Residency Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Once in a Lifetime Procedures Code List 2019 Effective: 11/14/2010
Policy Name: Once in a Lifetime Procedures Once in a Lifetime Procedures Code List 2019 Effective: 11/14/2010 Family Rhinectomy Code Description 30160 Rhinectomy; total Family Laryngectomy Code Description 31360 Laryngectomy; total, without radical neck dissection 31365 Laryngectomy; total, with radical neck dissection Family Pneumonectomy Code Description 32440 Removal of lung, pneumonectomy; Removal of lung, pneumonectomy; with resection of segment of trachea followed by 32442 broncho-tracheal anastomosis (sleeve pneumonectomy) 32445 Removal of lung, pneumonectomy; extrapleural Family Splenectomy Code Description 38100 Splenectomy; total (separate procedure) Splenectomy; total, en bloc for extensive disease, in conjunction with other procedure (List 38102 in addition to code for primary procedure) Family Glossectomy Code Description Glossectomy; complete or total, with or without tracheostomy, without radical neck 41140 dissection Glossectomy; complete or total, with or without tracheostomy, with unilateral radical neck 41145 dissection Family Uvulectomy Code Description 42140 Uvulectomy, excision of uvula Family Gastrectomy Code Description 43620 Gastrectomy, total; with esophagoenterostomy 43621 Gastrectomy, total; with Roux-en-Y reconstruction 43622 Gastrectomy, total; with formation of intestinal pouch, any type Family Colectomy Code Description 44150 Colectomy, total, abdominal, without proctectomy; with ileostomy or ileoproctostomy 44151 Colectomy, total, abdominal, without proctectomy; with continent ileostomy 44155 Colectomy, -

