S41467-020-18249-3.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dedifferentiation by Adenovirus E1A Due to Inactivation of Hippo Pathway Effectors YAP and TAZ
Downloaded from genesdev.cshlp.org on October 3, 2021 - Published by Cold Spring Harbor Laboratory Press Dedifferentiation by adenovirus E1A due to inactivation of Hippo pathway effectors YAP and TAZ Nathan R. Zemke, Dawei Gou, and Arnold J. Berk Molecular Biology Institute, University of California at Los Angeles, Los Angeles, California 90095, USA Adenovirus transformed cells have a dedifferentiated phenotype. Eliminating E1A in transformed human embryonic kidney cells derepressed ∼2600 genes, generating a gene expression profile closely resembling mesenchymal stem cells (MSCs). This was associated with a dramatic change in cell morphology from one with scant cytoplasm and a globular nucleus to one with increased cytoplasm, extensive actin stress fibers, and actomyosin-dependent flat- tening against the substratum. E1A-induced hypoacetylation at histone H3 Lys27 and Lys18 (H3K27/18) was reversed. Most of the increase in H3K27/18ac was in enhancers near TEAD transcription factors bound by Hippo signaling-regulated coactivators YAP and TAZ. E1A causes YAP/TAZ cytoplasmic sequestration. After eliminating E1A, YAP/TAZ were transported into nuclei, where they associated with poised enhancers with DNA-bound TEAD4 and H3K4me1. This activation of YAP/TAZ required RHO family GTPase signaling and caused histone acetylation by p300/CBP, chromatin remodeling, and cohesin loading to establish MSC-associated enhancers and then superenhancers. Consistent results were also observed in primary rat embryo kidney cells, human fibroblasts, and human respiratory tract epithelial cells. These results together with earlier studies suggest that YAP/TAZ function in a developmental checkpoint controlled by signaling from the actin cytoskeleton that prevents differ- entiation of a progenitor cell until it is in the correct cellular and tissue environment. -

Establishing the Pathogenicity of Novel Mitochondrial DNA Sequence Variations: a Cell and Molecular Biology Approach
Mafalda Rita Avó Bacalhau Establishing the Pathogenicity of Novel Mitochondrial DNA Sequence Variations: a Cell and Molecular Biology Approach Tese de doutoramento do Programa de Doutoramento em Ciências da Saúde, ramo de Ciências Biomédicas, orientada pela Professora Doutora Maria Manuela Monteiro Grazina e co-orientada pelo Professor Doutor Henrique Manuel Paixão dos Santos Girão e pela Professora Doutora Lee-Jun C. Wong e apresentada à Faculdade de Medicina da Universidade de Coimbra Julho 2017 Faculty of Medicine Establishing the pathogenicity of novel mitochondrial DNA sequence variations: a cell and molecular biology approach Mafalda Rita Avó Bacalhau Tese de doutoramento do programa em Ciências da Saúde, ramo de Ciências Biomédicas, realizada sob a orientação científica da Professora Doutora Maria Manuela Monteiro Grazina; e co-orientação do Professor Doutor Henrique Manuel Paixão dos Santos Girão e da Professora Doutora Lee-Jun C. Wong, apresentada à Faculdade de Medicina da Universidade de Coimbra. Julho, 2017 Copyright© Mafalda Bacalhau e Manuela Grazina, 2017 Esta cópia da tese é fornecida na condição de que quem a consulta reconhece que os direitos de autor são pertença do autor da tese e do orientador científico e que nenhuma citação ou informação obtida a partir dela pode ser publicada sem a referência apropriada e autorização. This copy of the thesis has been supplied on the condition that anyone who consults it recognizes that its copyright belongs to its author and scientific supervisor and that no quotation from the -

