Report of a WHO Informal Consultation on Sustainable Control of Human African Trypanosomiasis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Country Sheet Democratic Republic of Congo (Drc)
The Country of Return Information Project functions as a network of NGOs for the collection and transfer of specific information on reintegration possibilities for potential returnees and their counsellor. All questions you may have on reintegration possibilities and on which you don’t find the answer in this country sheet can be directed to the helpdesk: “Country of Return Information and Vulnerable Groups”. E-mail: [email protected] COUNTRY SHEET DEMOCRATIC REPUBLIC OF CONGO (DRC) The Country of Return Information Project and Vulnerable Groups runs until June 2009 and is funded by the European Community. The European Commission is not responsible for any use that JUNE 09 may be made of the information provided. Sole responsibility for its content lies with the author. 1 DISCLAIMER This Country Sheet is for informational purposes only and no rights can be derived from its contents. The CRI-partners will do their utmost to include accurate, corroborated, transparent and up-to-date information, but make no warrants as to its accuracy or completeness. Consequently, the CRI-partners do not accept responsibility in any way for the information in this Country Sheet and accept no liability for damages of any kind arising from using the information in this Country Sheet. The information in this Country Sheet has been retrieved in collaboration with local partners. This Country Sheet contains links to websites that are created and maintained by other organizations. The CRI-project does not take any responsibility for the content of these websites. The CRI-partners are the partners who participate fully in the CRI-project: Vluchtelingenwerk Vlaanderen, Asociación Comissión Católica Española de Migración, Caritas International Belgium, Consiglio Italiano Per I Rifugiati, Coordination et Initiatives pour les Réfugiés et Étrangers and Dansk Flygtningehjælp. -

Portuguese Language in Angola: Luso-Creoles' Missing Link? John M
Portuguese language in Angola: luso-creoles' missing link? John M. Lipski {presented at annual meeting of the AATSP, San Diego, August 9, 1995} 0. Introduction Portuguese explorers first reached the Congo Basin in the late 15th century, beginning a linguistic and cultural presence that in some regions was to last for 500 years. In other areas of Africa, Portuguese-based creoles rapidly developed, while for several centuries pidginized Portuguese was a major lingua franca for the Atlantic slave trade, and has been implicated in the formation of many Afro- American creoles. The original Portuguese presence in southwestern Africa was confined to limited missionary activity, and to slave trading in coastal depots, but in the late 19th century, Portugal reentered the Congo-Angola region as a colonial power, committed to establishing permanent European settlements in Africa, and to Europeanizing the native African population. In the intervening centuries, Angola and the Portuguese Congo were the source of thousands of slaves sent to the Americas, whose language and culture profoundly influenced Latin American varieties of Portuguese and Spanish. Despite the key position of the Congo-Angola region for Ibero-American linguistic development, little is known of the continuing use of the Portuguese language by Africans in Congo-Angola during most of the five centuries in question. Only in recent years has some attention been directed to the Portuguese language spoken non-natively but extensively in Angola and Mozambique (Gonçalves 1983). In Angola, the urban second-language varieties of Portuguese, especially as spoken in the squatter communities of Luanda, have been referred to as Musseque Portuguese, a name derived from the KiMbundu term used to designate the shantytowns themselves. -

