Crawley CCG 2019/20 Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Crawley Borough Council
Council Meeting 27 May 2011 Crawley Borough Council Minutes of Council 27 May 2011 at 7.30 p.m. Present: Councillor L A M Burke (Mayor) was in the Chair for Minute Number 1. Councillor C R Eade (Deputy Mayor) Councillors M L Ayling, B K Blake, S A Blake, Dr H S Bloom, N Boxall, K Brockwell, B J Burgess, R G Burgess, A L I Burke, R D Burrett, A C W Crane, D G Crow, V S Cumper, C L Denman, L R Gilroy, I T Irvine, M G Jones, S J Joyce, S Kaur, P K Lamb, R A Lanzer, C C Lloyd, B MeCrow, J L Millar-Smith, C Oxlade, B J Quinn, A J E Quirk, D J Shreeves, B A Smith, G Thomas, K J Trussell and K Williamson Also in Attendance: Mr P Nicolson – Independent Member (Chair of Standards Committee). Mr A Timms – Independent Member (Vice Chair of Standards Committee). Officers Present: Lee Harris Chief Executive Ann-Maria Brown Head of Legal and Democratic Services Peter Browning Director of Environment and Housing David Covill Director of Resources Lucasta Grayson Head of People and Technology Phil Rogers Director of Community Services Roger Brownings Democratic Services Officer 1. Mayor’s Presentations and Announcement At the start of the meeting, the Mayor made a short address to the Council about his Mayoral year. The Mayor thanked his family for their support and encouragement during his year in office, and in so doing made particular reference to his wife, Councillor Ali Burke, for the significant and continuing loyal support she had given him during that term. -

North Mid Sussex
Crawley Fit for the Future Consultation Meeting held at The Friary Hall, Crawley on Saturday 27 September 2007 David Dewdney, Chairman of the East Crawley County Local Committee (CLC) informed the meeting that there were two County Local Committees in Crawley and introduced James McGough, Chairman of the West Crawley County Local Committee, who would share the Chairmanship of the Joint Meeting. Mr McGough introduced the members of the West Crawley CLC – John Mortimer, Christopher Mullins, James Smith and Janet Sully. Mr Dewdney introduced the members of the East Crawley CLC – Gillian Joyce and Henry Smith and passed on the apologies of Duncan Crow, who was unable to attend the meeting. Mr Dewdney introduced Liz Tayler, Medical Director and Consultant in Public Heath, Sue Braysher, Director for Contracting and Performance and Dr Sunil Dasan, Clinical Director for Emergency Care, from the West Sussex Primary Care Trust. Mr Dewdney then asked Henry Smith, Leader of West Sussex County Council, to speak about the reasons that the meeting had been called. Mr Smith informed the meeting that County Local Committees had been formed in March 2005 as a means for the County Council to devolve decision- making to a more local level. They were also intended to hear local people’s views on strategic issues to inform the County Council’s decisions. The Joint Crawley CLC hosted meeting was the last of 13 public meetings hosted by the County Local Committees across the county during September and October to consider the PCT’s consultation. ‘Fit for the Future’ (FFF) proposals contained many positive aspects, including bringing many services closer to people and communities. -

Serving Crawley in Worth, Pound Hill, Maidenbower and Forge Wood
Serving Crawley in Worth, Pound Hill, Maidenbower and Forge Wood Rector Fr Michael Boag [email protected] 01293 882229 Associate Vicar Revd Sarah Upchurch [email protected] 01293 524804 Revd Canon Roger Brown 01293 520454 Assistant Priests Revd Gordon Parry 07802 432398 Our regular services are shown below; a calendar at the back of this magazine details special services, groups and events happening throughout the next two months. ’, ’, Sundays 08.00 Holy Communion 10.00 1st,, 2nd, and 3rd Sundays - (Book of Common Prayer, 1662) Eucharist and Sunday School 10.00 Sung Eucharist 10.00 4th Sundays (Common Worship) Child- friendly Eucharist Tuesdays 10.30 Eucharist 15:00 Messy Church at St Barnabas’ Wednesdays 26 June, 17 July and 25 September Thursdays 10.30 Eucharist You can also join us at: 12 June, 10, July and 11 Sept 15:15 Messy Church in Maidenbower And here’s what’s happening in the café each week: ‘ Tuesdays 10.30 - 12.00 Pop in for a cake and a drink Thursdays 14.00 - 16.00 Knit and Natter -bring any crafts to do Fridays 10.30 - 12.30 Pop in for a cake and a drink 12.30 Lunches – please prebook tickets (£6.50) by calling 0300 111 8150 Saturdays 10.30 - 12.00 Pop in for a cake and a drink. Market on the first Saturday each month You can also find up to date information here: If you have a Baptism, Wedding or general enquiry, please call the office on 0300 111 8150 or email [email protected] To contact Fr. -

