Review of the National Program for Onchocerciasis Control in the Democratic Republic of the Congo
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Country Sheet Democratic Republic of Congo (Drc)
The Country of Return Information Project functions as a network of NGOs for the collection and transfer of specific information on reintegration possibilities for potential returnees and their counsellor. All questions you may have on reintegration possibilities and on which you don’t find the answer in this country sheet can be directed to the helpdesk: “Country of Return Information and Vulnerable Groups”. E-mail: [email protected] COUNTRY SHEET DEMOCRATIC REPUBLIC OF CONGO (DRC) The Country of Return Information Project and Vulnerable Groups runs until June 2009 and is funded by the European Community. The European Commission is not responsible for any use that JUNE 09 may be made of the information provided. Sole responsibility for its content lies with the author. 1 DISCLAIMER This Country Sheet is for informational purposes only and no rights can be derived from its contents. The CRI-partners will do their utmost to include accurate, corroborated, transparent and up-to-date information, but make no warrants as to its accuracy or completeness. Consequently, the CRI-partners do not accept responsibility in any way for the information in this Country Sheet and accept no liability for damages of any kind arising from using the information in this Country Sheet. The information in this Country Sheet has been retrieved in collaboration with local partners. This Country Sheet contains links to websites that are created and maintained by other organizations. The CRI-project does not take any responsibility for the content of these websites. The CRI-partners are the partners who participate fully in the CRI-project: Vluchtelingenwerk Vlaanderen, Asociación Comissión Católica Española de Migración, Caritas International Belgium, Consiglio Italiano Per I Rifugiati, Coordination et Initiatives pour les Réfugiés et Étrangers and Dansk Flygtningehjælp. -
Tangled! Congolese Provincial Elites in a Web of Patronage
Researching livelihoods and services affected by conflict Tangled! Congolese provincial elites in a web of patronage Working paper 64 Lisa Jené and Pierre Englebert January 2019 Written by Lisa Jené and Pierre Englebert SLRC publications present information, analysis and key policy recommendations on issues relating to livelihoods, basic services and social protection in conflict-affected situations. This and other SLRC publications are available from www.securelivelihoods.org. Funded by UK aid from the UK Government, Irish Aid and the EC. Disclaimer: The views presented in this publication are those of the author(s) and do not necessarily reflect the UK Government’s official policies or represent the views of Irish Aid, the EC, SLRC or our partners. ©SLRC 2018. Readers are encouraged to quote or reproduce material from SLRC for their own publications. As copyright holder SLRC requests due acknowledgement. Secure Livelihoods Research Consortium Overseas Development Institute (ODI) 203 Blackfriars Road London SE1 8NJ United Kingdom T +44 (0)20 3817 0031 F +44 (0)20 7922 0399 E [email protected] www.securelivelihoods.org @SLRCtweet Cover photo: Provincial Assembly, Lualaba. Lisa Jené, 2018 (CC BY-NC-ND 2.0). B About us The Secure Livelihoods Research Consortium (SLRC) is a global research programme exploring basic services, livelihoods and social protection in fragile and conflict-affected situations. Funded by UK Aid from the UK Government’s Department for International Development (DFID), with complementary funding from Irish Aid and the European Commission (EC), SLRC was established in 2011 with the aim of strengthening the evidence base and informing policy and practice around livelihoods and services in conflict. -

Democratic Republic of Congo Constitution