Hybridization Between the Megasubspecies Cailliautii and Permista of the Green-Backed Woodpecker, Campethera Cailliautii
Le Gerfaut 77: 187–204 (1987) HYBRIDIZATION BETWEEN THE MEGASUBSPECIES CAILLIAUTII AND PERMISTA OF THE GREEN-BACKED WOODPECKER, CAMPETHERA CAILLIAUTII Alexandre Prigogine The two woodpeckers, Campethera cailliautii (with races nyansae, “fuel leborni”, loveridgei) and C. permista (with races togoensis, kaffensis) were long regarded as distinct species (Sclater, 1924; Chapin 1939). They are quite dissimi lar: permista has a plain green mantle and barred underparts, while cailliautii is characterized by clear spots on the upper side and black spots on the underpart. The possibility that they would be conspecific was however considered by van Someren in 1944. Later, van Someren and van Someren (1949) found that speci mens of C. permista collected in the Bwamba Forest tended strongly toward C. cailliautii nyansae and suggested again that permista and cailliautii may be con specific. Chapin (1952) formally treated permista as a subspecies of C. cailliautii, noting two intermediates from the region of Kasongo and Katombe, Zaire, and referring to a correspondence of Schouteden who confirmed the presence of other intermediates from Kasai in the collection of the MRAC (see Annex 2). Hall (1960) reported two intermediates from the Luau River and from near Vila Luso, Angola. Traylor (1963) noted intermediates from eastern Lunda. Pinto (1983) mentioned seven intermediates from Dundo, Mwaoka, Lake Carumbo and Cafunfo (Luango). Thus the contact zone between permista and nyansae extends from the region north-west of Lake Tanganyika to Angola, crossing Kasai, in Zaire. A second, shorter, contact zone may exist near the eastern border of Zaire, not far from the Equator. The map published by Short and Tarbaton (in Snow 1978) shows cailliautii from the Semliki Valley, on the Equator but I know of no speci mens of this woodpecker from this region. -

The Luanda to Ambaca Railway As a Pioneer Case of the Transfer of Technical Engineering Knowledge Overseas to Africa
The Luanda to Ambaca Railway as a pioneer case of the transfer of technical engineering knowledge overseas to Africa. Bruno J. Navarro Interuniversity Center of Science History and Technology On 31 October 1886, three years after construction work had started on the Tua Line, the official launch ceremony was held for the Luanda-Ambaca railway, the first inland railway that the Portuguese state planned in its vast overseas space. It was the culmination of a long process of reorganization of the Portuguese colonial empire, marked out between the independence of Brazil and the defining of an agenda for the promotion of the African provinces, due to the urgent necessity to promote effective occupation of those territories, just as they had been imposed, by the major European powers at the 1885 Berlin Conference. To politicians and especially the professional class of Portuguese engineers, the railway emerged as a prodigious symbol of modernity and development, an indispensible tool for strategic territorial ownership (of a region where lines of communication were practically inexistent). It was as well directed to its population, a systematic implementation of the Portuguese state’s administrative machinery, economic use of natural resources – in domestic and foreign trade – , agricultural and industrial revitalization, and above all, the affirmation of Portugal (a small country in peripheral Europe, but in the political center in extensive colonial rule) in the community of nations that disputed influence and power in Africa. The first stretch, with a distance of 45 km linking Luanda to Funda, was open to exploitation on 1 November 1888. The connection to Ambaca appeared to be, in the spirit of its ambitious mentors, the first stage (353 km) of a more extensive project, whose ultimate goal would be the link to the opposite shore of the continent in Mozambique, in the Zambezi region. -

