Establishing the Pathogenicity of Novel Mitochondrial DNA Sequence Variations: a Cell and Molecular Biology Approach
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Frontiers in Integrative Genomics and Translational Bioinformatics
BioMed Research International Frontiers in Integrative Genomics and Translational Bioinformatics Guest Editors: Zhongming Zhao, Victor X. Jin, Yufei Huang, Chittibabu Guda, and Jianhua Ruan Frontiers in Integrative Genomics and Translational Bioinformatics BioMed Research International Frontiers in Integrative Genomics and Translational Bioinformatics Guest Editors: Zhongming Zhao, Victor X. Jin, Yufei Huang, Chittibabu Guda, and Jianhua Ruan Copyright © òýÔ Hindawi Publishing Corporation. All rights reserved. is is a special issue published in “BioMed Research International.” All articles are open access articles distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Contents Frontiers in Integrative Genomics and Translational Bioinformatics, Zhongming Zhao, Victor X. Jin, Yufei Huang, Chittibabu Guda, and Jianhua Ruan Volume òýÔ , Article ID Þò ¥ÀÔ, ç pages Building Integrated Ontological Knowledge Structures with Ecient Approximation Algorithms, Yang Xiang and Sarath Chandra Janga Volume òýÔ , Article ID ýÔ ò, Ô¥ pages Predicting Drug-Target Interactions via Within-Score and Between-Score, Jian-Yu Shi, Zun Liu, Hui Yu, and Yong-Jun Li Volume òýÔ , Article ID ç ýÀç, À pages RNAseq by Total RNA Library Identies Additional RNAs Compared to Poly(A) RNA Library, Yan Guo, Shilin Zhao, Quanhu Sheng, Mingsheng Guo, Brian Lehmann, Jennifer Pietenpol, David C. Samuels, and Yu Shyr Volume òýÔ , Article ID âòÔçý, À pages Construction of Pancreatic Cancer Classier Based on SVM Optimized by Improved FOA, Huiyan Jiang, Di Zhao, Ruiping Zheng, and Xiaoqi Ma Volume òýÔ , Article ID ÞÔýòç, Ôò pages OperomeDB: A Database of Condition-Specic Transcription Units in Prokaryotic Genomes, Kashish Chetal and Sarath Chandra Janga Volume òýÔ , Article ID çÔòÔÞ, Ôý pages How to Choose In Vitro Systems to Predict In Vivo Drug Clearance: A System Pharmacology Perspective, Lei Wang, ChienWei Chiang, Hong Liang, Hengyi Wu, Weixing Feng, Sara K. -

Efficacy and Mechanistic Evaluation of Tic10, a Novel Antitumor Agent
University of Pennsylvania ScholarlyCommons Publicly Accessible Penn Dissertations 2012 Efficacy and Mechanisticv E aluation of Tic10, A Novel Antitumor Agent Joshua Edward Allen University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/edissertations Part of the Oncology Commons Recommended Citation Allen, Joshua Edward, "Efficacy and Mechanisticv E aluation of Tic10, A Novel Antitumor Agent" (2012). Publicly Accessible Penn Dissertations. 488. https://repository.upenn.edu/edissertations/488 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/edissertations/488 For more information, please contact [email protected]. Efficacy and Mechanisticv E aluation of Tic10, A Novel Antitumor Agent Abstract TNF-related apoptosis-inducing ligand (TRAIL; Apo2L) is an endogenous protein that selectively induces apoptosis in cancer cells and is a critical effector in the immune surveillance of cancer. Recombinant TRAIL and TRAIL-agonist antibodies are in clinical trials for the treatment of solid malignancies due to the cancer-specific cytotoxicity of TRAIL. Recombinant TRAIL has a short serum half-life and both recombinant TRAIL and TRAIL receptor agonist antibodies have a limited capacity to perfuse to tissue compartments such as the brain, limiting their efficacy in certain malignancies. To overcome such limitations, we searched for small molecules capable of inducing the TRAIL gene using a high throughput luciferase reporter gene assay. We selected TRAIL-inducing compound 10 (TIC10) for further study based on its induction of TRAIL at the cell surface and its promising therapeutic index. TIC10 is a potent, stable, and orally active antitumor agent that crosses the blood-brain barrier and transcriptionally induces TRAIL and TRAIL-mediated cell death in a p53-independent manner. -

Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 T + is online at: average * The Journal of Immunology , 34 of which you can access for free at: 2016; 197:1477-1488; Prepublished online 1 July from submission to initial decision 4 weeks from acceptance to publication 2016; doi: 10.4049/jimmunol.1600589 http://www.jimmunol.org/content/197/4/1477 Molecular Profile of Tumor-Specific CD8 Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. Waugh, Sonia M. Leach, Brandon L. Moore, Tullia C. Bruno, Jonathan D. Buhrman and Jill E. Slansky J Immunol cites 95 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2016/07/01/jimmunol.160058 9.DCSupplemental This article http://www.jimmunol.org/content/197/4/1477.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 25, 2021. The Journal of Immunology Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. -

Studies of Mitochondrial Dysfunction in Models of Rett Syndrome
Studies of Mitochondrial Dysfunction in Models of Rett Syndrome by Natalya O. Shulyakova A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Department of Physiology University of Toronto © Copyright by Natalya O. Shulyakova 2016 Studies of Mitochondrial Dysfunction in Models of Rett Syndrome Natalya O. Shulyakova Doctor of Philosophy Department of Physiology University of Toronto 2016 Abstract Rett syndrome (RTT) is a neurodevelopmental disorder affecting primarily females that is predominantly caused by mutations in the MECP2 gene. RTT is characterized by a loss of previously acquired skills, ambulatory deficits, respiratory problems and overall retarded growth. Mitochondrial dysfunction and oxidative stress identified in MeCP2-deficient tissues raised the possibility that mitochondrial impairments may play role in the pathogenesis of RTT. To further investigate the role of mitochondrial dysfunction in the absence of MeCP2, I analyzed mitochondrial function and morphology in Mecp2-deficient mouse adult skin fibroblasts (ASF) and in Mecp2-null mouse ESC derived neurons using an array of fluorescent dyes coupled with flow cytometry and confocal microscopy. The heterogeneity of cellular responses in ASF prevented identification of consistent changes in mitochondrial function, making them an unsuitable model for studying mitochondrial dysfunctions. Mecp2-null mouse ESC were differentiated into enriched population of neurons. Mecp2-null neurons displayed hyperpolarized mitochondria, high levels of ROS, low ATP and impaired mitochondrial trafficking. Resveratrol and mitochondrial cocktail that target expression of mitochondrial genes and mitochondrial metabolism, but not simple ROS scavengers, were successful at ameliorating ROS levels and normalizing mitochondrial membrane potential. Since oxidative stress was reported in RTT ii mice, I tested whether resveratrol and mitochondrial cocktail could reverse or improve behavioral phenotype in RTT mice. -

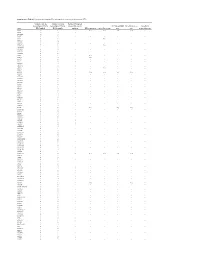
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Stelios Pavlidis3, Matthew Loza3, Fred Baribaud3, Anthony
Supplementary Data Th2 and non-Th2 molecular phenotypes of asthma using sputum transcriptomics in UBIOPRED Chih-Hsi Scott Kuo1.2, Stelios Pavlidis3, Matthew Loza3, Fred Baribaud3, Anthony Rowe3, Iaonnis Pandis2, Ana Sousa4, Julie Corfield5, Ratko Djukanovic6, Rene 7 7 8 2 1† Lutter , Peter J. Sterk , Charles Auffray , Yike Guo , Ian M. Adcock & Kian Fan 1†* # Chung on behalf of the U-BIOPRED consortium project team 1Airways Disease, National Heart & Lung Institute, Imperial College London, & Biomedical Research Unit, Biomedical Research Unit, Royal Brompton & Harefield NHS Trust, London, United Kingdom; 2Department of Computing & Data Science Institute, Imperial College London, United Kingdom; 3Janssen Research and Development, High Wycombe, Buckinghamshire, United Kingdom; 4Respiratory Therapeutic Unit, GSK, Stockley Park, United Kingdom; 5AstraZeneca R&D Molndal, Sweden and Areteva R&D, Nottingham, United Kingdom; 6Faculty of Medicine, Southampton University, Southampton, United Kingdom; 