THE CONSTITUTION OF THE DEMOCRATIC REPUBLIC OF THE CONGO, 2005 [1] Table of Contents PREAMBLE TITLE I GENERAL PROVISIONS Chapter 1 The State and Sovereignty Chapter 2 Nationality TITLE II HUMAN RIGHTS, FUNDAMENTAL LIBERTIES AND THE DUTIES OF THE CITIZEN AND THE STATE Chapter 1 Civil and Political Rights Chapter 2 Economic, Social and Cultural Rights Chapter 3 Collective Rights Chapter 4 The Duties of the Citizen TITLE III THE ORGANIZATION AND THE EXERCISE OF POWER Chapter 1 The Institutions of the Republic TITLE IV THE PROVINCES Chapter 1 The Provincial Institutions Chapter 2 The Distribution of Competences Between the Central Authority and the Provinces Chapter 3 Customary Authority TITLE V THE ECONOMIC AND SOCIAL COUNCIL TITLE VI DEMOCRACY-SUPPORTING INSTITUTIONS Chapter 1 The Independent National Electoral Commission Chapter 2 The High Council for Audiovisual Media and Communication TITLE VII INTERNATIONAL TREATIES AND AGREEMENTS TITLE VIII THE REVISION OF THE CONSTITUTION TITLE IX TRANSITORY AND FINAL PROVISIONS PREAMBLE We, the Congolese People, United by destiny and history around the noble ideas of liberty, fraternity, solidarity, justice, peace and work; Driven by our common will to build in the heart of Africa a State under the rule of law and a powerful and prosperous Nation based on a real political, economic, social and cultural democracy; Considering that injustice and its corollaries, impunity, nepotism, regionalism, tribalism, clan rule and patronage are, due to their manifold vices, at the origin of the general decline -

With Effect from 1 April 2012 Through 30 June 2012
List of locations where payment of danger pay has been approved' with effect from 1 April 2012 through 30 June 2012: AFGHANISTAN CONGO, DEMOCRATIC REPUBLIC OF - North Kivu Province, South Kivu Province, Orientale Province - (only Bas Uele, Haut Uele and Ituri Districts), Maniema Province ETHIOPIA - Somali Region IRAQ - Entire country except Erbil KENYA - North Eastern Province (Garissa, Dadaab, Mandera, Wajir, Ijara) LEBANON - South Lebanon (UNIFIL Area of Operations, except the Tyre pocket) PAKISTAN - Balochistan Province, Khyber Pakhtunkhawa Province (formerly, North-West Frontier Province) and Federally Administrated Tribal Areas SOMALIA SOUTH SUDAN - Unity State, Upper Nile State, Jonglei State, Warrap State (except Tonji South county), in Lakes State (only Awerial, Yirol East, Rumbek Centre, Rumbek North and Rumbek East counties), in Northern Bar El Gazal State (only Aweil East and Aweil North counties), in Western Bar El Gazal State (all locations north of the road Kafia-Gabir-Kosho-Raja, excluding Raga town), Western Equatoria (only all locations south of the road Morobo-Yei-Maridi- Yambio-Nadi-Tambura, except Yambio town) SUDAN - the Darfurs (West, South and North Darfur), Abyei Administered Area, South Kordofan State and Blue Nile State SYRIA ARAB REPUBLIC - Entire country except Damascus (city boundaries) and UNDOF Area of Operations • YEMEN Addendum Please note that in addition to the approved locations above, on 3 July 2012, Danger Pay was also approved for the location below with retroactive effective date of 1 to 30 June 2012: ® Damascus, Syria. -

Republique Democratique Du Congo
ETUDE DE L’IMPACT DES ARTS, DE LA CULTURE ET DES INDUSTRIES CREATIVES SUR L’ ECONOMIE EN AFRIQUE REPUBLIQUE DEMOCRATIQUE DU CONGO Projet développé et exécuté par Agoralumiere en collaboration avec CAJ(Afrique du Sud) commandé par ARTerial Network et financé par la Foundation DOEN , la Foundation Stomme et la République Fédérale du Nigeria Ministry of Commerce and Industry Federal Republic of Nigeria Democratic Republic of Congo Africa Union www.creative-africa.org Agoralumiere 2009 Remerciements Cette étude pilote a été commandée par ARTERIAL NETWORK et conjointement financée par STICHTING DOEN, la Fondation STROMME et le Gouvernement de la République Fédérale du Nigeria. Agoralumiere a été soutenue par l’Union Africaine pour la conduite de ce travail de recherche pilote dans le cadre de la mise en œuvre du Plan d’Action des Industries Culturelles et Créatives reformulé par Agoralumiere à la demande de la Commission et qui fut adopté en octobre 2008 par les Ministres de la Culture de l’Union Africaine. Agoralumiere a aussi été soutenue par le gouvernement de la République Démocratique du Congo, et particulièrement par le Cabinet du Premier Ministre qui entend utiliser ce travail de base pour élaborer une suite plus approfondie au niveau national, avec des chercheurs nationaux déjà formés dans le secteur. Agoralumiere a enfin été soutenue par le Dr Bamanga Tukur, Président du African Business Roundtable et du NEPAD Business Group. Agoralumiere tient à remercier tous ceux dont la participation directe et la contribution indirecte ont appuyé -