Liste Des Contribuables Déclarés Introuvables Par Le CDI KIN Et Transférés Dans Les CIS
Liste des contribuables déclarés introuvables par le CDI KIN et transférés dans les CIS FORME N° NIF Raison Sociale Sigle Adresse SECTEUR ACTIVITE ETAT SOCIETE SERVICE GESTIONNAIRE JURIDIQUE AV. COL Télécom. et nouvelles 1 A1418699R PM 2ÈME OEIL YA COMMUNICATION SARL INTROUVABLE CIS / NGALIEMA MONDJIBA technologies d'information 2ID CONSULTING ( INGENIERIE DE L'INFORMATION ET DU 2ID AV.N°157 DE LA Prestation de services et travaux 2 A1611866R PM INTROUVABLE CIS / GOMBE DECISIONNEL ) SARL CONSULTING VALLEE N°72 immobiliers SARL BLVD.C/GOMBE DU 30 Commerce Général et Import- 3 A1515021U PM 3RD YES SARL INTROUVABLE CIS / GOMBE JUIN N°10 IMM. Export AV.GALERIE LOKOLELA Commerce Général et Import- 4 A1302545G PM 7 SARL INTROUVABLE CIS / KINSHASA N°112 Export AV.C/KINSHASA EQUATEUR Commerce Général et Import- 5 A0708987C PM A.M. YOZMA SPRL A.M.YO. INTROUVABLE CIS / GOMBE N°749 Export AV.C/GOMBE SERGENT Prestation de services et travaux 6 A1401591W PM A.S.B GROUP S.A.R.L INTROUVABLE CIS / NGALIEMA MOKE N°14 immobiliers ETS CONGO 4C/NGALIEMA EME N°230/B 7 A1007700G PP ABBAS BACHROUCH "ETS CONGO BRIQUES" Industie INTROUVABLE CIS / LIMETE BRIQUES Q/INDUSTRIEL AV.KINGABUAC/LIMETE 8 A1301215L PP ABBAS GHANEM Autres INTROUVABLE CIS / LIMETE N° 3717 AV.C/LIMETE Commerce Général et Import- 9 A1504836Z PM ABD GROUP CONGO SARL A.G.C SARL INTROUVABLE CIS / MASINA AMBASSADEUR Export BLVDN°06 Q/SANS Commerce Général et Import- 10 A0714176S PP ABDOUL HASSAN ''ETS FISH & MEAT'' * INTROUVABLE CIS / LIMETE LUMUMBA N° Export AV.198605 TSHUAPA 1ère Agriculture et exploitation 11 A0905544M PP ABDOULAY ABASA INTROUVABLE CIS / KINSHASA Q/MADIMBA forestière AV.C/KINSHASA AVENIR Commerce Général et Import- 12 A1520272C PM ABIKIZ SARL INTROUVABLE CIS / KINTAMBO N°12 Export AV.CONCESSION EQUATEUR Commerce Général et Import- 13 A0803244L PM ABNER CONGO DIAMOND SPRL A.C.D SPRL INTROUVABLE CIS / GOMBE N° 24 C/ Export AV.GOMBE COL V/KINEBEYA Prestation de services et travaux 14 A1214486K PP ACHRAF ALI ALACHKAR INTROUVABLE CIS / GOMBE N°76 C/GOMBE immobiliers BLVD. -

2.3 Angola Road Network
2.3 Angola Road Network Distance Matrix Travel Time Matrix Road Security Weighbridges and Axle Load Limits For more information on government contact details, please see the following link: 4.1 Government Contact List. Page 1 Page 2 Distance Matrix Uige – River Nzadi bridge 18 m-long and 4 m-wide near the locality of Kitela, north of Songo municipality destroyed during civil war and currently under rehabilitation (news 7/10/2016). Road Details Luanda The Government/MPLA is committed to build 1,100 km of roads in addition to 2,834 km of roads built in 2016 and planned rehabilitation of 7,083 km of roads in addition to 10,219 km rehabilitated in 2016. The Government goals will have also the support from the credit line of the R. of China which will benefit inter-municipality links in Luanda, Uige, Malanje, Cuanza Norte, Cuanza Sul, Benguela, Huambo and Bié provinces. For more information please vitsit the Website of the Ministry of Construction. Zaire Luvo bridge reopened to trucks as of 15/11/2017, this bridge links the municipality of Mbanza Congo with RDC and was closed for 30 days after rehabilitation. Three of the 60 km between MCongo/Luvo require repairs as of 17/11/2017. For more information please visit the Website of Agencia Angola Press. Works of rehabilitation on the road nr, 120 between Mbanza Congo (province Zaire) and the locality of Lukunga (province of Uige) of a distance of 111 km are 60% completed as of 29/9/2017. For more information please visit the Website of Agencia Angola Press. -