The Bright Company-2
ALL THE BRIGHT COMPANY OF HEAVEN ALL THE BRIGHT COMPANY OF HEAVEN Renny Richardson Menin House an imprint of Tommies Guides Military Booksellers & Publishers Menin House 13 Hunloke Avenue Eastbourne East Sussex BN22 8UL www.tommiesguides.co.uk First published in Great Britain by Menin House Publishers 2011 © 2011 Renny Richardson A catalogue record for this book is available from the British Library All rights reserved. Apart from any use under UK copyright law no part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without prior written permission of the publisher, nor be otherwise circulated in any form of binding or cover other than that in which it is published and without a similar condition being imposed on the subsequent publisher. ISBN 978-1-908336-00-2 Cover design by Tommies Guides Typeset by Graham Hales Printed and bound in Great Britain by CPI Antony Rowe, Chippenham and Eastbourne CONTENTS PREFACE: REASONS . .13 FOREWORD . .15 INTRODUCTION 17 PART ONE: BUILDERS 1834-1913 . 19 PART TWO: SOLDIERS 1914 45 1915 59 1916 103 1917 . 155 1918 . 203 PART THREE: MEMORIALS 1919-1921 291 PART FOUR: ENDINGS 2010 339 DEDICATION This book is dedicated to the memory of all those men, known and unknown, of the Crawley & Ifield district who fought but in particular to the memories of:- Lieutenant (Acting Captain) Alfred Edward Cook September 29th 1867-August 11th 1938 Second Lieutenant Richard Edward Cook January 9th 1898-April 13th 1918 Private Donald Herbert Cook July 31st 1899-December 29th 1962 with love and admiration 7 All the bright company of Heaven Hold him in their high comradeship, The Dog-Star, and the Sisters Seven, Orion’s Belt and sworded hip – taken from Into Battle (Flanders, April 1915) by Julian Grenfell Not even a sparrow falls to the earth without God’s knowing of it – Matthew 10:29-31 What we do in life echoes in eternity – Ridley Scott, Gladiator. -

Crawley Clinical Commissioning Group Horsham and Mid Sussex Clinical Commissioning Group
Agenda Item No. 6b Lower Ground Floor Crawley Hospital West Green Drive Crawley West Sussex RH11 7DH Tel: 01293 600300 (ext. 4255) Email: [email protected] Dear Mr Turner and Dr Walsh, Thank you for your letter dated 13th December and the opportunity to respond. As you are aware we are committed to transforming our community services to deliver an integrated service model in collaboration with all our partners across Crawley, Horsham and Mid Sussex CCG areas. The work we have been progressing throughout 15/16 has laid the foundations for improving the preferred model of ‘home first’ principles. The current programme of work includes: • increased focus on delivering the principles of an integrated discharge team across our acute hospital sites at East Surrey Hospital and Princess Royal Hospital • developing an enhanced responsive service model that transforms the current separate community services/teams offering admission avoidance and step down from an acute admission, into a cohesive service offer across the patient pathway from proactive care, crisis intervention and maintenance with access to specialist support at each stage where the need has been identified • Working with West Sussex County Council to align and move towards an integrated joint community rehabilitation service offer that will include access to re ablement home care support • developing a local clinical navigation hub that will enable patients and professionals to access advice/support from urgent care services to meet their needs first time and avoid multiple referrals and confusing signposting We welcome the Boards recommendation for further improvements to the current level of information sharing and a shared understanding of pressures across Health and Social Care. -