Deforestation and Forest Degradation Activities in the DRC
E4838 V5 DEMOCRATIC REPUBLIC OF THE CONGO MINISTRY FOR THE ENVIRONMENT, NATURE CONSERVATION AND TOURISM Public Disclosure Authorized STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS Public Disclosure Authorized BASELINE REPORT STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ Public Disclosure Authorized PROCESS Public Disclosure Authorized October 2014 STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS in the DRC INDEX OF REPORTS Environmental Analysis Document Assessment of Risks and Challenges REDD+ National Strategy of the DRC Strategic Environmental and Social Assessment Report (SESA) Framework Document Environmental and Social Management Framework (ESMF) O.P. 4.01, 4.04, 4.37 Policies and Sector Planning Documents Pest and Pesticide Cultural Heritage Indigenous Peoples Process Framework Management Management Planning Framework (FF) Resettlement Framework Framework (IPPF) O.P.4.12 Policy Framework (PPMF) (CHMF) O.P.4.10 (RPF) O.P.4.09 O.P 4.11 O.P. 4.12 Consultation Reports Survey Report Provincial Consultation Report National Consultation of June 2013 Report Reference and Analysis Documents REDD+ National Strategy Framework of the DRC Terms of Reference of the SESA October 2014 Strategic Environmental and Social Assessment SESA Report TABLE OF CONTENTS Introductory Note ........................................................................................................................................ 9 1. Preface ............................................................................................................................................ -

Mai-Ndombe Province: a REDD+ Laboratory in the Democratic Republic of the Congo
RIGHTS AND RESOURCES INITIATIVE | MARCH 2018 Rights and Resources Initiative 2715 M Street NW, Suite 300 Washington, DC 20007 P : +1 202.470.3900 | F : +1 202.944.3315 www.rightsandresources.org About the Rights and Resources Initiative RRI is a global coalition consisting of 15 Partners, 7 Affiliated Networks, 14 International Fellows, and more than 150 collaborating international, regional, and community organizations dedicated to advancing the forestland and resource rights of Indigenous Peoples and local communities. RRI leverages the capacity and expertise of coalition members to promote secure local land and resource rights and catalyze progressive policy and market reforms. RRI is coordinated by the Rights and Resources Group, a non-profit organization based in Washington, DC. For more information, please visit www.rightsandresources.org. Partners Affiliated Networks Sponsors The views presented here are not necessarily shared by the agencies that have generously supported this work, or all of the Partners and Affiliated Networks of the RRI Coalition. This work is licensed under a Creative Commons Attribution License CC BY 4.0. – 2 – Contents Acknowledgements ............................................................................................................................................ 4 Acronyms ............................................................................................................................................................. 5 Executive summary ........................................................................................................................................... -
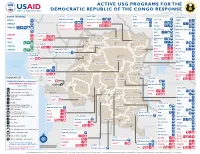
ACTIVE USG PROGRAMS for the DEMOCRATIC REPUBLIC of the CONGO RESPONSE Last Updated 07/27/20