La Ville De Kinshasa
« Kin la belle… – et Kin la poubelle» La ville de Kinshasa Suite à la dégradation économique et plu- En 1881, Henry sieurs vagues de pilla- Morton Stanley ges, les anciens quar- fonde le poste tiers de l’élite (la Léopoldville, Gombe, Ma Campa- nommé après gne à Ngaliema et par le Roi des quelques parties de Belges, colonisa- Limete) sont aujourd’hui d’un charme plutôt morbide. teur du Congo. L’endroit est spacieux et facile à défen- La réhabilitation des routes demeure un défi majeur. dre, ils existent plusieurs villages autochtones sur le Le personnel de la mission EUPOL RD Congo à Kinshasa, Dans les cités, des tornades de pluie font écouler des site. Léopoldville devient centre administratif du octobre 2008. maisons pendant chaque saison de pluie. Congo-Belge en 1929 (avant, c’était la ville de Boma « Kinshasa – the beauty and the beast »: Due to the de- sur la côte atlantique). La capitale devient Kinshasa en gradation of the economic situation and several lootings, 1966. / I n 1881, Henry Morton Stanley founds Leopold- EUPOL RDC et EUSEC RDC, ville, a settlement named after the Belgian King, owner the ancient elite’s quarters of Gombe, Ma Campagne in les deux missions PESD Ngaliema and some parts of Limete show nowadays a of the colony. The site is vast and easy to defend; there rather morbid charme. Rehabilitating Kinshasa’s roads en République Démocratique du Congo, are already several villages of natives in the area. Leo- rests a major challenge for the city’s development. In the vous souhaitent un bon séjour poldville is named administrative center of the Belgian- popular quarters, violent rain downpours bring down à Kinshasa. -

Praziquantel Mass Drug Administration Campaign for School-Aged Children in 3 Provinces of Angola November 2014. Provinces: Huamb
PRAZIQUANTEL MASS DRUG ADMINISTRATION CAMPAIGN FOR SCHOOL-AGED CHILDREN IN 3 PROVINCES OF ANGOLA NOVEMBER 2014. PROVINCES: HUAMBO, UÍGE E ZAIRE DISTRIBUTION CAMPAIGN FROM: 27 OCTOBER TO 08 NOVEMBER 2014 IMPLEMENTING PARTNERS: PROVINCIAL HEALTH DEPARTMENTS OF HUAMBO, UÍGE E ZAIRE PROVINCIAL EDUCATION DEPARTMENTS OF HUAMBO, UÍGE E ZAIRE THE MENTOR-INITIATIVE MUNICIPAL DEPARTMENTS OF HEALTH AND EDUCATION OF THE PROVINCES HUAMBO, UÍGE E ZAIRE. 1 JANUARY 2015 I. INTRODUCTION 3 II. PLANNING AND COORDINATION OF THE CAMPAIGN 4 III. SCHOOL-BASED TREATMENT CAMPAIGN PRAZIQUANTEL 7 1 - Methodology 7 2 – Distribution of the drugs 8 3- Treatment data collection and management 10 4- Results k10 IV. CHALLENGES 19 V. OPPORTUNITIES 20 VI. SUMMARY 21 2 I. INTRODUCTION The MENTOR Initiative is an international non-governmental organization dedicated to reducing death and suffering from malaria and neglected tropical diseases (NTDs) in humanitarian crises. Currently MENTOR is providing support to the most vulnerable communities in Angola, Liberia, Kenya, Central African Republic, South Sudan and Chad. The MENTOR is present in Angola since 2002, working with the National Malaria Control Program to reduce the burden of disease in the provinces of Huambo, Uíge and Zaire. Since 2011, MENTOR is implementing a private health sector malaria program in partnership with the Government and the NGO Population Services International (PSI), introducing combination therapies based on artemisinin (ACTs) and Rapid Diagnostic Tests (TDR) in private pharmacies. In partnership with the Government and the NGO World Learning, a public health malaria programme based on case management and capacity building within the National Health Structure is being implemented. In 2013, the MENTOR Initiative started the Neglected Tropical Disease control programme with the overall purpose to support the Ministry of Health of Angola to achieve a significant reduction in infections of Schistosomiasis, Soil Transmitted Helminths and Lymphatic Filariasis, in areas of high endemicity. -