Approved Surgical Procedures
UNION MEDICAL BENEFITS SOCIETY LTD APPROVED SURGICAL PROCEDURES The following list of surgical procedures should be read in conjunction with your policy document. If you are intending to have one of the listed procedures, please call our surgical team on 0800 600 666 so we can guide you through the prior approval process. If a surgical procedure is not listed below, it will not be covered unless UniMed decides, in its sole discretion, to offer cover. CARDIAC GENERAL • Pericardiotomy Breast • Pericardiocentesis • Breast Cyst Aspiration or Needle Biopsy • Drainage of Pericaridal Effusion • Breast Biopsy • Coronary Artery Bypass (using vein or artery) • Core Biopsy of Breast • Open Repair of Atrial Septal Defect (ASD) • Excision Accessary Breast Tissue • Valvuloplasty • Mastectomy • Aortic/ Mitral Valve Replacement via Sternotomy • Sentinel Node Biopsy with/without Axillary Dissection • Pulmonary Valve Replacement via Sternotomy • Breast Microdochotomy • Tricuspid Valve Replacement via Sternotomy • Balloon Valvuloplasty – Mitral/ Aortic Reconstruction Post Mastectomy • Pacemaker Surgery – Initial Implantation (Excluding the Cost • Breast/ Nipple Reconstruction of the Pacemaker) • Nipple Areolar Tattoo • Removal of Sternal Wire • Maze Arrhythmia Surgery Gastrointestinal • Removal & Rewiring of Sternal Wire • Anal Sphincterotomy • Maze Arrhythmia Surgery (Standalone procedure) • Simple Repair of Anal Fistula – Special approval only • Maze Procedure – Thoracoscopic • Anal Fistula Repair with Mucosal Advancement Flap • Bentall’s Procedure (includes -
Procedure Codes Section 5
NEW YORK STATE MEDICAID PROGRAM PHYSICIAN – PROCEDURE CODES SECTION 5 - SURGERY Physician – Procedure Codes, Section 5 - Surgery _____________________________________________________________________________ Table of Contents ANESTHESIA SECTION------------------------------------------------------------------------2 GENERAL INFORMATION AND RULES------------------------------------------------2 CALCULATION OF TOTAL ANESTHESIA VALUES --------------------------------4 SURGERY SECTION ----------------------------------------------------------------------------5 GENERAL INFORMATION AND RULES------------------------------------------------5 SURGERY SERVICES ------------------------------------------------------------------------ 11 GENERAL -------------------------------------------------------------------------------------- 11 INTERGUMENTARY SYSTEM ----------------------------------------------------------- 11 MUSCULOSKELETAL SYSTEM--------------------------------------------------------- 38 RESPIRATORY SYSTEM ---------------------------------------------------------------- 108 CARDIOVASCULAR SYSTEM --------------------------------------------------------- 123 HEMIC AND LYMPHATIC SYSTEMS ------------------------------------------------ 167 MEDIASTINUM AND DIAPHRAGM --------------------------------------------------- 170 DIGESTIVE SYSTEM---------------------------------------------------------------------- 171 URINARY SYSTEM ------------------------------------------------------------------------ 214 MALE GENITAL SYSTEM --------------------------------------------------------------- -
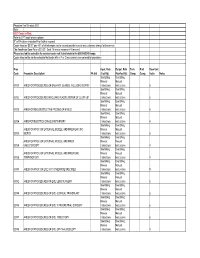
Physician Fee Schedule 2021 Note
Physician Fee Schedule 2021 Note: 2021 Codes in Red; Refer to CPT book for descriptions R" in PA column indicates Prior Auth is required Codes listed as '$0.00" pay 45% of billed amount not to exceed provider’s usual and customary charge for the service The Anesthesia Base Rate is $15.20. Each 15 minute increment=1 time unit. Please use lab fee schedule for covered codes not listed below in the 80000-89249 range. Codes listed on the lab fee schedule that begin with a P or Q are currently non-covered for physicians Proc Inpat. Rate Outpat. Rate Tech. Prof. Base Unit Code Procedure Description PA Ind (Facility) (NonFacility) Comp. Comp. Value Notes See Billing See Billing Manual Manual 00100 ANES FOR PROCEDURES ON SALIVARY GLANDS, INCLUDING BIOPSY Instructions Instructions 5 See Billing See Billing Manual Manual 00102 ANES FOR PROCEDURES INVOLVING PLASTIC REPAIR OF CLEFT LIP Instructions Instructions 6 See Billing See Billing Manual Manual 00103 ANES FOR RECONSTRUCTIVE PROCED OF EYELID Instructions Instructions 5 See Billing See Billing Manual Manual 00104 ANES FOR ELECTROCONVULSIVE THERAPY Instructions Instructions 4 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER EAR ,INC Manual Manual 00120 BIOPSY Instructions Instructions 5 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER Manual Manual 00124 EAR,OTOSCOPY Instructions Instructions 4 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER EAR, Manual Manual 00126 TYMPANOTOMY Instructions Instructions 4 See Billing See Billing Manual -

Correspondence Language Manual for Medicare Services
NATIONAL CORRECT CODING INITIATIVE CORRESPONDENCE LANGUAGE MANUAL FOR MEDICARE SERVICES Effective February 28, 2021 Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2020 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors, prospective payment systems, and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. Page 1 of 42 Medicare – Effective 02/28/2021 Table of Contents Introduction ..................................................................................................................... 3 National Correct Coding Initiative General Correspondence Language Policies ............. 6 National Correct Coding Initiative Medicare Correspondence Language Section-Specific Examples ...................................................................................................................... 11 Anesthesia Services CPT Codes 00000-09999 ......................................................... 11 Integumentary System CPT Codes 10000-19999 ..................................................... 13 Musculoskeletal System CPT Codes 20000-29999 .................................................. -

