Calponin and Cytoskeleton Dynamics in Macrophage Functions and the Ap Thogenesis of Atherosclerosis Rong Liu Wayne State University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic and Genomic Analysis of Hyperlipidemia, Obesity and Diabetes Using (C57BL/6J × TALLYHO/Jngj) F2 Mice
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Nutrition Publications and Other Works Nutrition 12-19-2010 Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P. Stewart Marshall University Hyoung Y. Kim University of Tennessee - Knoxville, [email protected] Arnold M. Saxton University of Tennessee - Knoxville, [email protected] Jung H. Kim Marshall University Follow this and additional works at: https://trace.tennessee.edu/utk_nutrpubs Part of the Animal Sciences Commons, and the Nutrition Commons Recommended Citation BMC Genomics 2010, 11:713 doi:10.1186/1471-2164-11-713 This Article is brought to you for free and open access by the Nutrition at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Nutrition Publications and Other Works by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. Stewart et al. BMC Genomics 2010, 11:713 http://www.biomedcentral.com/1471-2164/11/713 RESEARCH ARTICLE Open Access Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P Stewart1, Hyoung Yon Kim2, Arnold M Saxton3, Jung Han Kim1* Abstract Background: Type 2 diabetes (T2D) is the most common form of diabetes in humans and is closely associated with dyslipidemia and obesity that magnifies the mortality and morbidity related to T2D. The genetic contribution to human T2D and related metabolic disorders is evident, and mostly follows polygenic inheritance. The TALLYHO/ JngJ (TH) mice are a polygenic model for T2D characterized by obesity, hyperinsulinemia, impaired glucose uptake and tolerance, hyperlipidemia, and hyperglycemia. -

S41467-020-18249-3.Pdf
ARTICLE https://doi.org/10.1038/s41467-020-18249-3 OPEN Pharmacologically reversible zonation-dependent endothelial cell transcriptomic changes with neurodegenerative disease associations in the aged brain Lei Zhao1,2,17, Zhongqi Li 1,2,17, Joaquim S. L. Vong2,3,17, Xinyi Chen1,2, Hei-Ming Lai1,2,4,5,6, Leo Y. C. Yan1,2, Junzhe Huang1,2, Samuel K. H. Sy1,2,7, Xiaoyu Tian 8, Yu Huang 8, Ho Yin Edwin Chan5,9, Hon-Cheong So6,8, ✉ ✉ Wai-Lung Ng 10, Yamei Tang11, Wei-Jye Lin12,13, Vincent C. T. Mok1,5,6,14,15 &HoKo 1,2,4,5,6,8,14,16 1234567890():,; The molecular signatures of cells in the brain have been revealed in unprecedented detail, yet the ageing-associated genome-wide expression changes that may contribute to neurovas- cular dysfunction in neurodegenerative diseases remain elusive. Here, we report zonation- dependent transcriptomic changes in aged mouse brain endothelial cells (ECs), which pro- minently implicate altered immune/cytokine signaling in ECs of all vascular segments, and functional changes impacting the blood–brain barrier (BBB) and glucose/energy metabolism especially in capillary ECs (capECs). An overrepresentation of Alzheimer disease (AD) GWAS genes is evident among the human orthologs of the differentially expressed genes of aged capECs, while comparative analysis revealed a subset of concordantly downregulated, functionally important genes in human AD brains. Treatment with exenatide, a glucagon-like peptide-1 receptor agonist, strongly reverses aged mouse brain EC transcriptomic changes and BBB leakage, with associated attenuation of microglial priming. We thus revealed tran- scriptomic alterations underlying brain EC ageing that are complex yet pharmacologically reversible. -