WFP Angola Situation Report #01 July 2020 Received 312 Mt of Food Items (Maize Meal, Beans, Aged 6-23 Months in Selected Areas, WFP Angola Will Vegetable Oil)
WFP Angola In Numbers Situation Report July 2020 312 mt of food assistance distributed in July 2020 US$ 0 m cash-based transfers made US$ 1.87 m six-month net funding requirements 6,456 people assisted 51% 49% in July 2020 have been confirmed in the country. • The exceptional temporary measures introduced by Highlights the Government to prevent the spread of COVID-19 (mandatory use of masks, reduced working hours, • With an operational presence in Luanda, Dundo and border closures) have been prolonged until 07 Lóvua, WFP continues to work to ensure that September. refugees from Kasai are able to meet their basic food • Luanda and the municipality of Cazengo (Cuanza and nutrition requirements. Norte province) remain under a sanitary cordon. • At present, the capacities of the Government and Vehicles with humanitarian aid and food items are partners to maintain an integrated food security and allowed to enter. nutrition response are not yet significantly compromised by the COVID-19 pandemic. • WFP will maintain its focus on refugee response and the provision of technical assistance in the areas of WFP Response nutrition, supply chain management, vulnerability • WFP’s activities in Angola are defined by the Interim analysis and mapping (VAM), and emergency Country Strategic Plan 2020-2022. preparedness and response (EPR). • In coordination with the United Nations (UN) and • WFP COVID-19 Cargo Air Service has been non-governmental organizations (NGOs), WFP established between Luanda and Johannesburg. The started providing food assistance to refugees after first cargo for Angola has been dispatched to Luanda an official request for support from the Government on 28 July. -
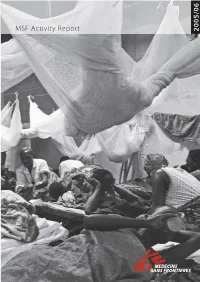
Activity Report Activity MSF
6 MSF International Office Rue de Lausanne 78, Case Postale 116, CH-1211 Geneva 21, Switzerland T (+41-22) 8498 400, F (+41-22) 8498 404, E [email protected], www.msf.org MSF Activity Report 2005/0 MSF Activity Repor t July 2005 – July 20 06 Médecins Sans Frontières (MSF) was founded in 1971 by a small group of doctors and journalists who believed that all people should have access to emergency relief. MSF was one of the first nongovernmental organisations to provide urgently needed medical assistance and to publicly bear witness to the plight of the people it helps. Today MSF is an international medical humanitarian movement with branch offices in 19 countries. In 2005, over 2225 MSF volunteer doctors, nurses, other medical professionals, logistical experts, water and sanitation engineers and administrators joined approximately 25,850 locally hired staff to provide medical aid in over 70 countries. MSF was awarded the 1999 Nobel Peace Prize. The Médecins Sans Frontières Charter About this publication FEATURE WRITERS Médecins Sans Frontières is a private international association. Nathalie Borremans, Leopold Buhendwa, Dieudonné Bwirire, Fabien Dubuet, Margaret Fitzgerald, The association is made up mainly of doctors and health C. Foncha, Moses Massaquoi, Marilyn McHarg, Dalitso Minsinde, Rodrick Nalingukgwi, Fasineh Samura, Milton Tectonidis, Emmanuel Tronc sector workers and is also open to all other professions which might help in achieving its aims. COUNTRY TEXT AND SIDEBAR MATERIAL WRITTEN BY Emma Bell, Claude Briade, Lucy Clayton, -

