Bryant et al., 2003:11). In this first chapter on the findings of the study, the external environments of the participants are sketched to contextualise the contemporary food practices of the Mmotla community. -

Motor Competence in Visually Impaired Persons
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/341870616 Motor competence in visually impaired persons Book · January 2019 DOI: 10.5507/ftk.19.24455549 CITATIONS READS 0 20 2 authors, including: Janečka Zbyněk Palacký University Olomouc 15 PUBLICATIONS 19 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: dis HBSC - monitoring of lifestyle of students with special education needs View project Centra podpory integrace / Center of inclusion support View project All content following this page was uploaded by Janečka Zbyněk on 27 November 2020. The user has requested enhancement of the downloaded file. Palacký University Olomouc Faculty of Physical Culture Motor competence in visually impaired persons Zbyněk Janečka Ladislav Bláha et al. Olomouc 2019 Reviewers: Ken Black Maria Dinold First Edition Unauthorized use of the work is a breach of copyright and may be subject to civil, administrative or criminal liability. © Zbyněk Janečka, Ladislav Bláha, 2019 © Palacký University Olomouc, 2019 DOI: 10.5507/ftk.19.24455549 ISBN 978-80-244-5554-9 (print) ISBN 978-80-244-5555-6 (online : PDF) Content 1 / Terminology (Janečka, Bláha) ............................................................................................................7 2 / Type of impairment and its categorisation (Bláha) ..........................................................................11 3 / Vision (Janečka) .................................................................................................................................15 -

Preventive Aspects of Early Nutrition Nestlé Nutrition Institute Workshop Series
Preventive Aspects of Early Nutrition Nestlé Nutrition Institute Workshop Series Vol. 85 Preventive Aspects of Early Nutrition Editors Mary S. Fewtrell London, UK Ferdinand Haschke Salzburg, Austria Susan L. Prescott Perth, Australia Nestec Ltd., 55 Avenue Nestlé, CH–1800 Vevey (Switzerland) S. Karger AG, P.O. Box, CH–4009 Basel (Switzerland) www.karger.com Library of Congress Cataloging-in-Publication Data Names: Fewtrell, Mary S., editor. | Haschke, F., editor. | Prescott, Susan L., editor. Title: Preventive aspects of early nutrition / editors, Mary S. Fewtrell, Ferdinand Haschke, Susan L. Prescott. Description: Basel ; New York : Karger, [2016] | Series: Nestlé Nutrition Institute workshop series, ISSN 1664-2147 ; vol. 85 | Includes bibliographical references and index. Identifiers: LCCN 2015046033| ISBN 9783318056426 (hard cover : alk. paper) | ISBN 9783318056433 (electronic version) Subjects: | MESH: Child Nutritional Physiological Phenomena | Infant Nutritional Physiological Phenomena | Pediatric Obesity--prevention & control | Hypersensitivity--prevention & control | Congresses Classification: LCC RJ206 | NLM WS 130 | DDC 613.2083--dc23 LC record available at http://lccn.loc.gov/2015046033 The material contained in this volume was submitted as previously unpublished material, except in the instances in which credit has been given to the source from which some of the illustrative material was derived. Great care has been taken to maintain the accuracy of the information contained in the volume. However, neither Nestec Ltd. nor S. Karger AG can be held responsible for errors or for any consequences arising from the use of the information contained herein. © 2016 Nestec Ltd., Vevey (Switzerland) and S. Karger AG, Basel (Switzerland). All rights reserved. This book is protected by copyright. No part of it may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, or recording, or otherwise, without the written permission of the publisher. -