Local News and What's on Village People
Local village talk, by the village Issue #6 : Apr/May 2013 Inc. Brook St, Ansty & Staplefield Free Local news and What’s On page 4 Village People: Jo cycles for charity page 14 Baptist Church ‘Contact’ included page 17 CL06 AprMay CLife.indd 1 08/04/2013 10:28 2 Local news & info on Twitter: @CuckfieldLife www.cuckfieldlife.co.uk CL06 AprMay CLife.indd 2 08/04/2013 10:28 EDITORIAL By David Tingley, Editor I have a confession to make; I had fully intended on taking part in the Cuckfield Walking Race which took place earlier in April - but I completely forgot! However, it seems that the race was certainly on - get the facts overleaf on page 4. While I talk about getting involved in village life I also want to plug the annual Cuckoo Fayre on Bank Holiday Monday 6th May. Cuckfield Life will have a stall there and we’d love to see the many familiar local faces as well as lots of new ones, so do come over and have a drink and a chat with us. More about the Fayre can be found in the Mayor’s column on page 7. If the weather has warmed up sufficiently for you to consider a recreational walk this month, do read Peter Lovett’s article on page 32. It gives a flavour and an insight into a fascinating local history-themed walk. Thanks Peter for sharing it with us. Elsewhere in the magazine we catch up with Cuckfield mum Jo Walker, who is soon to be cycling through the Sri Lanken tea plantations to raise money for a cause very close to her heart. -

Health Focus – Spring 2014
HealthIssue 6 Spring 2014 Focus Surrey and Sussex Healthcare NHS Trust 5 Health Secretary praises ‘patient centred care’ 8 Championing dementia Issue 6 - spotlight on care for the elderly Spring 2014 10 Operation recovery - tips to help you after surgery Health Focus 1 Useful information Surrey and Sussex Healthcare NHS Trust Where are we located? Disabled parking Surrey and Sussex Healthcare NHS Trust (SASH) There are dedicated parking spaces for disabled patients provides emergency and non-emergency services at: around East Surrey Hospital. There are spaces outside the new Main Entrance, in front of the East Entrance, East Surrey Hospital and adjacent to the visitor’s car park. Disabled parking Canada Avenue, Redhill, Surrey RH1 5RH in these areas is free. There are more disabled parking Telephone: 01737 768511 spaces in the visitor’s car park where the normal car park SASH provides some non-emergency services at Crawley tariff applies. Hospital which is managed by Sussex Community Trust: PALS: Patient Advice and Liaison Service at SASH Crawley Hospital West Green Drive, Crawley, West Sussex RH11 7DH As a patient, relative, carer or visitor sometimes you may Telephone: 01293 600300 need to turn to someone for confidential, on-the-spot help, advice and support. PALS will help you to sort out We also provide a number of services at four any concerns you may have about the care we provide. community sites: We can also guide you through the different services Caterham Dene Hospital available from the NHS. Church Road, Caterham, Surrey CR3 5RA Contacting PALS Telephone: 01883 837500 • telephone on 01737 231958 Dorking Hospital • email [email protected] Horsham Road, Dorking, Surrey RH4 2AA Telephone: 01306 646238 • writing to: PALS, East Surrey Hospital, Canada Avenue, Redhill, Surrey, RH1 5RH Horsham Hospital Hurst Road, Horsham, West Sussex RH12 2DR You can also ask a member of staff to contact the PALS Telephone 01403 227000 on your behalf. -