Map Prior Authorization List Eff: 3/1/2021
MAP PRIOR AUTHORIZATION LIST EFF: 3/1/2021 (Updated 02/18/2021) CPT, HCPCS or Revenue Description Comment Note Code INPATIENT All Inpatient admissions require authorization 0100 All inclusive room and board plus ancillary 0101 All inclusive room and board 0110 Room and Board Private (one bed) 0111 Room and Board Private (one bed) - Medical/Surgical/GYN 0113 Room and Board Private (one bed) - Pediatric 0117 Room and Board Private (one bed) - Oncology 0119 Room and Board Private (one bed) - Other 0121 Room and Board Semiprivate (two beds) - Medical/Surgical/GYN 0123 Room and Board Semiprivate (two beds) - Pediatric 0127 Room and Board Semiprivate (two beds) - Oncology 0130 Room & Board - Three and Four Beds General Classification 0131 Room & Board - Three and Four Beds Medical/Surgical/Gyn 0133 Room & Board - Three and Four Beds Pediatric 0137 Room & Board - Three and Four Beds Oncology 0139 Room & Board - Three and Four Beds Other 0140 Room & Board - Deluxe Private General Classification 0141 Room & Board - Deluxe Private Medical/Surgical/Gyn 0143 Room & Board - Deluxe Private Pediatric 0147 Room & Board - Deluxe Private Oncology 0149 Room & Board - Deluxe Private Other 0150 Room & Board - Ward General Classification 0151 Room & Board - Ward Medical/Surgical/Gyn 0153 Room & Board - Ward Pediatric 0157 Room & Board - Ward Oncology 0159 Room & Board - Ward Other 0160 Room & Board - Other General Classification 0164 Other Room & Board - Sterile Environment 0167 Room & Board - Other Self Care 0169 Room & Board - Other Other 00170 Anesthesia -

Prioritization of Health Services
PRIORITIZATION OF HEALTH SERVICES A Report to the Governor and the 77 th Oregon Legislative Assembly Health Evidence Review Commission Office for Oregon Health Policy and Research Oregon Health Authority 2013 TABLE OF CONTENTS List of Figures . iv Health Evidence Review Commission and Staff . .v Acknowledgments . .vi Executive Summary . vii CHAPTER ONE: PRIORITIZATION OF HEALTH SERVICES FOR 2014-15 Charge to the Health Evidence Review Commission . 2 Prioritization Methodology . 3 Biennial Review of the Prioritized List . 6 Interim Modifications to the Prioritized List . 19 Technical Changes . 20 Advancements in Medical Technology . 26 Prioritization of Medications and Other Ancillary Services . .. 28 Therapies With Marginal Benefit Or High Cost . 29 CHAPTER TWO: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES Practice Guidelines . 32 Guidelines on Ancillary and Diagnostic Services Not Appearing on the Prioritized List . .32 Advanced Imaging For Low Back Pain . .. 33 Breast Cancer Screening . 35 Neuroimaging For Headache . 36 Neuroimaging in Dementia . .. 36 Non-Prenatal Genetic Testing . .. 37 Guideline Notes For Health Services That Appear On The Prioritized List . .42 Acne Conglobata. 42 Acromioclavicular Joint Sprain, Management of . 42 Acupuncture. 42 Acute Viral Infections, Hospitalization for . 43 Artificial Disk Replacement . 45 Bariatric Surgery. 46 Benign Neoplasm Of Urinary Organs, Treatment Of. .47 Blepharoplasty. .48 Bone Tumors, Benign . .48 Breast Reconstruction. .48 Cataract. 48 Cesarean Delivery, Planned. .49 Chemodenervation of the Bladder. .49 Cognitive Rehabilitation. .49 Collapsed Vertebra. .50 Dental Services Basic Peridontics. .. 51 Frenulectomy/Frenulotomy. 51 Oral Surgery. .52 Posterior Composite Restorations, One Surface (Deleted). 52 Preventive Dental Care. 52 Removeable Prosthodontics. 52 Silver Compounds For Dental Caries. 53 Dysmenorrhea. -

Understanding Head and Neck Cancers
Understanding Head and Neck Cancers A guide for people with cancer, their families and friends Understanding Head and Neck Cancers A guide for people with cancer, their families and friends First published July 2008; Abridged February 2010 © The Cancer Council New South Wales 2010; ISBN 978 1 921041 72 3 Acknowledgements We thank the Cancer Institute NSW for their support and acknowledge the NSW Oncology Group (NSWOG) Head & Neck for their clinical review of the original edition of this booklet: Dr G Morgan, Surgeon; C Baxter, Senior Speech Pathologist; C Bullivant, NSWOG Project Officer; J Dahlstrom, Anatomical Pathologist; L Dall’Armi, Cancer Nurse Coordinator; M Findlay, Senior Oncology Dietitian; Dr D Forstner, Radiation Oncologist; Dr A Goldrick, Medical Oncologist; R Hield, Consumer; Dr J Hill, Radiation Oncologist; M Nutt, Nurse Care Coordinator; K Pronk, Senior Oncology Dietitian; T Simpson, Social Worker; Dr C Wratten, Chairman and Director, Radiation Oncology; and Dr SC Yeoh, Staff specialist, Oral Medicine & Pathology. We also thank the additional reviewers: K Chapman, Nutrition Program Manager, Cancer Council NSW; Dr J Clark, Head of Fellowship, Sydney Head & Neck Cancer Institute; B & C Gardner, Laryngectomee Association of NSW; C Julien, Clinical Nurse Consultant; A Moloney, Cancer Nurse Coordinator. We acknowledge Dr K Shannon, Chairman, Cancer Institute NSW Oncology Group (NSWOG) Head & Neck, for approving this abridged booklet. Cancer Council NSW wishes to acknowledge Cancer Council Victoria for kindly permitting its resource Cancers of the Mouth, Nose and Throat to be used as the main source for this booklet, and for the adaptation of its illustrations on pages 4-5. -