The Parliamentary Constituency Offices
REPUBLIC OF BOTSWANA THE PARLIAMENTARY CONSTITUENCY OFFICES Parliament of Botswana P O Box 240 Gaborone Tel: 3616800 Fax: 3913103 Toll Free; 0800 600 927 e - mail: [email protected] www.parliament.gov.bw Introduction Mmathethe-Molapowabojang Mochudi East Mochudi West P O Box 101 Mmathethe P O Box 2397 Mochudi P O Box 201951 Ntshinoge Representative democracy can only function effectively if the Members of Tel: 5400251 Fax: 5400080 Tel: 5749411 Fax: 5749989 Tel: 5777084 Fax: 57777943 Parliament are accessible, responsive and accountable to their constituents. Mogoditshane Molepolole North Molepolole South The mandate of a Constituency Office is to act as an extension of Parliament P/Bag 008 Mogoditshane P O Box 449 Molepolole P O Box 3573 Molepolole at constituency level. They exist to play this very important role of bringing Tel: 3915826 Fax: 3165803 Tel: 5921099 Fax: 5920074 Tel: 3931785 Fax: 3931785 Parliament and Members of Parliament close to the communities they serve. Moshupa-Manyana Nata-Gweta Ngami A constituency office is a Parliamentary office located at the headquarters of P O Box 1105 Moshupa P/Bag 27 Sowa Town P/Bag 2 Sehithwa Tel: 5448140 Fax: 5448139 Tel: 6213756 Fax: 6213240 Tel: 6872105/123 each constituency for use by a Member of Parliament (MP) to carry out his or Fax: 6872106 her Parliamentary work in the constituency. It is a formal and politically neutral Nkange Okavango Palapye place where a Member of Parliament and constituents can meet and discuss P/Bag 3 Tutume P O Box 69 Shakawe P O Box 10582 Palapye developmental issues. Tel: 2987717 Fax: 2987293 Tel: 6875257/230 Tel: 4923475 Fax: 4924231 Fax: 6875258 The offices must be treated strictly as Parliamentary offices and must therefore Ramotswa Sefhare-Ramokgonami Selibe Phikwe East be used for Parliamentary business and not political party business. -

Land Tenure Reforms and Social Transformation in Botswana: Implications for Urbanization
Land Tenure Reforms and Social Transformation in Botswana: Implications for Urbanization. Item Type text; Electronic Dissertation Authors Ijagbemi, Bayo, 1963- Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 06/10/2021 17:13:55 Link to Item http://hdl.handle.net/10150/196133 LAND TENURE REFORMS AND SOCIAL TRANSFORMATION IN BOTSWANA: IMPLICATIONS FOR URBANIZATION by Bayo Ijagbemi ____________________ Copyright © Bayo Ijagbemi 2006 A Dissertation Submitted to the Faculty of the DEPARTMENT OF ANTHROPOLOGY In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY In the Graduate College THE UNIVERSITY OF ARIZONA 2006 2 THE UNIVERSITY OF ARIZONA GRADUATE COLLEGE As members of the Dissertation Committee, we certify that we have read the dissertation prepared by Bayo Ijagbemi entitled “Land Reforms and Social Transformation in Botswana: Implications for Urbanization” and recommend that it be accepted as fulfilling the dissertation requirement for the Degree of Doctor of Philosophy _______________________________________________________________________ Date: 10 November 2006 Dr Thomas Park _______________________________________________________________________ Date: 10 November 2006 Dr Stephen Lansing _______________________________________________________________________ Date: 10 November 2006 Dr David Killick _______________________________________________________________________ Date: 10 November 2006 Dr Mamadou Baro Final approval and acceptance of this dissertation is contingent upon the candidate’s submission of the final copies of the dissertation to the Graduate College. I hereby certify that I have read this dissertation prepared under my direction and recommend that it be accepted as fulfilling the dissertation requirement. -

Annual Report 2008-2009
annual report 09 v4:Layout 1 11/8/2010 9:39 AM Page 1 Western Reserve Academy Annual Report 2008-2009 Behind each student and faculty member lie the loyalty, generosity and strength of the entire Western Reserve Academy community. annual report 09 v4:Layout 1 11/8/2010 9:39 AM Page 2 2008-2009 Board of Trustees Mark R. Tercek ’75, Daniel W. Christman ’61 Andrew R. Midler ’79 Douglas Kurdziel ’05, Co-president Alexandria, Va. St. Thomas, U.S. Virgin College Trustee Irvington, N.Y. Kathryn I. Clark ’76 Islands Nashville, Tenn. Peter S. Hellman ’68, Ann Arbor, Mich. Katie Ong-Landini ’83 Cookie Richardson, Co-president Ruth Swetland Eppig Shaker Heights, Ohio Pioneer Women President Hunting Valley, Ohio Bratenahl, Ohio Gregory Pennington ’71 Hudson, Ohio Stephan W. Cole ’66, Dagmar F. Fellowes ’75 Milwaukee, Wis. Lorraine Debose ’93, Vice President Pepper Pike, Ohio R. Lawrence Roth Alumni Association President Jupiter, Fla. New York, N.Y. Euclid, Ohio John M. Fowler ’67 Trustee Emeriti David M. Hunter ’68, Bronxville, N.Y. Hewitt B. Shaw Vice President Hudson, Ohio H. Arthur Bellows Jr. ’56 Silver Lake, Ohio Anne C. Goodman ’84 Shaker Heights, Ohio Shannah Tharp-Taylor ’91 Greenwich, Conn. Richard W. Neu, Ronald M. Harrington ’87 Pittsburgh, Pa. Jefferson W. Keener Jr. ’50 Treasurer Akron, Ohio Naples, Fla. Hudson, Ohio Jason M. Wortendyke ’94 Olin J. Heestand Jr. ’62 Chicago, Ill. T. Dixon Long ’51 Fred A. Cummings ’85, San Anselmo, Calif. Assistant Treasurer Chicago, Ill. Special Trustees Moreland Hills, Ohio Nathaniel E. Leonard ’82 David J. -