7Faculty of Medicine, University of Amsterdam, Amsterdam, Netherlands; 8European Institute for Systems Biology and Medicine, CNRS-ENS-UCBL, Université de Lyon, France. †Contributed equally #Consortium project team members are listed under Supplementary 1 Materials *To whom correspondence should be addressed: [email protected] 2 List of the U-BIOPRED Consortium project team members Uruj Hoda & Christos Rossios, Airways Disease, National Heart & Lung Institute, Imperial College London, UK & Biomedical Research Unit, Biomedical Research Unit, Royal -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Genes in a Refined Smith-Magenis Syndrome Critical Deletion Interval on Chromosome 17P11.2 and the Syntenic Region of the Mouse
Downloaded from genome.cshlp.org on September 25, 2021 - Published by Cold Spring Harbor Laboratory Press Article Genes in a Refined Smith-Magenis Syndrome Critical Deletion Interval on Chromosome 17p11.2 and the Syntenic Region of the Mouse Weimin Bi,1,6 Jiong Yan,1,6 Paweł Stankiewicz,1 Sung-Sup Park,1,7 Katherina Walz,1 Cornelius F. Boerkoel,1 Lorraine Potocki,1,3 Lisa G. Shaffer,1 Koen Devriendt,4 Małgorzata J.M. Nowaczyk,5 Ken Inoue,1 and James R. Lupski1,2,3,8 Departments of 1Molecular & Human Genetics, 2Pediatrics, Baylor College of Medicine, 3Texas Children’s Hospital, Houston, Texas 77030, USA; 4Centre for Human Genetics, University Hospital Gasthuisberg, Catholic University of Leuven, B-3000 Leuven, Belgium; 5Department of Pathology and Molecular Medicine, McMaster University, Hamilton, Ontario L8S 4J9, Canada Smith-Magenis syndrome (SMS) is a multiple congenital anomaly/mental retardation syndrome associated with behavioral abnormalities and sleep disturbance. Most patients have the same ∼4 Mb interstitial genomic deletion within chromosome 17p11.2. To investigate the molecular bases of the SMS phenotype, we constructed BAC/PAC contigs covering the SMS common deletion interval and its syntenic region on mouse chromosome 11. Comparative genome analysis reveals the absence of all three ∼200-kb SMS-REP low-copy repeats in the mouse and indicates that the evolution of SMS-REPs was accompanied by transposition of adjacent genes. Physical and genetic map comparisons in humans reveal reduced recombination in both sexes. Moreover, by examining the deleted regions in SMS patients with unusual-sized deletions, we refined the minimal Smith-Magenis critical region (SMCR) to an ∼1.1-Mb genomic interval that is syntenic to an ∼1.0-Mb region in the mouse. -
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Mapping the Genetic Architecture of Gene Regulation in Whole Blood
Mapping the Genetic Architecture of Gene Regulation in Whole Blood Katharina Schramm1,2., Carola Marzi3,4,5., Claudia Schurmann6., Maren Carstensen7,8., Eva Reinmaa9,10, Reiner Biffar11, Gertrud Eckstein1, Christian Gieger12, Hans-Jo¨ rgen Grabe13, Georg Homuth6, Gabriele Kastenmu¨ ller14, Reedik Ma¨gi10, Andres Metspalu9,10, Evelin Mihailov10,15, Annette Peters2, Astrid Petersmann16, Michael Roden7,8,17, Konstantin Strauch12,18, Karsten Suhre14,19, Alexander Teumer6,UweVo¨ lker6, Henry Vo¨ lzke20, Rui Wang-Sattler3,4, Melanie Waldenberger3,4, Thomas Meitinger1,2,21, Thomas Illig22, Christian Herder7,8., Harald Grallert3,4,5., Holger Prokisch1,2*. 1 Institute of Human Genetics, Helmholtz Center Munich, German Research Center for Environmental Health, Neuherberg, Germany, 2 Institute of Human Genetics, Technical University Munich, Mu¨nchen, Germany, 3 Research Unit of Molecular Epidemiology, Helmholtz Center Munich, German Research Center for Environmental Health, Neuherberg, Germany, 4 Institute of Epidemiology II, Helmholtz Center Munich, German Research Center for Environmental Health, Neuherberg, Germany, 5 German Center for Diabetes Research (DZD e.V.), Neuherberg, Germany, 6 Interfaculty Institute for Genetics and Functional Genomics, Department of Functional Genomics, University Medicine Greifswald, Greifswald, Germany, 7 Institute for Clinical Diabetology, German Diabetes Center, Leibniz Center for Diabetes Research at Heinrich Heine University Du¨sseldorf, Du¨sseldorf, Germany, 8 German Center for Diabetes Research (DZD e.V.), -