ACTIVE USG PROGRAMS FOR THE DEMOCRATIC REPUBLIC OF THE CONGO RESPONSE Last Updated 07/27/20 BAS-UELE HAUT-UELE ITURI S O U T H S U D A N COUNTRYWIDE NORTH KIVU OCHA IMA World Health Samaritan’s Purse AIRD Internews CARE C.A.R. Samaritan’s Purse Samaritan’s Purse IMA World Health IOM UNHAS CAMEROON DCA ACTED WFP INSO Medair FHI 360 UNICEF Samaritan’s Purse Mercy Corps IMA World Health NRC NORD-UBANGI IMC UNICEF Gbadolite Oxfam ACTED INSO NORD-UBANGI Samaritan’s WFP WFP Gemena BAS-UELE Internews HAUT-UELE Purse ICRC Buta SCF IOM SUD-UBANGI SUD-UBANGI UNHAS MONGALA Isiro Tearfund IRC WFP Lisala ACF Medair UNHCR MONGALA ITURI U Bunia Mercy Corps Mercy Corps IMA World Health G A EQUATEUR Samaritan’s NRC EQUATEUR Kisangani N Purse WFP D WFPaa Oxfam Boende A REPUBLIC OF Mbandaka TSHOPO Samaritan’s ATLANTIC NORTH GABON THE CONGO TSHUAPA Purse TSHOPO KIVU Lake OCEAN Tearfund IMA World Health Goma Victoria Inongo WHH Samaritan’s Purse RWANDA Mercy Corps BURUNDI Samaritan’s Purse MAI-NDOMBE Kindu Bukavu Samaritan’s Purse PROGRAM KEY KINSHASA SOUTH MANIEMA SANKURU MANIEMA KIVU WFP USAID/BHA Non-Food Assistance* WFP ACTED USAID/BHA Food Assistance** SA ! A IMA World Health TA N Z A N I A Kinshasa SH State/PRM KIN KASAÏ Lusambo KWILU Oxfam Kenge TANGANYIKA Agriculture and Food Security KONGO CENTRAL Kananga ACTED CRS Cash Transfers For Food Matadi LOMAMI Kalemie KASAÏ- Kabinda WFP Concern Economic Recovery and Market Tshikapa ORIENTAL Systems KWANGO Mbuji T IMA World Health KWANGO Mayi TANGANYIKA a KASAÏ- n Food Vouchers g WFP a n IMC CENTRAL y i k -
A Life of Fear and Flight
A LIFE OF FEAR AND FLIGHT The Legacy of LRA Brutality in North-East Democratic Republic of the Congo We fled Gilima in 2009, as the LRA started attacking there. From there we fled to Bangadi, but we were confronted with the same problem, as the LRA was attacking us. We fled from there to Niangara. Because of insecurity we fled to Baga. In an attack there, two of my children were killed, and one was kidnapped. He is still gone. Two family members of my husband were killed. We then fled to Dungu, where we arrived in July 2010. On the way, we were abused too much by the soldiers. We were abused because the child of my brother does not understand Lingala, only Bazande. They were therefore claiming we were LRA spies! We had to pay too much for this. We lost most of our possessions. Once in Dungu, we were first sleeping under a tree. Then someone offered his hut. It was too small with all the kids, we slept with twelve in one hut. We then got another offer, to sleep in a house at a church. The house was, however, collapsing and the owner chased us. He did not want us there. We then heard that some displaced had started a camp, and that we could get a plot there. When we had settled there, it turned out we had settled outside of the borders of the camp, and we were forced to leave. All the time, we could not dig and we had no access to food. -

Drc): Case Studies from Katanga, Ituri and Kivu
CONFLICT BETWEEN INDUSTRIAL AND ARTISANAL MINING IN THE DEMOCRATIC REPUBLIC OF CONGO (DRC): CASE STUDIES FROM KATANGA, ITURI AND KIVU Ruben de Koning Introduction The mining sector in the Democratic Republic of Congo (DRC) is widely regarded as the key engine for post-conflict reconstruction. To attract for- eign investment, the government in 2002 enacted a new mining code that makes it easier for foreign companies to obtain industrial mining titles. Within a few years exploration concessions covered about a third of the country. Meanwhile, exploitation rights to the most important proven deposits were converted to new joint-ventures between foreign investors and Congolese state mining companies. The rapid attribution of min- ing titles has, however, not lead to a resumption of industrial mining on the scale the central government and its foreign donors had hoped for. Apart from a few copper and cobalt mines in the southern Katanga prov- ince, mineral production in the rest of the country, but also in Katanga, remains largely artisanal. Artisanal mining employs up to two million people across the country and largely takes place on concessions where industrial mining is supposed happen (Wold Bank 2009). In many of these artisanal mining areas and particularly in the eastern DRC state functions have almost completely eroded during two consecutive civil wars. Arti- sanal miners often work in dangerous conditions and are forced to pay numerous illegal taxes or to work for the military and rebel forces that control mines. At the same time, the local power complexes that emerged around artisanal mining operations have withheld large scale industrial investment, thereby preventing displacement of artisanal miners from concessions. -