Travel and Tours Packages in Botswana
TRAVEL AND TOURS PACKAGES IN BOTSWANA 1. Sunrise Travel And Tours Email: [email protected] / [email protected] Tel: 318 7807 / 71 624 625 / 73 805 806 Day Trip Around Gaborone -Botanic Garden (Otse) (Half Day) -Three Chiefs -Mannyelanong Game Reserve -Botswana Craft -Lentswe La Baratani -Somarela Tikologo -Samora Machel Memorial -The NO 1 Ladies Detective Agency -Snack -Snack -Transport -Transport Total Price BW P850.00 Per Person Total Price BW P750.00 Per Person Ranaka (Half Day) Day Trip Around Gaborone -Poloko View Point -Gaborone Game Reserve -Mmalogage Gorge -Gaborone Dam -Ranaka Stone Walls -National Museum -Snack -Kgale Hill -Transport -Snack Total Price BW P899.00 Per Person -Transport Total Price BW P750.00 Per Person Chobe-Botswana Camping Day Trip Around Gaborone -3 Nights Acommodation -Mokolodi Nature Reserve -All Meals -Lion Park Resort -Boat Cruise -Snack -Village Tour -Transport -Vist To Kazungula Ferry Total Price BW P850.00 Per Person Total Price P2 200 PP Mmankgodi (Full Day) Kasane Package -Manyana Rock Paintings Return Transport From Gabs To Kasane -Gabane Pottery 3 Nights’ Accommodation And Breakfast -Livingstone Memorial (Lodging) -Snack Activities -Transport Village Tour Total Price BW P850.00 Per Person Boat Cruise Game Drive Kanye (Full Day) Sunset Cruise -Bathoen I Statue Visit To Lesoma Memorial -Bathoen Ii Museum Visit Kazungula Ferry -Pharing Gorge OPTIONAL -Mmakgodumo Dam -Snack A Day Trip To Victoria Falls @ Own Account Total Price BW P950.00 Per Person ***Free Photographer And Tour Manager*** -

Lrtsv27no3.Pdf
EDITORIATBOARD Editor,andChairpersonoJtheEditoriatBoard. .. Er-rzesl.rlrL'Tare AssistantEditors Psvllrs A RrcnrroNo .for Cataloging and Classification Section Eow,A,noSwaNsoN Cenorvr C. Monnow for Presewation of Library Materials Section FneNcrsF. SpnErrznr for Reproduction of Library Materials Section Section J. Mrcueel Bnuen for Resources LrNor Sepp for Serials Section Editorial Adoisu: Donts H Cr-acx (for Regional Groups) Liaisonuith RTSD Newsletter: Atrqor-o HrnsnoN, RTSD NewsletterEditor Library ResourcesI TechnicalSerares (ISSN 0024-252?), the quarterly official publication ofthe Resourcesand Technical ServicesDivision of the American Library Association,is publishedat 50 E.HuronSt.,Chicago, IL60611. BusinessOffice:AmericanLibraryAssociation,50E.HuronSt., Chicago, IL 60611. Aduntising Tralfic Coordinator;Leona Swiech, Central Production Unit, ALA Headquarters,50E. HuronSt., Chicago, IL60611. CirculationandProduction:Central Production Unit{turnals, ALA Headquarters,50 E. Huron St., Chicago,IL 60611 . SubscriptionPrice. to mem- bersof the ALA Resourcesand Technical ServicesDivision, $10 per year, included in the member- ship dues; to nonmembers, $20 per year; singlecopies $5. Second-classpostage paid at Chicago, Illinois, and at additional mailing offices.POSTMAS- TER: Send addiess changes to Librarl ResourcesI TechnicalSeruices, 50 E. Huron St., Chicago, IL 6061I Librar2 ResourcesI TechnicalSeraices is indexed in Library Literature,Librarl I InformationScience Index- Con- Absmai, CurrentIndex toJournals in Education, ScienceCitation Index, and Hospital Literature tentsarelistedin CALL(CurrmtAuareness-Librar\Literature).ItsreviewsareincludedinBookRetieu Digest,Book Reouw Infux, and Retieu of Reuieus Copies of books for review should be addressedto Arnold Hirshon, Editor, R ZSD Newsletter,Ca- bell Library, virginia commonwealth ljniversity, 901 Park Ave., Richmond, VA 23284. Do not send journal issuesor journal articles for review. The contents of this journal, unless otheruise indicated, are copyrighted by the Association. -