Prioritization of Health Services
PRIORITIZATION OF HEALTH SERVICES A Report to the Governor and the 74th Oregon Legislative Assembly Oregon Health Services Commission Office for Oregon Health Policy and Research Department of Administrative Services 2007 TABLE OF CONTENTS List of Figures . iii Health Services Commission and Staff . .v Acknowledgments . .vii Executive Summary . ix CHAPTER ONE: A HISTORY OF HEALTH SERVICES PRIORITIZATION UNDER THE OREGON HEALTH PLAN Enabling Legislatiion . 3 Early Prioritization Efforts . 3 Gaining Waiver Approval . 5 Impact . 6 CHAPTER TWO: PRIORITIZATION OF HEALTH SERVICES FOR 2008-09 Charge to the Health Services Commission . .. 25 Biennial Review of the Prioritized List . 26 A New Prioritization Methodology . 26 Public Input . 36 Next Steps . 36 Interim Modifications to the Prioritized List . 37 Technical Changes . 38 Advancements in Medical Technology . .42 CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES Practice Guidelines . 47 Age-Related Macular Degeneration (AMD) . 47 Chronic Anal Fissure . 48 Comfort Care . 48 Complicated Hernias . 49 Diagnostic Services Not Appearing on the Prioritized List . 49 Non-Prenatal Genetic Testing . 49 Tuberculosis Blood Test . 51 Early Childhood Mental Health . 52 Adjustment Reactions In Early Childhood . 52 Attention Deficit and Hyperactivity Disorders in Early Childhood . 53 Disruptive Behavior Disorders In Early Childhood . 54 Mental Health Problems In Early Childhood Related To Neglect Or Abuse . 54 Mood Disorders in Early Childhood . 55 Erythropoietin . 55 Mastocytosis . 56 Obesity . 56 Bariatric Surgery . 56 Non-Surgical Management of Obesity . 58 PET Scans . 58 Prenatal Screening for Down Syndrome . 59 Prophylactic Breast Removal . 59 Psoriasis . 59 Reabilitative Therapies . 60 i TABLE OF CONTENTS (Cont’d) CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES (CONT’D) Practice Guidelines (Cont’d) Sinus Surgery . -

Master Precertification List
0f MASTER PRECERTIFICATION LIST For Health Care Providers Effective October 2021, Last updated September 24, 2021 Complete/PHS+ - The most comprehensive care management model that includes all the components of our Preferred level, plus additional digital tools and the highest level of engagement and potential savings. Preferred - A comprehensive care management model that includes all the components of our existing care management model, including comprehensive outpatient precertification, plus higher intensity of care coordination and more customer engagement opportunities. Basic Standard - A lower touch care management model that includes many of the components of our existing care management model, such as higher intensity of care coordination and more customer engagement opportunities. Basic Standard has a limited number of outpatient precertification categories (radiation therapy, medical oncology, medical injectables, home infusion therapy and private duty nursing), fewer than our Preferred and Complete solutions. *Removal from precertification is not a guarantee of payment. Codes may be subject to code editing, benefit plan exclusions and post-service review for coverage. Complete /PHS+/ Basic Code Code Description Addition/Removal Preferred Standard Precertification delegated to eviCore Revenue Radiology-Therapeutic and/or Chemotherapy Administration- healthcare National Code 0333 Radiation Therapy Radiation Therapy X X Program; Added 02/27/2016 Revenue Cell/Gene Therapy - General Classification Added 04/01/2019 Code 0870 X X Revenue Cell/Gene Therapy - Cell Collection Added 04/01/2019 Code 0871 X X Revenue Cell/Gene Therapy - Specialized Biologic Processing And Added 04/01/2019 Code 0872 Storage - Prior To Transport X X All Cigna products and services are provided exclusively by or through operating subsidiaries of Cigna Corporation, including Cigna Health and Life Insurance Company and Express Scripts, Inc. -