Regulation of Cdc42 and Its Effectors in Epithelial Morphogenesis Franck Pichaud1,2,*, Rhian F
© 2019. Published by The Company of Biologists Ltd | Journal of Cell Science (2019) 132, jcs217869. doi:10.1242/jcs.217869 REVIEW SUBJECT COLLECTION: ADHESION Regulation of Cdc42 and its effectors in epithelial morphogenesis Franck Pichaud1,2,*, Rhian F. Walther1 and Francisca Nunes de Almeida1 ABSTRACT An overview of Cdc42 Cdc42 – a member of the small Rho GTPase family – regulates cell Cdc42 was discovered in yeast and belongs to a large family of small – polarity across organisms from yeast to humans. It is an essential (20 30 kDa) GTP-binding proteins (Adams et al., 1990; Johnson regulator of polarized morphogenesis in epithelial cells, through and Pringle, 1990). It is part of the Ras-homologous Rho subfamily coordination of apical membrane morphogenesis, lumen formation and of GTPases, of which there are 20 members in humans, including junction maturation. In parallel, work in yeast and Caenorhabditis elegans the RhoA and Rac GTPases, (Hall, 2012). Rho, Rac and Cdc42 has provided important clues as to how this molecular switch can homologues are found in all eukaryotes, except for plants, which do generate and regulate polarity through localized activation or inhibition, not have a clear homologue for Cdc42. Together, the function of and cytoskeleton regulation. Recent studies have revealed how Rho GTPases influences most, if not all, cellular processes. important and complex these regulations can be during epithelial In the early 1990s, seminal work from Alan Hall and his morphogenesis. This complexity is mirrored by the fact that Cdc42 can collaborators identified Rho, Rac and Cdc42 as main regulators of exert its function through many effector proteins. -

Stelios Pavlidis3, Matthew Loza3, Fred Baribaud3, Anthony
Supplementary Data Th2 and non-Th2 molecular phenotypes of asthma using sputum transcriptomics in UBIOPRED Chih-Hsi Scott Kuo1.2, Stelios Pavlidis3, Matthew Loza3, Fred Baribaud3, Anthony Rowe3, Iaonnis Pandis2, Ana Sousa4, Julie Corfield5, Ratko Djukanovic6, Rene 7 7 8 2 1† Lutter , Peter J. Sterk , Charles Auffray , Yike Guo , Ian M. Adcock & Kian Fan 1†* # Chung on behalf of the U-BIOPRED consortium project team 1Airways Disease, National Heart & Lung Institute, Imperial College London, & Biomedical Research Unit, Biomedical Research Unit, Royal Brompton & Harefield NHS Trust, London, United Kingdom; 2Department of Computing & Data Science Institute, Imperial College London, United Kingdom; 3Janssen Research and Development, High Wycombe, Buckinghamshire, United Kingdom; 4Respiratory Therapeutic Unit, GSK, Stockley Park, United Kingdom; 5AstraZeneca R&D Molndal, Sweden and Areteva R&D, Nottingham, United Kingdom; 6Faculty of Medicine, Southampton University, Southampton, United Kingdom; 7Faculty of Medicine, University of Amsterdam, Amsterdam, Netherlands; 8European Institute for Systems Biology and Medicine, CNRS-ENS-UCBL, Université de Lyon, France. †Contributed equally #Consortium project team members are listed under Supplementary 1 Materials *To whom correspondence should be addressed: [email protected] 2 List of the U-BIOPRED Consortium project team members Uruj Hoda & Christos Rossios, Airways Disease, National Heart & Lung Institute, Imperial College London, UK & Biomedical Research Unit, Biomedical Research Unit, Royal -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Hypopituitarism May Be an Additional Feature of SIM1 and POU3F2 Containing 6Q16 Deletions in Children with Early Onset Obesity