Expression of Smooth Muscle and Extracellular Matrix Proteins in Relation to Airway Function in Asthma
Expression of smooth muscle and extracellular matrix proteins in relation to airway function in asthma Annelies M. Slats, MD,a Kirsten Janssen, BHe,a Annemarie van Schadewijk, MSc,a Dirk T. van der Plas, BSc,a Robert Schot, BSc,a Joost G. van den Aardweg, MD, PhD,b Johan C. de Jongste, MD, PhD,c Pieter S. Hiemstra, PhD,a Thais Mauad, MD,d Klaus F. Rabe, MD, PhD,a and Peter J. Sterk, MD, PhDa,e Leiden, Alkmaar, Rotterdam, and Amsterdam, The Netherlands, and Sa˜o Paulo, Brazil Background: Smooth muscle content is increased within the selective expression of airway smooth muscle proteins and airway wall in patients with asthma and is likely to play a role in components of the extracellular matrix. (J Allergy Clin airway hyperresponsiveness. However, smooth muscle cells Immunol 2008;121:1196-202.) express several contractile and structural proteins, and each of these proteins may influence airway function distinctly. Key words: Actin, desmin, elastin, airway smooth muscle, extracel- Objective: We examined the expression of contractile and lular matrix, lung function, hyperresponsiveness, deep inspiration- structural proteins of smooth muscle cells, as well as induced bronchodilation, bronchial biopsies extracellular matrix proteins, in bronchial biopsies of patients with asthma, and related these to lung function, airway hyperresponsiveness, and responses to deep inspiration. Asthma is characterized by chronic airway inflammation, Methods: Thirteen patients with asthma (mild persistent, which is presumed to contribute to variable airways obstruction 1 atopic, nonsmoking) participated in this cross-sectional study. and bronchial hyperresponsiveness. However, recent studies FEV1% predicted, PC20 methacholine, and resistance of the have led to a reappraisal of the role of airway smooth muscle in 2 respiratory system by the forced oscillation technique during asthma pathophysiology. -
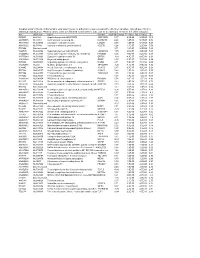
Supplementary File 2A Revised
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06 -
Expression Profiling the Developing Mammalian Enteric Nervous System Identifies Marker and Candidate Hirschsprung Disease Genes
Expression profiling the developing mammalian enteric nervous system identifies marker and candidate Hirschsprung disease genes Tiffany A. Heanue and Vassilis Pachnis* Division of Molecular Neurobiology, National Institute for Medical Research, Medical Research Council, The Ridgeway, Mill Hill, London NW7 1AA, United Kingdom Communicated by Shirley M. Tilghman, Princeton University, Princeton, NJ, March 16, 2006 (received for review January 19, 2006) The enteric nervous system (ENS) is composed of neurons and glial eration, differentiation, and axonogenesis within the ENS (11–13). cells, organized as interconnected ganglia within the gut wall, How Ret signaling regulates these diverse cellular responses re- which controls persistalsis of the gut wall and secretions from its quired for normal ENS development is not understood. glands. The Ret receptor tyrosine kinase is expressed throughout HSCR occurs relatively frequently in the human population enteric neurogenesis and is required for normal ENS development; (1:5,000 live births). Mutations in RET and the Endothelin receptor humans with mutations in the RET locus have Hirschsprung disease type B (EDNRB) account for 50% and 5% of familial HSCR cases, (HSCR, an absence of ganglia in the colon), and mice lacking Ret respectively. Mutations in a number of other genes account for a have total intestinal aganglionosis. The Ret mutant mouse pro- further small percentage of HSCR cases, including the Ret ligands vides a tool for identifying genes implicated in development of the GDNF and NTN, the EDNRB ligand EDN3, the EDN3-converting ENS. By using RNA from WT and Ret mutant (aganglionic) gut tissue enzyme ECE1, SOX10, PHOX2B, and ZFHX1B (7). Additional and DNA microarrays, we have conducted a differential screen for susceptibility loci have been identified, although the corresponding ENS-expressed genes and have identified hundreds of candidate genes have yet to be determined (7). -

Characterizing Iqgap1-C Domain Binding to Phosphoinositides
CHARACTERIZING IQGAP1-C DOMAIN BINDING TO PHOSPHOINOSITIDES A Major Qualifying Project Report Submitted to the Faculty of WORCESTER POLYTECHNIC INSTITUTE In partial fulfillment of the requirements for the Degree of Bachelor of Science in Biochemistry Written by: Approved by: __________________ . Christopher Dallarosa Dr. Arne Gericke Date: April 2018 Table of Contents Acknowledgments........................................................................................................................... 3 Abstract ........................................................................................................................................... 4 Introduction ..................................................................................................................................... 5 Background ..................................................................................................................................... 6 History ......................................................................................................................................... 6 Scaffolding Proteins .................................................................................................................... 6 IQGAP Protein Family ................................................................................................................ 8 IQGAPs in Yeast Cells ............................................................................................................ 8 Mammalian IQGAPs ............................................................................................................. -