La Ville De Kinshasa
« Kin la belle… – et Kin la poubelle» La ville de Kinshasa Suite à la dégradation économique et plu- En 1881, Henry sieurs vagues de pilla- Morton Stanley ges, les anciens quar- fonde le poste tiers de l’élite (la Léopoldville, Gombe, Ma Campa- nommé après gne à Ngaliema et par le Roi des quelques parties de Belges, colonisa- Limete) sont aujourd’hui d’un charme plutôt morbide. teur du Congo. L’endroit est spacieux et facile à défen- La réhabilitation des routes demeure un défi majeur. dre, ils existent plusieurs villages autochtones sur le Le personnel de la mission EUPOL RD Congo à Kinshasa, Dans les cités, des tornades de pluie font écouler des site. Léopoldville devient centre administratif du octobre 2008. maisons pendant chaque saison de pluie. Congo-Belge en 1929 (avant, c’était la ville de Boma « Kinshasa – the beauty and the beast »: Due to the de- sur la côte atlantique). La capitale devient Kinshasa en gradation of the economic situation and several lootings, 1966. / I n 1881, Henry Morton Stanley founds Leopold- EUPOL RDC et EUSEC RDC, ville, a settlement named after the Belgian King, owner the ancient elite’s quarters of Gombe, Ma Campagne in les deux missions PESD Ngaliema and some parts of Limete show nowadays a of the colony. The site is vast and easy to defend; there rather morbid charme. Rehabilitating Kinshasa’s roads en République Démocratique du Congo, are already several villages of natives in the area. Leo- rests a major challenge for the city’s development. In the vous souhaitent un bon séjour poldville is named administrative center of the Belgian- popular quarters, violent rain downpours bring down à Kinshasa. -

Democratic Republic of the Congo of the Congo Democratic Republic
Democratic Republic of the Congo of the Congo Democratic Republic Main objectives Impact • UNHCR provided international protection to some In 2005, UNHCR aimed to strengthen the protection 204,300 refugees in the DRC of whom some 15,200 framework through national capacity building, registra- received humanitarian assistance. tion, and the prevention of and response to sexual and • Some of the 22,400 refugees hosted by the DRC gender-based violence; facilitate the voluntary repatria- were repatriated to their home countries (Angola, tion of Angolan, Burundian, Rwandan, Ugandan and Rwanda and Burundi). Sudanese refugees; provide basic assistance to and • Some 38,900 DRC Congolese refugees returned to locally integrate refugee groups that opt to remain in the the DRC, including 14,500 under UNHCR auspices. Democratic Republic of the Congo (DRC); prepare and UNHCR monitored the situation of at least 32,000 of organize the return and reintegration of DRC Congolese these returnees. refugees into their areas of origin; and support initiatives • With the help of the local authorities, UNHCR con- for demobilization, disarmament, repatriation, reintegra- ducted verification exercises in several refugee tion and resettlement (DDRRR) and the Multi-Country locations, which allowed UNHCR to revise its esti- Demobilization and Reintegration Programme (MDRP) mates of the beneficiary population. in cooperation with the UN peacekeeping mission, • UNHCR continued to assist the National Commission UNDP and the World Bank. for Refugees (CNR) in maintaining its advocacy role, urging local authorities to respect refugee rights. UNHCR Global Report 2005 123 Working environment Recurrent security threats in some regions have put another strain on this situation.