História E Variação Morfossintática
doi: http://dx.doi.org/10.5007/1984- 8412.2018v15n4 p 3289 HISTÓRIA E VARIAÇÃO MORFOSSINTÁTICA ENTRE O QUIMBUNDO E O PORTUGUÊS NA REGIÃO DE KWANZA NORTE, EM ANGOLA: FORMAÇÃO DO PLURAL, CONCORDÂNCIA DE GÊNERO E FORMAÇÃO DO DIMINUTIVO E DO AUMENTATIVO DOS SUBSTANTIVOS HISTORIA Y VARIACIÓN MORFOSINTÁCTICA ENTRE KIMBUNDU Y PORTUGUÉS EN LA REGIÓN DE KWANZA NORTE, EN ANGOLA: FORMACIÓN DEL PLURAL, CONCORDANCIA DE GÉNERO Y FORMACIÓN DEL DIMINUTIVO Y DEL AUMENTATIVO DE LOS SUSTANTIVOS HISTORY AND MORPHOSYNTACTIC VARIATION BETWEEN KIMBUNDU AND PORTUGUESE IN ANGOLA’S KWANZA NORTH PROVINCE: PLURAL FORMATION, GENDER AGREEMENT, AND AUGMENTATIVE AND DIMINUTIVE NOUN FORMATION João Lourenço António∗ Universidade da Beira Interior Paulo Osório∗∗ Universidade da Beira Interior RESUMO: A pesquisa aqui apresentada baseia-se no estudo da convivência entre duas línguas – quimbundo e português – no município de Cazengo-Ndalatando, uma província da região Kwanza Norte, em Angola. Uma observação sociolinguística do contato e uso simultâneo entre as duas línguas mostra claramente situações de interferência do quimbundo na língua portuguesa ∗ Mestre em Estudos Lusófonos pela Universidade da Beira Interior (Covilhã, Portugal). E- mail: <[email protected]>. ∗ ∗ Doutor, Pós- doutor, Professor com Agregação em Linguística Portuguesa. Professor Associado com Agregação na Universidade da Beira Interior (Covilhã, Portugal). E- mail: <[email protected]> . 3290 (língua oficial em Angola), o que é possível comprovar pela análise linguística de enunciados orais recolhidos diretamente na zona geográfica em questão e cujo juízo de aceitação linguística foi atestado por um dos autores deste trabalho, que é falante nativo de quimbundo. Neste artigo são, assim, analisados três fenômenos linguísticos de interferência do quimbundo no português, indicadores de variação morfossintática nos registros orais da língua portuguesa: formação do plural, concordância de gênero, além da formação do diminutivo e do aumentativo dos substantivos. -

Democratic Republic of Congo Round 7 – Service Delivery Point Questionnaire
Democratic Republic of Congo Round 7 – Service Delivery Point Questionnaire ◯ Yes 001a. Your ID: [NAME] Is this your ID? ◯ No 001b. Enter your ID below. Please record your ID Day: 002b. Record the correct date and time. Month: Year: ◯ KonGo Central 003a. Province ◯ KINSHASA ◯ BARUMBU ◯ BAS_FLEUVE ◯ BINZA_METEO ◯ BINZA_OZONE ◯ BIYELA ◯ BOMA ◯ BUMBU ◯ CATARACTES ◯ KALAMU_I ◯ KALAMU_II ◯ KIKIMI ◯ KIMBANSEKE ◯ KINGABWA ◯ KINGASANI ◯ KINSHASA 003b. District ◯ KINTAMBO ◯ KISENSO ◯ LEMBA ◯ LIMETE ◯ LINGWALA ◯ LUKAYA ◯ MASINA_I ◯ MASINA_II ◯ MATADI ◯ MATETE ◯ MONT_NGAFULA_I ◯ MONT_NGAFULA_II ◯ NGABA ◯ NGIRINGIRI ◯ SELEMBAO 1 ◯ BARUMBU ◯ BAS_FLEUVE ◯ BINZA_METEO ◯ BINZA_OZONE ◯ BIYELA ◯ BOMA ◯ BUMBU ◯ CATARACTES ◯ KALAMU_I ◯ KALAMU_II ◯ KIKIMI ◯ KIMBANSEKE ◯ KINGABWA ◯ KINGASANI ◯ KINSHASA 003b. Zone de Santé ◯ KINTAMBO ◯ KISENSO ◯ LEMBA ◯ LIMETE ◯ LINGWALA ◯ LUKAYA ◯ MASINA_I ◯ MASINA_II ◯ MATADI ◯ MATETE ◯ MONT_NGAFULA_I ◯ MONT_NGAFULA_II ◯ NGABA ◯ NGIRINGIRI ◯ SELEMBAO ◯ 17_MAI ◯ ASSOSSA_NGIRI_NGIRI ◯ BAKI_VILLE ◯ BAMBOMA ◯ BANA ◯ BANGU ◯ BETON ◯ BINZA_PIGEON 003c. Aire de Santé ◯ BITSHAKU_TSHAKU ◯ BOBA ◯ BUMBA ◯ BUNZI ◯ CAMP_PERMANENT ◯ CNECI ◯ CONGO ◯ CONGO_1 2 ◯ DIANGIENDA_I ◯ DINGI_DINGI ◯ ESSANGA ◯ HYGIENE_A ◯ IMBALI ◯ INGA ◯ KAPINGA ◯ KASAI_MASINA ◯ KASAI_BUMBU ◯ KAUKA_I ◯ KEMI ◯ KHAMI ◯ KHESA ◯ KIFUMA_NGIMBI ◯ KIKIMI ◯ KIMBANGU_A ◯ KIMBANZA ◯ KIMBATA___TUDI ◯ KIMBIANGA ◯ KIMBONDO1(_KINDELE) ◯ KIMUAKA ◯ KINGABWA ◯ KINKENGE ◯ KINSUKA_PECHEUR ◯ KINZAU_MVUE ◯ KIPASA ◯ KISANTU ◯ KISENSO_GARE ◯ KITOMESA ◯ KIVALA_TADI ◯ KIVEVE ◯ KIVUNDA ◯ KUMBI