27Th April 2000
Practice Privacy Notice Your information This privacy notice explains why we collect information about you, how this data may be used and how we keep it safe and confidential. Data Controller Saxonbrook Medical Maidenbower Square Crawley RH10 7QH Data Protection Officer Crawley Clinical Commissioning Group (CCG) are in the process of appointing a designated Data Protection Officer (DPO). This notice will be updated with their details once this becomes available. Until this time, Saxonbrook Medical’s interim DPO is: Andre Bento, Practice Manager Saxonbrook Medical Maidenbower Square Crawley RH10 7QH Caldicott Guardian Dr Ian Anderson, Senior Partner Saxonbrook Medical Maidenbower Square Crawley RH10 7QH Why we collect information about you Health care professionals are required by law to maintain records about your health and any treatment or care you have received within any NHS organisation. These records help to provide you with the best possible healthcare. We collect and hold data for the sole purpose of providing healthcare services to our patients. “Saxonbrook Medical is a team of skilled people aiming to provide quality healthcare to our local communities in a welcoming environment.” Partners: Dr Ian Anderson, Dr Hicham Nakouzi Saxonbrook Medical Centre, Maidenbower Square, Maidenbower, West Sussex, RH10 7QH Tel: +44 1293 450400, Fax: +44 1293 450419, E-mail [email protected], www.saxonbrook.co.uk In carrying out this role we may collect information about you which helps us respond to your queries or secure specialist services. We may keep your information in written form and/or in digital form. The records may include basic details about you, such as your name and address. -

At Crawley Study 2009
Crawley Borough Council, Horsham District Council & Mid Sussex District Council At Crawley Study 2009 Final Report: October 2009 AT CRAWLEY STUDY 2009 CONTENTS 1. INTRODUCTION 2 2. STUDY CONTEXT 7 3. SUSTAINABILITY ASSESSMENT 13 4. DEVELOPMENT OPTIONS 19 5. SOCIAL INFRASTRUCTURE ASSESSMENT 25 6. TRANSPORT INFRASTRUCTURE ASSESSMENT 33 7. ENERGY & UTILITIES ASSESSMENT 43 8. ACHIEVABILITY 55 9. KEY FINDINGS 61 Contact: Nick Ireland, Associate Director, GL Hearn T: 020 7851 4813 E: [email protected] Page 1 of 76 AT CRAWLEY STUDY 2009 1.5 The Study is intended to ensure that future strategic development at Crawley is highly sustainable, properly planned and supported by 1. INTRODUCTION timely provision of adequate infrastructure. It aims to ensure that future strategic development is of a high quality and supports the town as a 1.1 This Study examines the potential for strategic development ‘at whole. Crawley.’ It explores the potential to bring forward strategic development, including a new neighbourhood and/ or strategic Objectives employment, in the period to 2026. It assesses the suitability of a number of potential locations for development in line with sustainable 1.6 The Study Area comprises areas contiguous to Crawley’s Built-up development principles, together with the availability of sites and their Area Boundary. It includes land which falls within the boundaries of deliverability. This includes an assessment of social, energy, utilities Crawley Borough together with Horsham and Mid Sussex Districts in and transport infrastructure necessary to support strategic West Sussex. development. 1.7 The Study area together with the site ‘options’ considered previously 1.2 The Study has been undertaken by a multi-disciplinary team of as part of the 2005 ‘Atkins’ Study are shown in Figure 1.1. -

Crawley-Borough-Council-Cycle-Map
C L U Langshott RS M E L 21 H E L I Y RO Infant School LL ON YOUR BIKE AD O A S R D EN CYCLE CRAWLEY QUE KEY People driving cars typically look for other vehicles and may Manorfield Primary Oakwood Library Crawley is fairly flat and cycle facilities make cycling and Nursery School School Advisory cycle route not notice you on your bike, even when you are in front of even easier and safer. With panniers or a trailer, a lot Cycle lane on road them. Make sure you are seen by positioning yourself well map of shopping can be done by bike. Many trips are short Cycle track off road in view – the ‘primary’ position is about one metre from the Cyycle enough to go easily by bike, often more quickly than kerb – and observing where drivers are looking when you Walkway craawleyw by car. Cycle parking is free, readily available and you Police want to turn. Station Footpath can stop and walk at any time. Bridleway Think carefully about overtaking on the inside, even when Cycling: vehicles are stationary. Be aware that lorry and bus drivers 21 National Cycle Network VICTORIA ROAD cannot see you there. l Is quick and direct HOOKWOOD route number cycling, l Avoids traffic jams 21 Horley Toucan crossing On shared paths, a sudden appearance of a bike can be an Superstore E IV R D unpleasant shock for a pedestrian, particularly for people l Helps keep you fit Cycle parkingS EN with visual or hearing impairment, even if you allow enough l Saves money Spire Gatwick UE Bus stop VEN pedestrian and Park Hospital ES A space. -