Head and Neck Surgery (OHNS) (List of Core Privileges) I CORE PRIVILEGE Training and Experience Requirements for Initial Privileging: 1
7/21/2020 www.ucsfmedicalcenter.org/medstaffoffice/privilege_form.asp?LINK=18874 Department of Otolaryngology - Head And Neck Surgery (OHNS) (List of Core Privileges) I CORE PRIVILEGE Training and Experience Requirements for Initial Privileging: 1. Board-Certified or eligible for Board Certification. Initial / FPPE: 1. The Chair is responsible for selecting a proctor or proctors to evaluate the individual’s performance in the operating room and prepare a written report describing the type of cases observed. 2. If unsatisfactory, the reason(s) will be stated. 3. A minimum of five (5) cases will be proctored,which reflect the spectrum of the core procedures unless prior arrangements for performance of other surgical procedures have been made with the Chair. Maintenance / Reappointment: 1. A minimum of five (5) cases per year reflecting the spectrum of the core procedures unless prior arrangements for performance of other surgical procedures have been made with the Chair. II ORTHOGNATHIC SURGERY Orthognathic surgery privileges include: midface and mandibular sliding osteotomies for the treatment of sleep apnea. Training and Experience Requirements for Initial Privileging: 1. Board-Certified or eligible for Board Certification. A. Completion of additional training no less than six (6) months in duration with an experience in maxillomandibular advancement to treat obstructive sleep apnea (OSA) that includes direct involvement with a minimum of twenty (20) surgical cases. B. Sufficient background and training demonstrated by surgical experience of at least ten (10) cases. Initial / FPPE: 1. The Chair is responsible for selecting a proctor or proctors to evaluate the individual’s performance in the operating room and prepare a written report describing the type of cases observed. -

UNDERSTANDING HEAD and NECK CANCERS SEP 2021 CAN1161 Understanding Head and Neck Cancers a Guide for People with Cancer, Their Families and Friends
UNDERSTANDING HEAD AND NECK CANCERS HEAD AND NECK UNDERSTANDING CANCER TYPE Understanding Head and Neck Cancers A guide for people with cancer, their families and friends SEP 2021 CAN1161 For information & support, call 13 11 20 Understanding Head and Neck Cancers A guide for people with cancer, their families and friends First published July 2008. This edition September 2021. © Cancer Council Australia 2021. ISBN 978 0 6489506 1 5 Understanding Head and Neck Cancers is reviewed approximately every two years. Check the publication date above to ensure this copy is up to date. Editor: Jenni Bruce. Designer: Eleonora Pelosi. Printer: SOS Print + Media Group. Acknowledgements This edition has been developed by Cancer Council NSW on behalf of all other state and territory Cancer Councils as part of a National Cancer Information Subcommittee initiative. We thank the reviewers of this booklet: A/Prof Richard Gallagher, Head and Neck Surgeon, Director of Cancer Services and Head and Neck Cancer Services, St Vincent’s Health Network, NSW; Dr Sophie Beaumont, Head of Dental Oncology, Dental Practitioner, Peter MacCallum Cancer Centre, VIC; Dr Bena Brown, Speech Pathologist, Princess Alexandra Hospital, and Senior Research Fellow, Menzies School of Health Research, QLD; Dr Teresa Brown, Assistant Director, Nutrition and Dietetics, Royal Brisbane and Women’s Hospital, QLD; Lisa Castle-Burns, Head and Neck Cancer Specialist Nurse, Canberra Region Cancer Centre, The Canberra Hospital, ACT; A/Prof Ben Chua, Radiation Oncologist, Royal Brisbane and Women’s