Open Access Journal of Pediatric Endocrinology Case Report Hypopituitarism may be an Additional Feature of SIM1 and POU3F2 Containing 6q16 Deletions in Children with Early Onset Obesity Rutteman B1, De Rademaeker M2, Gies I1, Van den Bogaert A2, Zeevaert R1, Vanbesien J1 and De Abstract Schepper J1* Over the past decades, 6q16 deletions have become recognized as a 1Department of Pediatric Endocrinology, UZ Brussel, frequent cause of the Prader-Willi-like syndrome. Involvement of SIM1 in the Belgium deletion has been linked to the development of obesity. Although SIM1 together 2Department of Genetics, UZ Brussel, Belgium with POU3F2, which is located close to the SIM1 locus, are involved in pituitary *Corresponding author: De Schepper J, Department development and function, pituitary dysfunction has not been reported frequently of Pediatric Endocrinology, UZ Brussel, Belgium in cases of 6q16.1q16.3 deletion involving both genes. Here we report on a case of a girl with typical Prader-Willi-like symptoms including early-onset Received: December 23, 2016; Accepted: February 21, hyperphagic obesity, hypotonia, short hands and feet and neuro-psychomotor 2017; Published: February 22, 2017 development delay. Furthermore, she suffered from central diabetes insipidus, central hypothyroidism and hypocortisolism. Her genetic defect is a 6q16.1q16.3 deletion, including SIM1 and POU3F2. We recommend searching for a 6q16 deletion in children with early onset hyperphagic obesity associated with biological signs of hypopituitarism and/or polyuria-polydipsia syndrome. The finding of a combined SIM1 and POU3F2 deletion should prompt monitoring for the development of hypopituitarism, if not already present at diagnosis. Keywords: 6q16 deletion; SIM1; POU3F2; Prader-Willi-like syndrome; Hypopituitarism Introduction insipidus and of some specific pituitary hormone deficiencies in children with a combined SIM1 and POU3F2 deficiency. -

Datasheet: VPA00673 Product Details
Datasheet: VPA00673 Description: RABBIT ANTI ATP5D Specificity: ATP5D Format: Purified Product Type: PrecisionAb™ Polyclonal Isotype: Polyclonal IgG Quantity: 100 µl Product Details Applications This product has been reported to work in the following applications. This information is derived from testing within our laboratories, peer-reviewed publications or personal communications from the originators. Please refer to references indicated for further information. For general protocol recommendations, please visit www.bio-rad-antibodies.com/protocols. Yes No Not Determined Suggested Dilution Western Blotting 1/1000 PrecisionAb antibodies have been extensively validated for the western blot application. The antibody has been validated at the suggested dilution. Where this product has not been tested for use in a particular technique this does not necessarily exclude its use in such procedures. Further optimization may be required dependant on sample type. Target Species Human Species Cross Reacts with: Mouse Reactivity N.B. Antibody reactivity and working conditions may vary between species. Product Form Purified IgG - liquid Preparation Rabbit polyclonal antibody purified by affinity chromatography Buffer Solution Phosphate buffered saline Preservative 0.09% Sodium Azide Stabilisers 2% Sucrose Immunogen Synthetic peptide encompassing part of the middle region of human ATP5D External Database Links UniProt: P30049 Related reagents Entrez Gene: 513 ATP5D Related reagents Specificity Rabbit anti Human ATP5D antibody recognizes ATP synthase subunit delta, mitochondrial, also known as ATP synthase subunit delta mitochondrial, F-ATPase delta subunit, mitochondrial ATP Page 1 of 2 synthase complex delta-subunit precusor, or mitochondrial ATP synthase, delta subunit. ATP5D gene encodes a subunit of mitochondrial ATP synthase. Mitochondrial ATP synthase catalyzes ATP synthesis, utilizing an electrochemical gradient of protons across the inner membrane during oxidative phosphorylation. -