Horsham and Mid Sussex Clinical Commissioning Group Lower Ground Floor Crawley Hospital West Green Drive Crawley West Sussex RH11 7DH Tel: 01293 600300 (Ext
Horsham and Mid Sussex Clinical Commissioning Group Lower Ground Floor Crawley Hospital West Green Drive Crawley West Sussex RH11 7DH Tel: 01293 600300 (ext. 4255) Email: [email protected] Website: www.horshamandmidsussexccg.nhs.uk 17 June 2019 Dear Colleague, Horsham and Mid Sussex CCG – Annual General Meeting and Market Place 2019 On behalf of the Governing Body, I would like to invite you to our Annual General Meeting (AGM), which will be held on 18 July, 11.30am – 12.30pm, at Clair Hall, Perrymount Road, Haywards Heath RH16 3DN. We will be holding a “market place” event after the AGM (12.30pm – 1.30pm) in order to showcase some of our key areas of work over the past year. This will also include details of some of the engagement we have been carrying out over the past few months under our “Our health and care, our FUTURE” programme. You will be able to meet our teams, find out more about the plans for health services locally and across the Sussex area. 2018-19 was a difficult and challenging year for the CCG but it was also a year of achievement, with progress in terms of governance, capability and capacity of the organisation. The AGM will be an opportunity to look back on our achievements and challenges, as well as look at how we are working now and our plans for the future. Our Annual Report 2018/19 sets out in more detail the CCG’s work over the last 12 months, and will be formally presented at the AGM. -
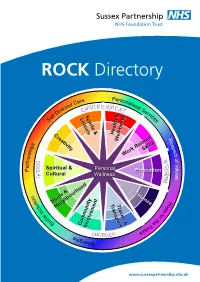
ROCK Directory
ROCK Directory re Perso Ca nal ed ise ct d S ire e D rv lf Sports & ic e Leisure e S s Creativity Health & R Well-being Well-being e s s p p i Skills e h c s t r Work Related o e f n t V r a a l Spiritual & Personal u P Personal Education e Cultural WellnessWellness s FinanceFinance n o H i s Home & o u TransportTransportTravelTravel && p l c Neighbourhood e n I f o l r a i t h c e o S F Community u t InvolvementInvolvement u r e s h t g n e r t S www.sussexpartnership.nhs.uk Contents Health and wellbeing ................................... 3 Work related skills .......................................... 54 Education ........................................................ 78 Finance ............................................................. 91 Travel and transport ...................................... 101 Community involvement ............................ 112 Home and neighbourhood ........................ 139 Spiritual and cultural ..................................... 162 Creativity .......................................................... 178 Sport and leisure ............................................ 188 re Perso Ca nal ed ise ct d S ire e D rv lf Sports & ic e Leisure e S s Creativity Health & R Well-being Well-being e s s p p i Skills e h c s t r Work Related o e f n t V r a a l Spiritual & Personal u P Personal Education e Cultural Wellness s Finance n o H i s Home & o u TransportTransportTravelTravel && p l c Neighbourhood e n I f o l r a i t h c e o S F Community u t InvolvementInvolvement u r e s h t g n e r t S 2 Health and wellbeing 3 Health and wellbeing Green Gym Stanmer BTCV Office, Stanmer Park, Lewes Road, Brighton BN1 9SE Telephone: 01273 691207 Mobile: 07740 899 709 Email: [email protected] www.btcv.org Services A unique scheme where you can become both physically and mentally healthier by taking part in conservation activities, based in Stanmer Park.