Supplemental Figure Legends Figure S1. Expression of Mir-133A
Supplemental Figure legends Figure S1. Expression of miR-133a and miR-1 in adult mice. (A) Expression of miR-133a in heart samples of miR-133a-1-KO and miR-133a-2-KO adult mice as detected by real-time PCR. Expression level of miR-133a in mutant hearts were normalized to GAPDH and compared to WT hearts. N=3 for each genotype group. (B) Northern blot analysis of heart and skeletal muscle RNA from adult mice. Ten micrograms of RNA from skeletal muscle and heart tissues were used in the Northern blots. 32P-labeled Start-Fire probes for miR-133a and miR-1 were used. Genotypes of mice are labeled on top. U6 probe was used as a loading control. GP, gastrocnemius- plantaris. (C) Expression of Mib1 mRNA and protein in dKO mice at P1. mRNA level of Mib1 as detected by real-time PCR in dKO hearts were normalized to GAPDH and compared to WT hearts. Error bars indicate SEM. Western blot analysis was performed on hearts from P1 wild type and dKO mutant mice. α -tubulin was detected as a loading control. Figure S2. Abnormal cardiomyocyte proliferation in miR-133a dKO hearts. Representative images of proliferating cardiomyocytes in WT and dKO hearts at P1. High magnification of immunohistochemistry on heart sections at P1 using phospho- histone H3 (PH3, red) and -actinin (green) was shown. Bar = 20 m. Figure S3. Expression of miR-133a in wild-type and beta-MHC-miR-133a transgenic hearts at E13.5 as detected by real-time PCR. Figure S4. Expression of miR-133a target genes in hearts of WT and dKO mutant mice at P1. -

Snapshot: Actin Regulators II Anosha D
SnapShot: Actin Regulators II Anosha D. Siripala and Matthew D. Welch Department of Molecular and Cell Biology, University of California, Berkeley, CA 94720, USA Representative Proteins Protein Family H. sapiens D. melanogaster C. elegans A. thaliana S. cerevisiae Endocytosis and Exocytosis ABP1/drebrin mABP1, drebrin, drebrin- †Q95RN0 †Q9XUT0 Abp1 like EPS15 EPS15 Eps-15 EHS-1 †Q56WL2 Pan1 HIP1R HIP1R †Q8MQK1 †O62142 Sla2 Synapsin synapsin Ia, Ib, IIa, IIb, III Synapsin SNN-1 Plasma Membrane Association Anillin anillin Scraps ANI-1, 2, 3 Annexins annexin A1–11, 13 (actin Annexin B9-11 NEX-1–4 ANN1-8 binding: 1, 2, 6) ERM proteins ezrin, radixin, moesin DMoesin ERM-1 MARCKS MARCKS, MRP/ Akap200 MACMARCKS/F52 Merlin *merlin/NF2 Merlin NFM-1 Protein 4.1 4.1R, G, N, B Coracle Spectrin α-spectrin (1–2), β-spectrin α-spectrin, β-spectrin, β heavy- SPC-1 (α-spectrin), UNC-70 (1–4), β heavy-spectrin/ spectrin/Karst (β-spectrin), SMA-1 (β heavy- karst spectrin) Identifi ed Cellular Role: X Membrane traffi cking and phagocytosis Cell-Cell Junctions X Cytokinesis α-catenin α-catenin 1–3 α-catenin HMP-1 X Cell surface organization and dynamics X Cell adhesion Afadin afadin/AF6 Canoe AFD-1 X Multiple functions ZO-1 ZO-1, ZO-2, ZO-3 ZO-1/Polychaetoid †Q56VX4 X Other/unknown Cell-Extracellular Matrix Junctions †UNIPROT database accession number *Mutation linked to human disease Dystrophin/utrophin *dystrophin, utrophin/ Dystrophin DYS-1 DRP1, DRP2 LASP LASP-1, LASP-2, LIM- Lasp †P34416 nebulette Palladin palladin Parvin α-, β-, χ-parvin †Q9VWD0 PAT-6 -