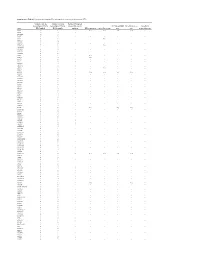
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Genome-Wide Association Study for Circulating Fibroblast Growth Factor
www.nature.com/scientificreports OPEN Genome‑wide association study for circulating fbroblast growth factor 21 and 23 Gwo‑Tsann Chuang1,2,14, Pi‑Hua Liu3,4,14, Tsui‑Wei Chyan5, Chen‑Hao Huang5, Yu‑Yao Huang4,6, Chia‑Hung Lin4,7, Jou‑Wei Lin8, Chih‑Neng Hsu8, Ru‑Yi Tsai8, Meng‑Lun Hsieh9, Hsiao‑Lin Lee9, Wei‑shun Yang2,9, Cassianne Robinson‑Cohen10, Chia‑Ni Hsiung11, Chen‑Yang Shen12,13 & Yi‑Cheng Chang2,9,12* Fibroblast growth factors (FGFs) 21 and 23 are recently identifed hormones regulating metabolism of glucose, lipid, phosphate and vitamin D. Here we conducted a genome‑wide association study (GWAS) for circulating FGF21 and FGF23 concentrations to identify their genetic determinants. We enrolled 5,000 participants from Taiwan Biobank for this GWAS. After excluding participants with diabetes mellitus and quality control, association of single nucleotide polymorphisms (SNPs) with log‑transformed FGF21 and FGF23 serum concentrations adjusted for age, sex and principal components of ancestry were analyzed. A second model additionally adjusted for body mass index (BMI) and a third model additionally adjusted for BMI and estimated glomerular fltration rate (eGFR) were used. A total of 4,201 participants underwent GWAS analysis. rs67327215, located within RGS6 (a gene involved in fatty acid synthesis), and two other SNPs (rs12565114 and rs9520257, located between PHC2-ZSCAN20 and ARGLU1-FAM155A respectively) showed suggestive associations with serum FGF21 level (P = 6.66 × 10–7, 6.00 × 10–7 and 6.11 × 10–7 respectively). The SNPs rs17111495 and rs17843626 were signifcantly associated with FGF23 level, with the former near PCSK9 gene and the latter near HLA-DQA1 gene (P = 1.04 × 10–10 and 1.80 × 10–8 respectively). -

High-Grade Glioneuronal Tumor with an ARHGEF2–NTRK1 Fusion Gene
Brain Tumor Pathology (2019) 36:121–128 https://doi.org/10.1007/s10014-019-00345-y CASE REPORT High‑grade glioneuronal tumor with an ARHGEF2–NTRK1 fusion gene Kazuhiko Kurozumi1 · Yoshiko Nakano2 · Joji Ishida1 · Takehiro Tanaka3 · Masatomo Doi4 · Junko Hirato5 · Akihiko Yoshida6 · Kana Washio7 · Akira Shimada7 · Takashi Kohno8 · Koichi Ichimura2 · Hiroyuki Yanai9 · Isao Date1 Received: 1 March 2019 / Accepted: 20 March 2019 / Published online: 22 April 2019 © The Japan Society of Brain Tumor Pathology 2019 Abstract Here, we report a highly unusual case of high-grade glioneuronal tumor with a neurotrophic tropomyosin receptor kinase (NTRK) fusion gene. A 13-year-old girl presented with headache and vomiting and MRI detected two cystic lesions bilaterally in the frontal areas with surrounding edema. The left larger tumor was removed by left frontal craniotomy. The tumor was diagnosed as a high-grade glioneuronal tumor, unclassifed. Methylation profling classifed it as a difuse leptomeningeal glioneuronal tumor (DLGNT) with low confdence. This tumor showed genotypes frequently found in DLGNT such as 1p/19q codeletion without IDH mutation and, however, did not have the typical DLGNT clinical and histological features. RNA sequencing identifed an ARHGEF2 (encoding Rho/Rac guanine nucleotide exchange factor 2)–NTRK1 fusion gene. The presence of recurrent NTRK fusion in glioneuronal tumors has an important implication in the clinical decision making and opens up a possibility of novel targeted therapy. Keywords Pediatric brain tumor · 1p19qLOH · RNA sequencing · NTRK1 Introduction diagnosis of glioneuronal tumors has been sometimes chal- lenging. However, unique molecular signatures have recently Mixed glioneuronal tumors are rare group of brain tumors been identifed, enabling creation of classifcation schemes that consist of glial and neuronal components. -