2011 Population & Housing Census Preliminary Results Brief
2011 Population & Housing Census Preliminary Results Brief For further details contact Census Office, Private Bag 0024 Gaborone: Tel 3188500; Fax 3188610 1. Botswana Population at 2 Million Botswana’s population has reached the 2 million mark. Preliminary results show that there were 2 038 228 persons enumerated in Botswana during the 2011 Population and Housing Census, compared with 1 680 863 enumerated in 2001. Suffice to note that this is the de-facto population – persons enumerated where they were found during enumeration. 2. General Comments on the Results 2.1 Population Growth The annual population growth rate 1 between 2001 and 2011 is 1.9 percent. This gives further evidence to the effect that Botswana’s population continues to increase at diminishing growth rates. Suffice to note that inter-census annual population growth rates for decennial censuses held from 1971 to 2001 were 4.6, 3.5 and 2.4 percent respectively. A close analysis of the results shows that it has taken 28 years for Botswana’s population to increase by one million. At the current rate and furthermore, with the current conditions 2 prevailing, it would take 23 years for the population to increase by another million - to reach 3 million. Marked differences are visible in district population annual growths, with estimated zero 3 growth for Selebi-Phikwe and Lobatse and a rate of over 4 percent per annum for South East District. Most district growth rates hover around 2 percent per annum. High growth rates in Kweneng and South East Districts have been observed, due largely to very high growth rates of villages within the proximity of Gaborone. -
The Development of a Musical to Implement the Food
UTILISATION OF TRADITIONAL AND INDIGENOUS FOODS IN THE NORTH WEST PROVINCE OF SOUTH AFRICA SARAH T.P. MATENGE (M. Consumer Sciences) Thesis submitted for the degree Doctor of Philosophy in Consumer Sciences at the Potchefstroom Campus of the North-West University Promoter: Prof. A. Kruger Co-promoter: Prof. M. van der Merwe Co-promoter: Dr. H. de Beer POTCHEFSTROOM 2011 DEDICATIONS This thesis is dedicated to: My beloved parents, Johnson Matenge and Tsholofelo Matenge who taught me how to persevere and always have hope for better outcomes in the unpredictable future. Thanks again for your guidance and patience. I love you so much. To my children, Tapiwa and Tawanda, leaving you at a time when you needed me the most was the hardest thing that I had to do in my life, but I thank the omnipresent God who is watching over you and because of him you coped reasonably well. My son Panashe, has given me sincere love and support, has endured well the tough life in Potchefstroom and has been doing a good job at school. Just one look in his eyes gave me hope. i ACKNOWLEDGEMENTS It is evident that this thesis is a product of joint efforts from many people. I would like to express my sincere gratitude to the following people who have contributed to make this study possible: Prof. A. Kruger, my promoter for her profound knowledge and her ability to see things in a bigger picture. Thanks for the hard work you have done as a supervisor. Prof. M. van der Merwe, co-promoter for her excellent guidance, expertise and selfless dedication. -