Mitochondrial Reprogramming Via ATP5H Loss Promotes Multimodal Cancer Therapy Resistance
Mitochondrial reprogramming via ATP5H loss promotes multimodal cancer therapy resistance Kwon-Ho Song, … , T.C. Wu, Tae Woo Kim J Clin Invest. 2018;128(9):4098-4114. https://doi.org/10.1172/JCI96804. Research Article Immunology Oncology The host immune system plays a pivotal role in the emergence of tumor cells that are refractory to multiple clinical interventions including immunotherapy, chemotherapy, and radiotherapy. Here, we examined the molecular mechanisms by which the immune system triggers cross-resistance to these interventions. By examining the biological changes in murine and tumor cells subjected to sequential rounds of in vitro or in vivo immune selection via cognate cytotoxic T lymphocytes, we found that multimodality resistance arises through a core metabolic reprogramming pathway instigated by epigenetic loss of the ATP synthase subunit ATP5H, which leads to ROS accumulation and HIF-1α stabilization under normoxia. Furthermore, this pathway confers to tumor cells a stem-like and invasive phenotype. In vivo delivery of antioxidants reverses these phenotypic changes and resensitizes tumor cells to therapy. ATP5H loss in the tumor is strongly linked to failure of therapy, disease progression, and poor survival in patients with cancer. Collectively, our results reveal a mechanism underlying immune-driven multimodality resistance to cancer therapy and demonstrate that rational targeting of mitochondrial metabolic reprogramming in tumor cells may overcome this resistance. We believe these results hold important implications for the clinical management of cancer. Find the latest version: https://jci.me/96804/pdf RESEARCH ARTICLE The Journal of Clinical Investigation Mitochondrial reprogramming via ATP5H loss promotes multimodal cancer therapy resistance Kwon-Ho Song,1,2,3 Jae-Hoon Kim,4 Young-Ho Lee,1,2,3 Hyun Cheol Bae,5 Hyo-Jung Lee,1,2,3 Seon Rang Woo,1,2,3 Se Jin Oh,1,2,3 Kyung-Mi Lee,1,2 Cassian Yee,6 Bo Wook Kim,7 Hanbyoul Cho,4 Eun Joo Chung,8 Joon-Yong Chung,9 Stephen M. -

ATP5H Antibody (Center) Affinity Purified Rabbit Polyclonal Antibody (Pab) Catalog # AW5527
10320 Camino Santa Fe, Suite G San Diego, CA 92121 Tel: 858.875.1900 Fax: 858.622.0609 ATP5H Antibody (Center) Affinity Purified Rabbit Polyclonal Antibody (Pab) Catalog # AW5527 Specification ATP5H Antibody (Center) - Product Information Application WB, IHC-P, FC,E Primary Accession O75947 Reactivity Human Host Rabbit Clonality Polyclonal Calculated MW H=18;M=19;R=19 KDa Isotype Rabbit Ig Antigen Source HUMAN ATP5H Antibody (Center) - Additional Information Gene ID 10476 Antigen Region 68-97 All lanes : Anti-ATP5H Antibody (Center) at 1:1000 dilution Lane 1: MDA-MB-453 whole Other Names cell lysate Lane 2: HepG2 whole cell lysate ATP synthase subunit d, mitochondrial, Lysates/proteins at 20 µg per lane. ATPase subunit d, ATP5H Secondary Goat Anti-Rabbit IgG, (H+L), Peroxidase conjugated at 1/10000 dilution. Dilution Predicted band size : 18 kDa WB~~1:1000 Blocking/Dilution buffer: 5% NFDM/TBST. IHC-P~~1:50~100 FC~~1:10~50 Target/Specificity This ATP5H antibody is generated from rabbits immunized with a KLH conjugated synthetic peptide between 68-97 amino acids from the Central region of human ATP5H. Storage Maintain refrigerated at 2-8°C for up to 2 weeks. For long term storage store at -20°C in small aliquots to prevent freeze-thaw cycles. Precautions ATP5H Antibody (Center) is for research use only and not for use in diagnostic or therapeutic procedures. ATP5H antibody (Center) (Cat. #AW5527) immunohistochemistry analysis in formalin fixed and paraffin embedded human brain Page 1/3 10320 Camino Santa Fe, Suite G San Diego, CA 92121 Tel: 858.875.1900 Fax: 858.622.0609 ATP5H Antibody (Center) - Protein Information tissue followed by peroxidase conjugation of the secondary antibody and DAB staining.