A Single-Cell Transcriptomic Landscape of Primate Arterial Aging
ARTICLE https://doi.org/10.1038/s41467-020-15997-0 OPEN A single-cell transcriptomic landscape of primate arterial aging Weiqi Zhang 1,2,3,4,5,13, Shu Zhang6,7,13, Pengze Yan3,8,13, Jie Ren7,9,13, Moshi Song3,5,8, Jingyi Li2,3,8, Jinghui Lei4, Huize Pan2,3, Si Wang3,5,8, Xibo Ma3,10, Shuai Ma2,3,8, Hongyu Li2,3, Fei Sun2,3, Haifeng Wan3,5,11, ✉ ✉ ✉ Wei Li 3,5,11, Piu Chan4, Qi Zhou3,5,11, Guang-Hui Liu 2,3,4,5,8 , Fuchou Tang 6,7,9,12 & Jing Qu 3,5,11 Our understanding of how aging affects the cellular and molecular components of the vas- 1234567890():,; culature and contributes to cardiovascular diseases is still limited. Here we report a single-cell transcriptomic survey of aortas and coronary arteries in young and old cynomolgus monkeys. Our data define the molecular signatures of specialized arteries and identify eight markers discriminating aortic and coronary vasculatures. Gene network analyses characterize tran- scriptional landmarks that regulate vascular senility and position FOXO3A, a longevity- associated transcription factor, as a master regulator gene that is downregulated in six subtypes of monkey vascular cells during aging. Targeted inactivation of FOXO3A in human vascular endothelial cells recapitulates the major phenotypic defects observed in aged monkey arteries, verifying FOXO3A loss as a key driver for arterial endothelial aging. Our study provides a critical resource for understanding the principles underlying primate arterial aging and contributes important clues to future treatment of age-associated vascular disorders. 1 CAS Key Laboratory of Genomic and Precision Medicine, Beijing Institute of Genomics, Chinese Academy of Sciences, Beijing 100101, China. -

Controls Homeostatic Splicing of ARGLU1 Mrna Stephan P
Published online 28 November 2016 Nucleic Acids Research, 2017, Vol. 45, No. 6 3473–3486 doi: 10.1093/nar/gkw1140 An Ultraconserved Element (UCE) controls homeostatic splicing of ARGLU1 mRNA Stephan P. Pirnie, Ahmad Osman, Yinzhou Zhu and Gordon G. Carmichael* Department of Genetics and Genome Sciences, UCONN Health Center, 400 Farmington Avenue, Farmington, CT 06030, USA Received January 13, 2016; Revised October 25, 2016; Editorial Decision October 28, 2016; Accepted October 31, 2016 ABSTRACT or inhibit the usage of a particular splice site (1,2). The ex- pression of trans-acting factors in a developmental and tis- Arginine and Glutamate-Rich protein 1 (ARGLU1) is sue specific manner results in regulated splicing that isof- a protein whose function is poorly understood, but ten cell specific. Most notably, trans-acting proteins such as may act in both transcription and pre-mRNA splicing. the NOVA (3–6), the RBFOX (7) and SR protein (8–11) We demonstrate that the ARGLU1 gene expresses families, and a number of hnRNP (12,13) proteins compete at least three distinct RNA splice isoforms – a fully to bind nascent RNAs at specific motifs and drive regula- spliced isoform coding for the protein, an isoform tion of alternative splicing in a tissue and developmentally containing a retained intron that is detained in the specific manner. Alternative splicing is an important pro- nucleus, and an isoform containing an alternative cess that is seen in at least 95% of multi-exon genes in the exon that targets the transcript for nonsense medi- human transcriptome (14). Furthermore, alternative splic- ated decay.