E-Government and Democracy in Botswana: Observational and Experimental Evidence on the Effects of E-Government Usage on Political Attitudes
A Service of Leibniz-Informationszentrum econstor Wirtschaft Leibniz Information Centre Make Your Publications Visible. zbw for Economics Bante, Jana et al. Working Paper E-government and democracy in Botswana: Observational and experimental evidence on the effects of e-government usage on political attitudes Discussion Paper, No. 16/2021 Provided in Cooperation with: German Development Institute / Deutsches Institut für Entwicklungspolitik (DIE), Bonn Suggested Citation: Bante, Jana et al. (2021) : E-government and democracy in Botswana: Observational and experimental evidence on the effects of e-government usage on political attitudes, Discussion Paper, No. 16/2021, ISBN 978-3-96021-153-2, Deutsches Institut für Entwicklungspolitik (DIE), Bonn, http://dx.doi.org/10.23661/dp16.2021 This Version is available at: http://hdl.handle.net/10419/234177 Standard-Nutzungsbedingungen: Terms of use: Die Dokumente auf EconStor dürfen zu eigenen wissenschaftlichen Documents in EconStor may be saved and copied for your Zwecken und zum Privatgebrauch gespeichert und kopiert werden. personal and scholarly purposes. Sie dürfen die Dokumente nicht für öffentliche oder kommerzielle You are not to copy documents for public or commercial Zwecke vervielfältigen, öffentlich ausstellen, öffentlich zugänglich purposes, to exhibit the documents publicly, to make them machen, vertreiben oder anderweitig nutzen. publicly available on the internet, or to distribute or otherwise use the documents in public. Sofern die Verfasser die Dokumente unter Open-Content-Lizenzen (insbesondere CC-Lizenzen) zur Verfügung gestellt haben sollten, If the documents have been made available under an Open gelten abweichend von diesen Nutzungsbedingungen die in der dort Content Licence (especially Creative Commons Licences), you genannten Lizenz gewährten Nutzungsrechte. -
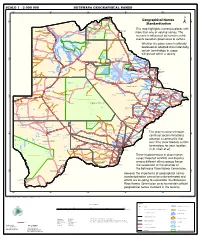
Geographical Names Standardization BOTSWANA GEOGRAPHICAL
SCALE 1 : 2 000 000 BOTSWANA GEOGRAPHICAL NAMES 20°0'0"E 22°0'0"E 24°0'0"E 26°0'0"E 28°0'0"E Kasane e ! ob Ch S Ngoma Bridge S " ! " 0 0 ' ' 0 0 ° Geographical Names ° ! 8 !( 8 1 ! 1 Parakarungu/ Kavimba ti Mbalakalungu ! ± n !( a Kakulwane Pan y K n Ga-Sekao/Kachikaubwe/Kachikabwe Standardization w e a L i/ n d d n o a y ba ! in m Shakawe Ngarange L ! zu ! !(Ghoha/Gcoha Gate we !(! Ng Samochema/Samochima Mpandamatenga/ This map highlights numerous places with Savute/Savuti Chobe National Park !(! Pandamatenga O Gudigwa te ! ! k Savu !( !( a ! v Nxamasere/Ncamasere a n a CHOBE DISTRICT more than one or varying names. The g Zweizwe Pan o an uiq !(! ag ! Sepupa/Sepopa Seronga M ! Savute Marsh Tsodilo !(! Gonutsuga/Gonitsuga scenario is influenced by human-centric Xau dum Nxauxau/Nxaunxau !(! ! Etsha 13 Jao! events based on governance or culture. achira Moan i e a h hw a k K g o n B Cakanaca/Xakanaka Mababe Ta ! u o N r o Moremi Wildlife Reserve Whether the place name is officially X a u ! G Gumare o d o l u OKAVANGO DELTA m m o e ! ti g Sankuyo o bestowed or adopted circumstantially, Qangwa g ! o !(! M Xaxaba/Cacaba B certain terminology in usage Nokaneng ! o r o Nxai National ! e Park n Shorobe a e k n will prevail within a society a Xaxa/Caecae/Xaixai m l e ! C u a n !( a d m a e a a b S c b K h i S " a " e a u T z 0 d ih n D 0 ' u ' m w NGAMILAND DISTRICT y ! Nxai Pan 0 m Tsokotshaa/Tsokatshaa 0 Gcwihabadu C T e Maun ° r ° h e ! 0 0 Ghwihaba/ ! a !( o 2 !( i ata Mmanxotae/Manxotae 2 g Botet N ! Gcwihaba e !( ! Nxharaga/Nxaraga !(! Maitengwe