Differential Expression of Drosophila Transgelins Throughout Development
fcell-09-648568 July 6, 2021 Time: 18:30 # 1 ORIGINAL RESEARCH published: 12 July 2021 doi: 10.3389/fcell.2021.648568 Differential Expression of Drosophila Transgelins Throughout Development Katerina M. Vakaloglou1†, Maria Mouratidou1†, Athina Keramidioti1,2 and Christos G. Zervas1* 1 Center of Basic Research, Biomedical Research Foundation, Academy of Athens, Athens, Greece, 2 Department of Biochemistry and Biotechnology, University of Thessaly, Larissa, Greece Transgelins are a conserved family of actin-binding proteins involved in cytoskeletal remodeling, cell contractility, and cell shape. In both mammals and Drosophila, three genes encode transgelin proteins. Transgelins exhibit a broad and overlapping expression pattern, which has obscured the precise identification of their role in development. Here, we report the first systematic developmental analysis of all Drosophila transgelin proteins, namely, Mp20, CG5023, and Chd64 in the Edited by: living organism. Drosophila transgelins display overall higher sequence identity with Lei-Miao Yin, mammalian TAGLN-3 and TAGLN-2 than with TAGLN. Detailed examination in different Shanghai University of Traditional Chinese Medicine, China developmental stages revealed that Mp20 and CG5023 are predominantly expressed in Reviewed by: mesodermal tissues with the onset of myogenesis and accumulate in the cytoplasm Cedric Soler, of all somatic muscles and heart in the late embryo. Notably, at postembryonic Clermont Université, France Simone Diestel, developmental stages, Mp20 and CG5023 are detected in the gut’s circumferential University of Bonn, Germany muscles with distinct subcellular localization: Z-lines for Mp20 and sarcomere and Rajesh Gunage, nucleus for CG5023. Only CG5023 is strongly detected in the adult fly in the abdominal, Boston Children’s Hospital, United States leg, and synchronous thoracic muscles. -

Role of IQGAP1 in Carcinogenesis
cancers Review Role of IQGAP1 in Carcinogenesis Tao Wei and Paul F. Lambert * McArdle Laboratory for Cancer Research, Department of Oncology, University of Wisconsin School of Medicine and Public Health, Madison, WI 53705, USA; [email protected] * Correspondence: [email protected] Simple Summary: IQ motif-containing GTPase-activating protein 1 (IQGAP1) is a signal scaffolding protein that regulates a range of cellular activities by facilitating signal transduction in cells. IQGAP1 is involved in many cancer-related activities, such as proliferation, apoptosis, migration, invasion and metastases. In this article, we review the different pathways regulated by IQGAP1 during cancer development, and the role of IQGAP1 in different types of cancer, including cancers of the head and neck, breast, pancreas, liver, colorectal, stomach, and ovary. We also discuss IQGAP10s regulation of the immune system, which is of importance to cancer progression. This review highlights the significant roles of IQGAP1 in cancer and provides a rationale for pursuing IQGAP1 as a drug target for developing novel cancer therapies. Abstract: Scaffolding proteins can play important roles in cell signaling transduction. IQ motif- containing GTPase-activating protein 1 (IQGAP1) influences many cellular activities by scaffolding multiple key signaling pathways, including ones involved in carcinogenesis. Two decades of studies provide evidence that IQGAP1 plays an essential role in promoting cancer development. IQGAP1 is overexpressed in many types of cancer, and its overexpression in cancer is associated with lower survival of the cancer patient. Here, we provide a comprehensive review of the literature regarding the oncogenic roles of IQGAP1. We start by describing the major cancer-related signaling pathways Citation: Wei, T.; Lambert, P.F. -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

A Study of Calponin's Role in Secretion
WORCESTER POLYTECHNIC INSTITUTE A Study of Calponin’s Role in Secretion The Proposed Model and the Experimental Design Christopher T. Rollins 4/30/2009 A Major Qualifying Project Report Submitted to the Faculty of the WORCESTER POLYTECHNIC INSTITUTE in partial fulfillment of the requirements for the Degree of Bachelor of Science in Biology and Biotechnology Approved: Jill Rulfs – Advisor Keywords: Actin, Cytoskeleton, Calponin, CaP, CN , Secretion , Exocytosis 1 A Study of Calponin’s R ole in Secretion Table of Contents Abstract .................................................................................................................................................. 2 Background ............................................................................................................................................. 2 Introduction ............................................................................................................................................ 6 Secretion Study – Model, Hypothesis, and Experiments ................................................................... 7 Materials and Methods ........................................................................................................................ 11 Amplification of pET, pCMV-HA, and GFP-Calponin Vectors ........................................................... 11 Creation of DH5α and XL-10 Gold Calcium Competent Cells ........................................................... 11 Transformation of Calcium Competent Cells ..................................................................................